Evaluation of a portable sleep monitor for the postoperative efficacy of supraglottoplasty in neonates with severe laryngomalacia
-
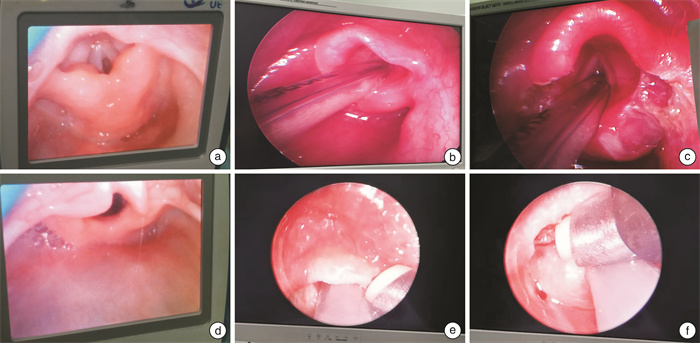
摘要: 目的 探讨便携式睡眠监测仪(portable monitor divice,PMD)是否可以用于评估新生儿重度喉软化(laryngomalacia,LM)行声门上成形术(supraglottoplasty,SGP)的疗效。 方法 回顾性分析2020年1月至2023年11月院诊治的11例重度LM新生儿,均行全麻下SGP,并在术前术后行床旁PMD监测,比较术前术后的睡眠监测指标的变化,应用SPSS 18.0统计学软件,采用Wilcoxon符号轶和检验,P<0.05为差异有统计学意义。 结果 11例患儿术后1周,阻塞性睡眠呼吸暂停低通气指数(OAHI)、阻塞性呼吸暂停指数(OAI)、氧减指数(ODI)均低于术前,最低血氧饱和度(SpO2)高于术前,差异有统计学意义(P<0.05),睡眠呼吸暂停低通气指数(AHI)和术前比较差异无统计学意义;术后1个月,AHI、OAHI、OAI、ODI均低于术前,最低SpO2、平均SpO2均高于术前,差异有统计学意义(P<0.05)。 结论 PMD检查的部分参数可用于评估新生儿重度LM的SGP的疗效,是新生儿LM病情评估的重要辅助手段。Abstract: Objective To explore whether a portable monitor device(PMD) can be used to evaluate the efficacy of supraglottoplasty(SGP) in neonates with severe laryngomalacia(LM). Methods A retrospective analysis of 11 neonates diagnosed as severe LM treated in our hospital from January 2020 to November 2023 was performed. All neonates underwent SGP under general anesthesia and overnight PMD monitoring before and after surgery.The changes of sleep monitoring parameters before and after surgery were compared, SPSS 18.0 statistical software was applied and Wilcoxon symbolic-rank l test was used. P < 0.05 showed statistical difference. Results One week after surgery, the obstructive apnea-hypopnea index(OAHI), obstructive apnea index(OAI), oxygen desaturationindex(ODI) of 11 children were lower than those before operation, and the minimum pulse oximetry saturation(SpO2) was higher than that before operation, P < 0.05, the difference was statistically significant, and there was no significant difference in sleep apnea hypopnea index(AHI) compared with that before operation. One month after surgery, AHI, OAHI, OAI and ODI were lower than those before operation, and the minimum SpO2 and mean SpO2 were higher than those before operation, P < 0.05, the difference was statistically significant. Conclusion Some parameters of PMD examination can be used to evaluate the efficacy of SGP in neonatal severe LM, which is an important auxiliary means for the evaluation of neonatal LM.
-
Key words:
- laryngomalacia neonate /
- supraglottoplasty /
- portable sleep monitoring
-

-
表 1 手术前后患儿症状比较
例 时间 喉喘鸣 呼吸困难 喂养困难 明显 轻度 无 发绀 明显三凹征 轻度三凹征 高碳酸血症 鼻饲 呛奶 吐奶 术前 11 0 0 3 8 3 5 7 4 3 术后1周 3 8 0 0 2 9 0 5 2 2 术后1个月 0 11 0 0 0 3 0 2 1 0 表 2 手术前后睡眠监测指数中位数比较
M(P25,P75) 监测项目 术前 术后1周 术后1个月 Z 中位数 中位数 Z 中位数 Z AHI/(次/h) 28.9(26.2,35.1) 27.5(25.3,30.2) -1.957 14.3(12.4,15.4) -2.934 -1.992 OAHI/(次/h) 21.8(17.8,24.3) 13.8(12.8,19.8) -2.934 3.7(2.8,5.6) -2.934 -2.201 CAI/(次/h) 9.6(8.1,11.4) 9.1(8.5,11.1) -0.356 9.4(8.1,10.3) -1.912 -0.315 OAI/(次/h) 8.5(7.3,8.8) 6.2(4.1,6.3) -2.845 2.3(1.3,2.7) -2.940 -2.201 MAI/(次/h) 1.8(1.3,2.8) 1.7(1.2,2.4) -0.679 1.4(1.2,2.3) -1.876 -1.261 最低SPO2/% 79.0(73.0,82.0) 82.0(77.0,84.0) -2.671 84.0(83.0,85.0) -2.814 -2.214 平均SPO2/% 92.5(91.3,94.2) 93.6(92.2,94.1) -1.600 95.3(94.8,95.3) -2.938 -1.572 ODI/(次/h) 16.9(15.5,20.3) 7.4(5.8,9.4) -2.934 3.5(2.1,5.3) -2.936 -2.201 平均心率/(次/min) 138.5(135.6,140.0) 139.7(134.5,146.5) -1.600 137.2(135.8,140.8) -1.779 -0.943 表 3 便携式睡眠监测仪与传统评估方法比较
项目 PMD 喉镜 脉搏SPO2 心电监护 血气分析 有创检查 否 是 否 否 是 可床边操作 是 是 是 是 是 有电子存档 是 是 否 否 是 可持续监测 是 是 是 是 否 软件分析 是 否 否 否 否 -
[1] 中国妇幼保健学会微创分会儿童耳鼻咽喉学组. 儿童喉软化症诊断与治疗临床实践指南[J]. 临床耳鼻咽头颈外科杂志, 2020, 34(11): 961-965.
[2] 刘晓君, 李晓艳. 喉软化症的发病机制及相关疾病研究进展[J]. 国际耳鼻咽喉头颈外科杂志, 2019, 43(5): 260-263. doi: 10.3760/cma.j.issn.1673-4106.2019.05.004
[3] Gan RWC, Moustafa A, Turner K, et al. Histopathology of laryngomalacia[J]. Acta Otolaryngol, 2021, 141(1): 85-88. doi: 10.1080/00016489.2020.1821246
[4] Sivarajah S, Isaac A, Anderson S, et al. Validity of laryngomalacia classification systems: a multi-institutional agreement study[J]. Clin Otolaryngol, 2020, 45(4): 471-476. doi: 10.1111/coa.13530
[5] Cialente F, Meucci D, Tropiano ML, et al. Changes in breathing patterns after surgery in severe laryngomalacia[J]. Children(Basel), 2021, 8(12): 1120.
[6] Miller C, Parikh SR. Does supraglottoplasty improve outcomes in children with laryngomalacia?[J]. Laryngoscope, 2019, 129(2): 285-287. doi: 10.1002/lary.27127
[7] Alshumrani RA, Matt BH, Daftary AS, et al. Correlation between the clinical severity of laryngomalacia and endoscopic findings[J]. Saudi Med J, 2020, 41(4): 406-412. doi: 10.15537/smj.2020.4.25014
[8] Cortes MC, Villamor P, de la Torre González C, et al. Complete polysomnographic parameters in infants with severe laryngomalacia prior to and after supraglottoplasty[J]. Int J Pediatr Otorhinolaryngol, 2019, 119: 131-135. doi: 10.1016/j.ijporl.2019.01.033
[9] Olney DR, Greinwald JH Jr, Smith RJ, et al. Laryngomalacia and its treatment. [J]. Laryngoscope, 1999, 109(11): 1770-1775. doi: 10.1097/00005537-199911000-00009
[10] Roger G, Denoyelle F, Triglia JM, et al. Severe laryngomalacia: surgical indications and results in 115 patients[J]. Laryngoscope, 1995, 105(10): 1111-1117. doi: 10.1288/00005537-199510000-00018
[11] Carr MM, Ramadan J, Bauer E. Laryngomalacia in neonates versus older infants: HCUP-KID perspective[J]. Clin Pediatr, 2020, 59(7): 679-685. doi: 10.1177/0009922820908917
[12] 姜岚, 韩富根, 许莹, 等. 低温等离子在婴幼儿喉软化症声门上成形术中的应用[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(9): 844-847, 852. https://lceh.whuhzzs.com/article/doi/10.13201/j.issn.2096-7993.2020.09.017
[13] 浦诗磊, 李晓艳. 改良声门上成形术治疗喉软化症的疗效评价[J]. 临床耳鼻咽喉头颈外科杂志, 2019, 33(11): 1072-1075, 1080. https://lceh.whuhzzs.com/article/doi/10.13201/j.issn.1001-1781.2019.11.016
[14] El-Kholy NA, Hashish MI, ElSobki AA. Coagulation of the lateral surface of aryepiglottic folds as an alternative to aryepiglottic fold release in management of type 2 laryngomalacia[J]. Auris Nasus Larynx, 2020, 47(3): 443-449. doi: 10.1016/j.anl.2019.10.004
[15] 刘燕, 魏萍, 寇巍, 等. 小儿重度喉软化症临床特点及手术疗效影响因素分析[J]. 临床耳鼻咽喉头颈外科杂志, 2022, 36(4): 258-264. https://lceh.whuhzzs.com/article/doi/10.13201/j.issn.2096-7993.2022.04.004
[16] Ng DK, Chan CH. A review of normal values of infant sleep polysomnography[J]. Pediatr Neonatol, 2013, 54(2): 82-87. doi: 10.1016/j.pedneo.2012.11.011
-




 下载:
下载: