Analysis of the difference of therapeutic effect and predictive factors between postural and non-postural OSA after modified uvulopalatopharyngoplasty
-
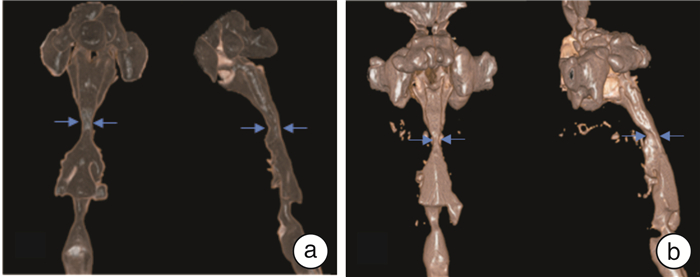
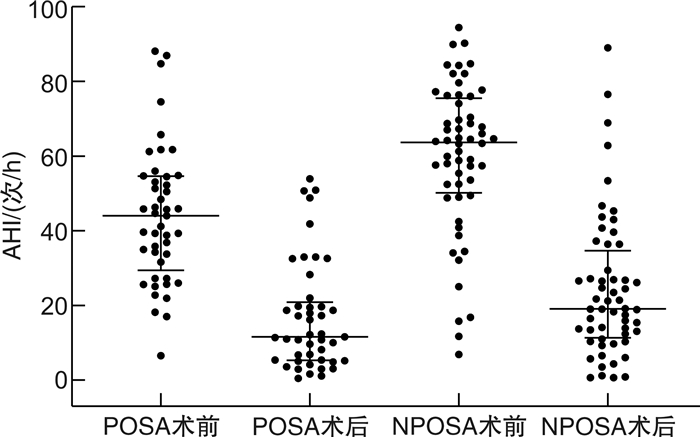
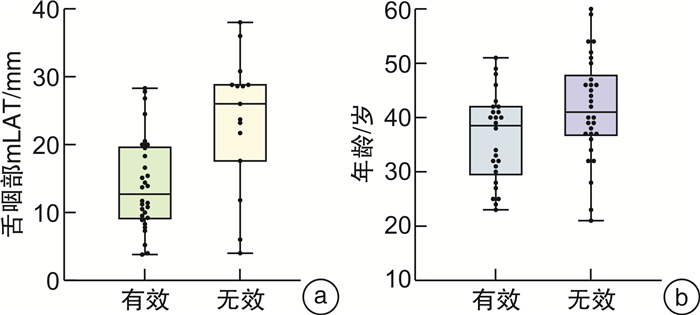
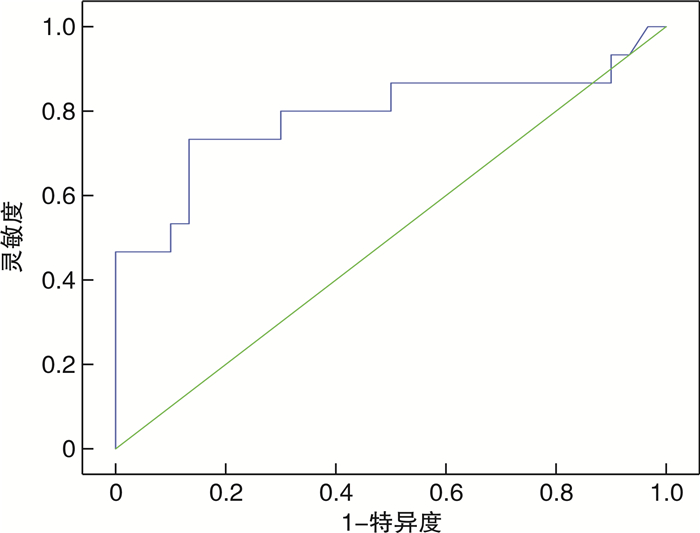
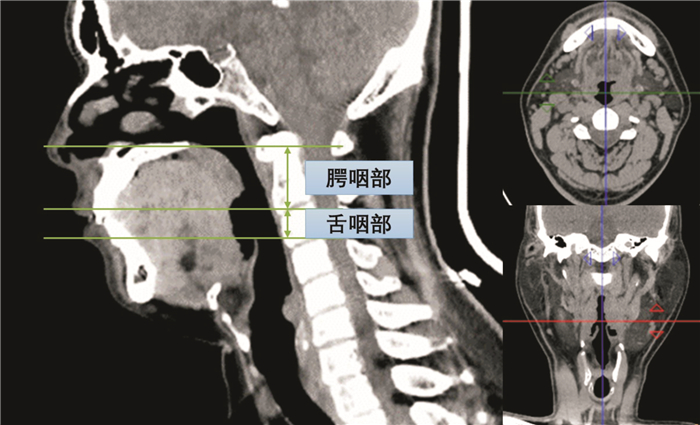
摘要: 目的 分析影响体位依赖性(positional obstructive sleep apnea, POSA)和非体位依赖性OSA(non-positional OSA,NPOSA)患者悬雍垂腭咽成形术疗效的因素,并探讨二者影响因素之间的差异。方法 回顾性分析2020年11月-2023年11月在浙江大学医学院附属第二医院耳鼻咽喉科接受治疗并追踪随访的101例OSA患者的临床资料,其中45例POSA患者,56例NPOSA患者,均行夜间睡眠呼吸监测及三维计算机断层扫描(3D-CT)评估上气道解剖结构。患者均接受保留悬雍垂的改良腭咽成形术(han-uvulopalatopharyngoplasty, H-UPPP),术后3个月随访。结果 手术总体有效率为55.45%,接受H-UPPP的POSA手术成功率(30/45,66.7%)高于NPOSA(26/56,46.4%),2组比较差异有统计学意义(P=0.042)。POSA的H-UPPP疗效与腭咽部气道最小左右径(r=-0.505,P < 0.001)、舌咽部气道最小左右径(mLAT)(r=-0.474,P=0.001)和最小横截面积(r=-0.394,P=0.007)呈负相关。Logistic分析显示,舌咽部mLAT是POSA患者手术疗效的显著预测因子(OR 0.873;95%CI 0.798~0.955,P=0.003)。年龄是NPOSA患者手术疗效的显著预测因子(OR 0.936;95%CI 0.879~0.998,P=0.042)。结论 POSA患者H-UPPP手术疗效高于NPOSA。舌咽部mLAT是影响POSA疗效的重要预测因素。年龄是影响NPOSA疗效的预测因素。
-
关键词:
- 体位 /
- 改良悬雍垂腭咽成形术 /
- 阻塞性睡眠呼吸暂停低通气 /
- 治疗结果
Abstract: Objective To analyze the factors influencing the outcome of uvulopalatopharyngoplasty in positional obstructive sleep apnea(POSA) and non-positional OSA(NPOSA) patients, and to explore the differences between the two groups.Methods The data of 101 patients with obstructive sleep apnea who received treatment from November 2020 to November 2023 were retrospectively analyzed. Among them, 45 positional patients(POSA group) and 56 non-positional patients(NPOSA group), who underwent overnight polysomnography were included. The upper airway(UA) anatomy was evaluated by three-dimensional computer tomography(3D-CT). All patients received revised uvulopalatopharyngoplasty with uvula preservation and were followed using polysomnography for at least three months postoperatively.Results The overall effective rate was 55.45%. The surgical success rate in POSA undergoing UPPP was higher than NPOSA(POSA 30/45, 66.7% versus NPOSA 26/56, 46.4%, P=0.042). The H-UPPP effect of POSA was negatively correlated with the minimum lateral airway of the Velopharyngeal airway(r=-0.505, P < 0.001), the minimum lateral airway of the glossopharyngeal airway(r=-0.474, P=0.001) and the minimum cross-sectional area(r=-0.394, P=0.007). Logistic analysis showed that minimal lateral airway of the glossopharynxgeum(mLAT)(OR 0.873; 95%CI 0.798-0.955, P=0.003) was a significant predictor for surgical outcomes among POSA patients. In NPOSA, age(OR 0.936; 95%CI 0.879-0.998, P=0.042) was a significant predictor for surgical outcomes.Conclusion The effect of H-UPPP was higher in POSA than in NPOSA. The width of glossopharyngeal mLAT was an important predictor of POSA efficacy. Age was a predictor of NPOSA efficacy. -

-
表 1 2组OSA患者的术前临床资料比较
X±S,M(P25,P75) 项目 POSA(n=45) NPOSA(n=56) t/Z P 一般资料 年龄/岁 34(30,44) 40(32,46) -1.412 0.158 BMI/kg/m2 26.80(24.60,28.40) 28.07(25.80,29.33) -2.071 0.038 AHI/次/h 44.00(29.40,54.60) 63.65(50.18,75.52) -4.178 < 0.01 LSpO2/% 78.00(73.5,82.5) 72.00(67.0,78.5) -3.46 0.001 TS90/% 4.07(1.50,16.10) 15.60(3.18,34.05) -2.498 0.013 腭咽部/mm MAP 7.72±2.80 7.27±2.65 0.892 0.375 mLAT 11.70(8.70,16.05) 10.50(7.15,12.50) -2.129 0.033 mCSA 89.00(63.61,125.86) 75.20(45.15,94.38) -2.245 0.025 舌咽部/mm mAP 13.75±4.38 14.12±4.87 -0.439 0.662 mLAT 15.40(9.75,25.25) 15.50(8.83,21.83) -0.799 0.424 mCSA 197.00(120.56,279,60) 187.32(141.10,259.63) -0.083 0.934 AL/mm 85.61±8.91 85.87±8.47 -0.719 0.472 MH/mm 14.04±6.64 15.10±6.44 -3.915 < 0.01 表 2 POSA患者手术有效者与无效者术前临床资料比较
X±S,M(P25,P75) 项目 有效(n=30) 无效(n=15) t/Z P 一般资料 年龄/岁 34(31,45) 35(29,43) -0.241 0.809 BMI/kg/m2 26.85(24.02,28.45) 26.12(24.90,28.10) -0.253 0.800 AHI/次/h 44.80±17.85 42.47±19.89 0.398 0.693 LSpO2/% 78.0(72.0,82.3) 78.0(75.0,83.4) -0.458 0.647 TS90/% 4.10(1.50,20.40) 3.40(1.30,13.30) -0.458 0.647 腭咽部/mm MAP 7.69±2.86 7.77±2.78 -0.089 0.929 mLAT 10.55(7.47,12.68) 16.00(13.00,18.90) -3.347 0.001 mCSA 84.30(56.43,114.00) 105.80(87.00,135.30) -1.866 0.062 舌咽部/mm mAP 13.53±4.68 14.19±3.82 -0.472 0.639 mLAT 14.15±6.86 23.57±9.98 -3.719 0.001 mCSA 179.62±82.65 259.87±97.97 -2.886 0.006 AL/mm 82.90(76.88,91.00) 83.50(78.90,95.40) -1.12 0.263 MH/mm 13.59±7.63 13.22±8.03 0.882 0.126 表 3 NPOSA患者手术有效者与无效者术前临床资料比较
X±S,M(P25,P75) 项目 有效(n=26) 无效(n=30) t/Z P 一般资料 年龄/岁 36.31±8.18 41.96±10.06 -2.282 0.026 BMI/kg/m2 28.40(24.80,29.40) 27.78(26.10,28.91) -0.016 0.987 AHI/次/h 64.80(48.80,70.40) 63.90(57.30,74.06) -0.288 0.774 LSpO2/% 72.69±7.49 70.23±10.39 1.002 0.321 TS90/% 18.00(3.00,32.80) 14.50(3.70,33.90) -0.846 0.397 腭咽部/mm mAP 7.22±2.27 7.24±2.96 -0.033 0.974 mLAT 11.00(7.80,12.50) 10.70(7.10,12.50) -0.107 0.915 mCSA 72.10±35.25 80.33±42.65 -0.77 0.445 舌咽部/mm mAP 14.46±4.77 13.89±4.94 0.441 0.661 mLAT 10.80(8.90,21.90) 17.80(12.30,21.60) -0.411 0.681 mCSA 203.24±78.95 206.72±105.60 -0.136 0.892 AL/mm 83.03±7.66 85.70±8.87 -1.184 0.242 MH/mm 13.49±6.82 15.05±7.85 -0.789 0.434 -
[1] Benjafield AV, Ayas NT, Eastwood PR, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis[J]. Lancet Respir Med, 2019, 7(8): 687-698. doi: 10.1016/S2213-2600(19)30198-5
[2] El-Kersh K, Cavallazzi R, Patel PM, et al. Effect of Sleep State and Position on Obstructive Respiratory Events Distribution in Adolescent Children[J]. J Clin Sleep Med, 2016, 12(4): 513-517. doi: 10.5664/jcsm.5678
[3] Cartwright RD. Effect of sleep position on sleep apnea severity[J]. Sleep, 1984, 7(2): 110-114. doi: 10.1093/sleep/7.2.110
[4] 中国医师协会睡眠医学专业委员会. 成人阻塞性睡眠呼吸暂停多学科诊疗指南[J]. 中华医学杂志, 2018, 98(24): 1902-1914.
[5] 崔前波, 谭健, 邹哲飞, 等. 阻塞性睡眠呼吸暂停低通气综合征患者改良悬雍垂腭咽成形术术后上气道重塑规律研究[J]. 临床耳鼻咽喉头颈外科杂志, 2022, 36(7): 497-500. https://lceh.whuhzzs.com/article/doi/10.13201/j.issn.2096-7993.2022.07.003
[6] Shie DY, Tsou YA, Tai CJ, et al. Impact of obesity on uvulopalatopharyngoplasty success in patients with severe obstructive sleep apnea: a retrospective single-center study in Taiwan[J]. Acta Otolaryngol, 2013, 133(3): 261-269. doi: 10.3109/00016489.2012.741328
[7] Sheen D, Abdulateef S. Uvulopalatopharyngoplasty[J]. Oral Maxillofac Surg Clin North Am, 2021, 33(2): 295-303. doi: 10.1016/j.coms.2021.01.001
[8] He M, Yin G, Zhan S, et al. Long-term Efficacy of Uvulopalatopharyngoplasty among Adult Patients with Obstructive Sleep Apnea: A Systematic Review and Meta-analysis[J]. Otolaryngol Head Neck Surg, 2019, 161(3): 401-411. doi: 10.1177/0194599819840356
[9] Li HY, Cheng WN, Chuang LP, et al. Positional dependency and surgical success of relocation pharyngoplasty among patients with severe obstructive sleep apnea[J]. Otolaryngol Head Neck Surg, 2013, 149(3): 506-512. doi: 10.1177/0194599813495663
[10] Lee CH, Kim SW, Han K, et al. Effect of uvulopalatopharyngoplasty on positional dependency in obstructive sleep apnea[J]. Arch Otolaryngol Head Neck Surg, 2011, 137(7): 675-679. doi: 10.1001/archoto.2011.99
[11] 李树华, 董莘, 石洪金, 等. CT测量在阻塞性睡眠呼吸暂停综合征上呼吸道狭窄定位诊断中的意义[J]. 中华耳鼻咽喉科杂志, 2002, 37(2): 133-136.
[12] Han D, Ye J, Lin Z, et al. Revised uvulopalatopharyngoplasty with uvula preservation and its clinical study[J]. ORL J Otorhinolaryngol Relat Spec, 2005, 67(4): 213-219. doi: 10.1159/000087390
[13] Oksenberg A, Silverberg DS, Arons E, et al. Positional vs nonpositional obstructive sleep apnea patients: anthropomorphic, nocturnal polysomnographic, and multiple sleep latency test data[J]. Chest, 1997, 112(3): 629-639. doi: 10.1378/chest.112.3.629
[14] Walsh JH, Leigh MS, Paduch A, et al. Effect of body posture on pharyngeal shape and size in adults with and without obstructive sleep apnea[J]. Sleep, 2008, 31(11): 1543-1549. doi: 10.1093/sleep/31.11.1543
[15] Tsuiki S, Almeida FR, Bhalla PS, et al. Supine-dependent changes in upper airway size in awake obstructive sleep apnea patients[J]. Sleep Breath, 2003, 7(1): 43-50. doi: 10.1007/s11325-003-0043-6
[16] Pevernagie DA, Stanson AW, Sheedy PF 2nd, et al. Effects of body position on the upper airway of patients with obstructive sleep apnea[J]. Am J Respir Crit Care Med, 1995, 152(1): 179-185. doi: 10.1164/ajrccm.152.1.7599821
[17] Oksenberg A, Silverberg DS, Arons E, et al. The sleep supine position has a major effect on optimal nasal continuous positive airway pressure: relationship with rapid eye movements and non-rapid eye movements sleep, body mass index, respiratory disturbance index, and age[J]. Chest, 1999, 116(4): 1000-1006. doi: 10.1378/chest.116.4.1000
[18] Ravesloot MJ, de Vries N. One hundred consecutive patients undergoing drug-induced sleep endoscopy: results and evaluation[J]. Laryngoscope, 2011, 121(12): 2710-2716. doi: 10.1002/lary.22369
[19] Tsai WH, Remmers JE, Brant R, et al. A decision rule for diagnostic testing in obstructive sleep apnea[J]. Am J Respir Crit Care Med, 2003, 167(10): 1427-1432. doi: 10.1164/rccm.200112-110OC
[20] Tucker Woodson B. Structural effectiveness of pharyngeal sleep apnea surgery[J]. Sleep Med Rev, 2008, 12(6): 463-479. doi: 10.1016/j.smrv.2008.07.010
[21] 李彦如, 费南希, 曹莉莉, 等. 口呼吸对阻塞性睡眠呼吸暂停患者上气道结构的影响[J]. 临床耳鼻咽喉头颈外科杂志, 2023, 37(7): 529-534. https://lceh.whuhzzs.com/article/doi/10.13201/j.issn.2096-7993.2023.07.005
[22] Dentino K, Ganjawalla K, Inverso G, et al. Upper Airway Length is Predictive of Obstructive Sleep Apnea in Syndromic Craniosynostosis[J]. J Oral Maxillofac Surg, 2015, 73(12 Suppl): S20-25.
[23] Edwards BA, Wellman A, Sands SA, et al. Obstructive sleep apnea in older adults is a distinctly different physiological phenotype[J]. Sleep, 2014, 37(7): 1227-1236. doi: 10.5665/sleep.3844
-




 下载:
下载: