Effect of mouth breathing on upper airway structure in patients with obstructive sleep apnea
-
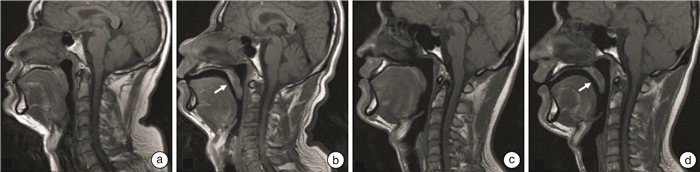
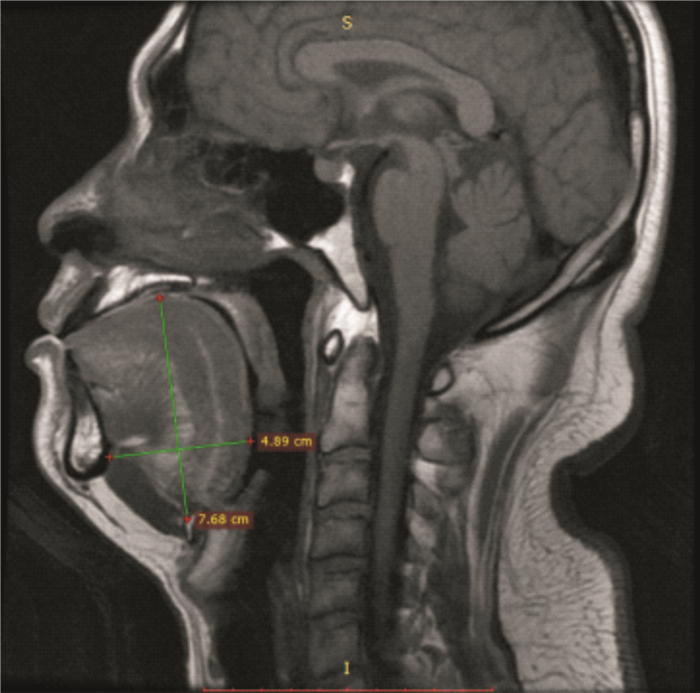
摘要: 目的 研究在经口或经鼻呼吸时,阻塞性睡眠呼吸暂停低通气综合征(OSAHS)患者和正常人的咽壁组织形态结构的变化,探索相关影响因素。方法 29例成人OSAHS患者及20例无鼾对照,分别于受试者清醒时及佩戴鼻夹经口呼吸时行MRI获取上气道结构测量指标。分析:①无鼾对照/OSAHS患者口呼吸与鼻呼吸上气道结构的变化;②OSAHS患者与对照口呼吸时上气道结构变化的差异及影响因素。结果 对照组男15例,女5例,呼吸暂停低通气指数(AHI)均 < 5次/h。OSAHS患者男26例,女3例,平均AHI(40.4±23.1)次/h,睡眠时最低血氧饱和度(LSaO2)平均79.5%±10.0%。对照组及OSAHS口呼吸时均观察到下颌骨与咽后壁的垂直距离变小(P < 0.05);舌体长轴减小(P < 0.05),舌体与软、硬腭接触区域减小。对照组软腭后及舌后气道总容积无显著改变(P>0.05)。而OSAHS患者软腭后气道最小截面积、气道体积明显减小(P < 0.001)。OSAHS患者口呼吸时悬雍垂平面左右径减小,与对照组趋势相反(P=0.017)。患者的AHI与口呼吸时软腭后气道容积的减小量正相关(P=0.001);而下颌骨与咽后壁间距的减小量与气道长度呈正相关(P < 0.001)。结论 口呼吸导致舌体长轴缩短、软腭与舌体接触面积减小,下颌骨与咽后壁的垂直距离减小、会厌平面截面积降低。OSAHS患者与对照的变化特点存在较大差异。口呼吸时患者软腭后气道的多个径线、面积及体积减小,且在重度患者更显著。
-
关键词:
- 睡眠呼吸暂停, 阻塞性 /
- 口呼吸 /
- 上气道
Abstract: Objective To compare the changes of morphology of pharynx in patients with obstructive sleep apnea hypopnea syndrome (OSAHS) and healthy individuals during oral or nasal breathing, and explore the relevant influencing factors.Methods Twenty-nine adult patients with OSAHS and 20 non-snoring controls underwent MRI to obtain upper airway structural measurements while the subjects were awake and during mouth breathing with a nasal clip.The following were analyzed. ①The changes of upper airway structure of oral and nasal respiration in non-snoring control/OSAHS patients were observed; ②The differences and influencing factors of upper airway structure changes between OSAHS patients and controls were compared during breathing.Results The control group consisted of 15 males and 5 females, with an apnea-hypopnea index (AHI) < 5 events/h, while the OSAHS group comprised 26 males and 3 females with an AHI of 40.4±23.1 events/h and the mean lowest arterial oxygen saturation (LSaO2) was 79.5% ±10.0%. In the both groups, the vertical distance between the mandible and the posterior pharyngeal wall decreased (P < 0.05); The long axis of tongue body decreased (P < 0.05), and the contact area between tongue and palate decreased. There was no significant change in the total volume of the retropalatine(RP) and retroglossal(RG) airway in the control group (P>0.05). However, the minimum cross-sectional area and volume of the RP airway in OSAHS decreased (P < 0.001). The lateral diameters of uvula plane in OSAHS decreased during mouth breathing, which was contrary to the trend in the control group (P=0.017). The AHI of patients was positively correlated with the reduction of the volume of the RP airway during oral breathing (P=0.001); The reduction of the distance between the mandible and the posterior pharyngeal wall was positively correlated with the length of the airway (P < 0.001).Conclusion Mouth breathing leads to the shortening of the long axis of the tongue, the reduction of the contact area between the soft palate and the tongue, vertical distance between the mandible and the posterior pharyngeal wall, and the cross-sectional area of the epiglottis plane. These changes vary between OSAHS patients and controls. During mouth breathing, the diameters, areas and volumes of the RP area decreased, and were more significant in severe cases.-
Key words:
- sleep apnea, obstructive /
- mouth breathing /
- upper airway
-

-
表 1 研究对象的一般情况
M(P25,P75) 组别 例数 年龄 BMI AHI LSaO2 仰卧位AHI OSAHS组 29 39.0(31.0,47.5) 26.1(24.5,27.7) 42.7(15.9,56.5) 82.0(73.0,88.0) 55.0(35.4,67.9) 对照组 20 26.5(24.0,29.8) 23.8(21.3,26.1) 1.5(0.7,2.9) 94.0(92.0,94.0) 2.4(1.1,3.8) 表 2 2组口呼吸与鼻呼吸时软腭后气道相关测量参数的比较
M(P25,P75) 对照组(n=20) OSAHS组(n=29) 鼻呼吸 口呼吸 z/t 鼻呼吸 口呼吸 z/t 硬腭平面气道面积/cm2 2.82(2.46,3.51) 2.59(1.52,3.58) -1.372 2.39(1.76,3.05) 1.24(0.87,2.24) -3.4362) 硬腭平面气道前后径/cm 1.59(1.39,1.79) 1.43(1.22,1.88) -1.111 1.41(1.26,1.69) 1.10(0.80,1.53) -3.1242) 硬腭平面气道左右径/cm 2.26±0.46 1.48±0.40 0.958 2.04±0.39 1.18±0.58 4.6412) 悬雍垂平面气道面积/cm2 1.91(1.66,2.81) 2.02(1.38,3.07) -0.240 0.69(0.52,1.02) 0.35(0.20,0.72) -2.2111) 悬雍垂平面形状(前后径和左右径比值,%) 81.09
(60.23,89.86)70.38
(49.00,85.22)-2.0251) 94.64
(61.95,123.22)113.92
(78.40,308.82)-1.486 悬雍垂平面前后径/cm 1.28(1.00,1.55) 1.46(0.87,2.00) -0.675 0.92(0.64,1.23) 0.68(0.46,1.68) -0.144 悬雍垂平面左右径/cm 1.76(1.39,1.92) 2.05(1.84,2.27) -3.1141) 0.94(0.80,1.34) 0.56(0.40,1.13) -2.9081) 软腭后气道最小截面积/cm2 1.28(1.11,1.68) 1.24(0.84,1.46) -1.285 0.53(0.42,0.72) 0.25(0.00,0.35) -3.9652) 软腭后气道最小截面积前后径 0.91(0.74,1.03) 0.79(0.66,0.96) -1.350 0.71(0.60,0.87) 0.30(0.00,0.55) -3.0522) 软腭后气道最小截面积左右径 1.93(1.72,2.20) 1.89(1.65,2.18) -0.308 1.01(0.68,1.33) 0.50(0.00,0.83) -3.1892) 软腭后气道体积/cm3 5.30(4.06,6.43) 4.39(2.50,6.48) -1.764 4.81(2.61,5.50) 1.64(0.52,3.78) -3.6712) 软腭硬腭间夹角/° 125.25±8.10 124.17±10.16 0.323 123.36±6.39 126.17±12.73 -1.541 与鼻呼吸比较,1)P < 0.05,2)P < 0.01。 表 3 2组口呼吸与鼻呼吸时舌后气道相关测量参数的比较
M(P25,P75) 无鼾对照(n=20) OSAHS(n=29) 鼻呼吸 口呼吸 z/t 鼻呼吸 口呼吸 z/t 会厌平面气道面积/cm2 3.27±0.88 2.52±0.85 2.8951) 2.69±1.40 2.02±1.04 3.6652) 会厌平面前后径/cm 1.48(1.29,1.64) 1.31(1.03,1.55) -1.086 1.39(0.99,1.72) 1.17(0.97,1.57) -3.7622) 会厌平面左右径/cm 2.86(2.63,3.16) 3.02(2.49,3.25) -1.132 2.71(2.20,3.19) 2.47(2.13,2.77) -2.2951) 会厌平面形状(前后径和左右径比值%) 49.22
(40.48,69.93)41.14
(36.31,57.76)-1.372 54.26
(45.26,67.85)54.52
(45.63,59.47)-0.793 舌后气道最小截面积/cm2 2.18(1.83,2.58) 2.31(1.83,2.69) -0.370 1.27[1.05,1.86] 1.20[0.93,1.77] -1.634 前后径/cm 1.36±0.32 1.51±0.42 -1.474 1.48±0.47 1.58±0.52 -0.899 左右径/cm 2.11(1.63,2.22) 2.28(2.10,2.59) -2.5911) 1.00(0.65,1.52) 0.95(0.54,1.76) -1.224 舌后气道体积/cm3 6.42(4.50,8.59) 6.01(5.09,9.03) -0.414 5.13(4.16,6.67) 4.47(3.70,5.20) -1.766 舌体长轴长度/cm 6.33±0.77 5.86±0.60 2.8191) 7.72±0.64 7.23±0.49 5.1722) 舌体短轴长度/cm 5.98(5.45,6.27) 5.35(4.94,5.65) -2.6792) 5.33(5.03,5.61) 5.21(4.84,5.60) -1.045 舌短轴与长轴的比例 90.33
(87.75,97.34)87.24
(84.09,93.63)-0.893 69.18
(62.94,77.20)71.70
(67.01,77.78)-2.5952) 下颌骨与咽后壁的垂直距离/cm 7.91±0.76 7.65±0.65 2.3791) 7.65±0.91 7.42±0.90 2.9472) 下颌骨与舌骨的距离/cm 4.72(4.31,5.42) 4.55(4.03,4.92) -1.154 5.06(4.79,5.64) 4.97(4.46,5.59) -0.300 舌骨到硬腭垂直间距/cm 6.56±0.67 6.83±0.67 -3.9172) 8.13±0.65 8.42±0.70 -2.1361) 与鼻呼吸比较,1)P < 0.05,2)P < 0.01。 -
[1] Benjafield AV, Ayas NT, Eastwood PR, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis[J]. Lancet Respir Med, 2019, 7(8): 687-698. doi: 10.1016/S2213-2600(19)30198-5
[2] Värendh M, Andersson M, Bjørnsdottir E, et al. Nocturnal nasal obstruction is frequent and reduces sleep quality in patients with obstructive sleep apnea[J]. J Sleep Res, 2018, 27(4): e12631. doi: 10.1111/jsr.12631
[3] Sawa A, Suzuki H, Niwa H, et al. Assessment of Screening for Nasal Obstruction among Sleep Dentistry Outpatients with Obstructive Sleep Apnea[J]. Dent J(Basel), 2020, 8(4): 119.
[4] Fitzpatrick MF, McLean H, Urton AM, et al. Effect of nasal or oral breathing route on upper airway resistance during sleep[J]. Eur Respir J, 2003, 22(5): 827-832. doi: 10.1183/09031936.03.00047903
[5] Koutsourelakis I, Vagiakis E, Roussos C, et al. Obstructive sleep apnoea and oral breathing in patients free of nasal obstruction[J]. Eur Respir J, 2006, 28(6): 1222-1228. doi: 10.1183/09031936.00058406
[6] Hoel HC, Kvinnesland K, Berg S. Impact of nasal resistance on the distribution of apneas and hypopneas in obstructive sleep apnea[J]. Sleep Med, 2020, 71: 83-88. doi: 10.1016/j.sleep.2020.03.024
[7] Meurice JC, Marc I, Carrier G, et al. Effects of mouth opening on upper airway collapsibility in normal sleeping subjects[J]. Am J Respir Crit Care Med, 1996, 153(1): 255-259. doi: 10.1164/ajrccm.153.1.8542125
[8] Suzuki M, Tanuma T. The effect of nasal and oral breathing on airway collapsibility in patients with obstructive sleep apnea: Computational fluid dynamics analyses[J]. PloS One, 2020, 15(4): e0231262. doi: 10.1371/journal.pone.0231262
[9] Hu B, Yin G, Fu S, et al. The influence of mouth opening on pharyngeal pressure loss and its underlying mechanism: A computational fluid dynamic analysis[J]. Front Bioeng Biotechnol, 2023, 10: 1081465. doi: 10.3389/fbioe.2022.1081465
[10] Koo SK, Park GH, Koh TK, et al. Effect of mouth closure on upper airway obstruction in patients with obstructive sleep apnoea exhibiting mouth breathing: a drug-induced sleep endoscopy study[J]. Eur Arch Otorhinolaryngol, 2020, 277(6): 1823-1828. doi: 10.1007/s00405-020-05904-0
[11] Lee SH, Choi JH, Shin C, et al. How does open-mouth breathing influence upper airway anatomy?[J]. Laryngoscope, 2007, 117(6): 1102-1106. doi: 10.1097/MLG.0b013e318042aef7
[12] Hu B, Ye J, Yin G, et al. The influential factors on the morphological changes of upper airway associated with mouth opening[J]. Laryngoscope, 2018, 128(12): 2902-2909. doi: 10.1002/lary.27212
[13] 中国医师协会睡眠医学专业委员会. 成人阻塞性睡眠呼吸暂停多学科诊疗指南[J]. 中华医学杂志, 2018, 98(24): 1902-1914. https://www.cnki.com.cn/Article/CJFDTOTAL-SMZZ201811020.htm
[14] Sutherland K, Lowth AB, Antic N, et al. Volumetric magnetic resonance imaging analysis of multilevel upper airway surgery effects on pharyngeal structure[J]. Sleep, 2021, 44(12): zsab183. doi: 10.1093/sleep/zsab183
[15] Lin H, Xiong H, Ji C, et al. Upper airway lengthening caused by weight increase in obstructive sleep apnea patients[J]. Respir Res, 2020, 21(1): 272. doi: 10.1186/s12931-020-01532-8
[16] Iwatani K, Matsuo K, Kawase S, et al. Effects of open mouth and rubber dam on upper airway patency and breathing[J]. Clin Oral Investig, 2013, 17: 1295-1299. doi: 10.1007/s00784-012-0810-5
-



 下载:
下载: