Morphological changes of upper airway in patients with obstructive sleep apnea hypopnea syndrome after H-UPPP
-
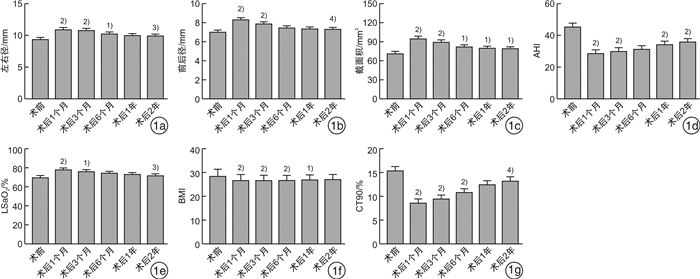
摘要: 目的 研究阻塞性睡眠呼吸暂停低通气综合征(OSAHS)患者行改良悬雍垂腭咽成形术(H-UPPP)后上气道腭咽平面的形态变化规律及与疗效的相关性。方法 选取2016年1月—2019年9月在武汉中心医院行H-UPPP的中重度OSAHS患者36例,于术前和术后1个月、3个月、6个月、1年、2年时测算BMI值,并行PSG检测AHI、LSaO2、CT90,采用64排螺旋CT检查腭咽平面最小前后径、左右径和截面积的变化情况。结果 AHI、LSaO2、CT90、BMI及腭咽平面最小前后径、左右径、截面积的变化在术后1个月时最明显。其中左右径的扩大可维持至术后6个月,术后1年逐渐回缩; 前后径的改善则可维持至术后3个月,术后2年时恢复到术前水平; 最小截面积在术后1个月时扩大明显,3个月后即出现缩小趋势,但术后2年观察时仍较术前有明显改善(P < 0.05);AHI的变化与最小截面积类似,术后2年仍有显著差异(P < 0.001);LSaO2的改善在术后1个月时最明显,可维持至术后3个月,后逐渐恢复; CT90的改善可维持至术后半年,在术后1年时下降明显; BMI在术后1年仍好于术前,但术后2年时恢复至术前水平。AHI与腭咽平面最小前后径和截面积的变化显著相关,而与左右径无明显相关。结论 OSAHS患者H-UPPP术后上气道形态变化主要为前后径、左右径、最小截面积扩大,以术后3个月最为明显,3个月后逐渐出现前后径和最小截面积变小; 最小前后径和截面积的变化可反映手术疗效。
-
关键词:
- 睡眠呼吸暂停低通气综合征,阻塞性 /
- 悬雍垂腭咽成形术 /
- 体层摄影术
Abstract: Objective To investigate the morphological changes of the upper airway palatepharyngeal plane after modified uvulopalatopharyngoplasty(H-UPPP) in patients with obstructive sleep apnea hypopnea syndrome(OSAHS) and efficacy of the surgery.Methods Thirty-six patients diagnosed as moderate to severe OSAHS in the Central Hospital of Wuhan from January 2016 to September 2019 were treated with H-UPPP. PSG and 64 slice spiral CT were performed before operation, 1 month, 3 months, 6 months, 1 year and 2 years after operation to evaluate the changes of AHI, LSaO2, CT90, BMI and the minimum anterior and posterior axis diameter, left and right axis diameter and cross-sectional volume of velopharyngeal plane, respectively.Results The AHI, LSaO2, CT90, BMI were significantly improved, while the minimum anterior posterior axis diameter, left and right axis diameter and cross-sectional volume of velopharyngeal plane were enlarged in the maximum extent at one month after operation. The alteration of left and right axis diameter could be maintained until half a year after operation, but gradually retracted after 1 year after operation. The improvement of anterior and posterior axis diameter can only be maintained until 3 months after operation, and return to the preoperative level 2 years after operation; The minimum cross-sectional area improved significantly at 1 month after operation and decreased after 3 months, but there was still a significant improvement at 2 years after operation(P < 0.05). The change of AHI was similar to that of the minimum cross-sectional area, and there was still a significant difference at 2 years after operation(P < 0.001); The improvement of LSaO2 was the most significant at 1 month after operation, which could be maintained until 3 months after operation, and then gradually recovered. The improvement of CT90 could be maintained until half a year after operation, and decreased significantly at 1 year after operation. BMI was still better than that before operation at 1 year after operation, but returned to the preoperative level at 2 years after operation. The improvement of AHI was mainly related to the minimum anterior posterior axis diameter and cross-sectional area of velopharyngeal plane, but not to the left and right axis diameters.Conclusion The morphological changes of upper airway in patients with OSAHS after H-UPPP are mainly the improvement of anterior posterior diameter, left and right diameter and minimum cross-sectional area caused by removing the anatomical load of upper airway within 3 months after operation, but the reduction of anterior posterior diameter and minimum cross-sectional area gradually occurs after 3 months, resulting in the weakening of surgical effect. -

-
表 1 36例患者术后各时间节点疗效比较
例(%) 时间 治愈 显效 有效 总有效 术后1个月 1(2.8) 12(33.3) 1(2.8) 14(38.9) 术后3个月 2(5.6) 10(27.8) 2(5.6) 14(38.9) 术后6个月 1(2.8) 12(33.3) 0(0) 13(36.1) 术后1年 0(0) 5(13.9) 1(2.8) 6(16.7) 术后2年 0(0) 4(11.1) 2(5.6) 6(16.7) -
[1] Gottlieb DJ, Punjabi NM. Diagnosis and Management of Obstructive Sleep Apnea: A Review[J]. JAMA, 2020, 323(14): 1389-1400. doi: 10.1001/jama.2020.3514
[2] Hingley L, Jeiranikhameneh A, Beirne S, et al. Modeling the upper airway: A precursor to personalized surgical interventions for the treatment of sleep apnea[J]. J Biomed Mater Res A, 2020, 108(6): 1419-1425. doi: 10.1002/jbm.a.36913
[3] Wang F, Liu Y, Xu H, et al. Association between Upper-airway Surgery and Ameliorative Risk Markers of Endothelial Function in Obstructive Sleep Apnea[J]. Sci Rep, 2019, 9(1): 20157. doi: 10.1038/s41598-019-56601-w
[4] Carberry JC, Jordan AS, White DP, et al. Upper Airway Collapsibility(Pcrit)and Pharyngeal Dilator Muscle Activity are Sleep Stage Dependent[J]. Sleep, 2016, 39(3): 511-521. doi: 10.5665/sleep.5516
[5] Kuzucu I, Parlak IS, Baklaci D, et al. Morphometric evaluation of the pterygoid hamulus and upper airway in patients with obstructive sleep apnea syndrome[J]. Surg Radiol Anat, 2020, 42(5): 489-496. doi: 10.1007/s00276-019-02314-8
[6] Mansukhani MP, Olson EJ, Caples SM. Upper Airway Surgery for Obstructive Sleep Apnea[J]. JAMA, 2020, 324(12): 1161-1162. doi: 10.1001/jama.2020.9332
[7] 冀永进, 李强, 张艳廷, 等. H-UPPP联合内镜下低温等离子舌根切除术治疗重度OSA的对照研究[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(4): 324-328. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202004009.htm
[8] 谭健, 陈伟, 胡姚, 等. 诱导睡眠后上气道阻塞部位的CT定位对阻塞性睡眠呼吸暂停患者病情及其手术疗效的评估价值[J]. 临床耳鼻咽喉头颈外科杂志, 2021, 35(8): 683-688. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202108003.htm
[9] 中华医学会呼吸病学分会睡眠呼吸障碍学组. 阻塞性睡眠呼吸暂停低通气综合征诊治指南(2011年修订版)[J]. 中华结核和呼吸杂志, 2012, 35(1): 9-12. doi: 10.3760/cma.j.issn.1001-0939.2012.01.007
[10] Whyte A, Gibson D. Imaging of adult obstructive sleep apnoea[J]. Eur J Radiol, 2018, 102: 176-187. doi: 10.1016/j.ejrad.2018.03.010
[11] 中华耳鼻咽喉头颈外科杂志编辑委员会, 中华医学会耳鼻咽喉头颈外科学分会咽喉学组. 阻塞性睡眠呼吸暂停低通气综合征诊断和外科治疗指南[J]. 中华耳鼻咽喉头颈外科杂志, 2009, 44(2): 95-96. doi: 10.3760/cma.j.issn.1673-0860.2009.02.003
[12] 佘万东, 王健, 钱晓云, 等. 阻塞性睡眠呼吸暂停综合征悬雍垂腭咽成形术的临床观察[J]. 中华耳鼻咽喉科杂志, 2001, 36(3): 227-230. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHEB200103032.htm
[13] Heiser C, Steffen A, Hofauer B, et al. Effect of Upper Airway Stimulation in Patients with Obstructive Sleep Apnea(EFFECT): A Randomized Controlled Crossover Trial[J]. J Clin Med, 2021, 10(13): 2880. doi: 10.3390/jcm10132880
[14] 董佳佳, 叶京英, 张俊波, 等. 悬雍垂腭咽成形术联合软腭前移术后气道结构变化的研究[J]. 中华耳鼻咽喉头颈外科杂志, 2013, 48(4): 289-294. doi: 10.3760/cma.j.issn.1673-0860.2013.04.006
[15] Wallace E, Eckert D, Osman A, et al. P155 Effects of upper airway muscle training on upper airway physiology in people with obstructive sleep apnea[J]. Sleep Advances, 2021, 2(Supplement_1): A72.
[16] Eckert DJ. Phenotypic approaches to obstructive sleep apnoea-New pathways for targeted therapy[J]. Sleep Med Rev, 2018, 37: 45-59. doi: 10.1016/j.smrv.2016.12.003
[17] Shokoueinejad M, Fernandez C, Carroll E, et al. Sleep apnea: a review of diagnostic sensors, algorithms, and therapies[J]. Physiol Meas, 2017, 38(9): R204-R252. doi: 10.1088/1361-6579/aa6ec6
[18] Osman AM, Carter SG, Carberry JC, et al. Obstructive sleep apnea: current perspectives[J]. Nat Sci Sleep, 2018, 10: 21-34. doi: 10.2147/NSS.S124657
[19] Tracy LF, Shehan J, Grillone GA. Upper Airway Burn Injury[J]. Oper Tech Otolaryngol Head Neck Surg, 2020, 31(4): 295-300. doi: 10.1016/j.otot.2020.10.006
-




 下载:
下载: