Clinical effects of two kinds of nasal bone reductors used for shortened and displaced overlapping external nasal fracture reduction under nasal endoscopy and the impact on ventilation function
-
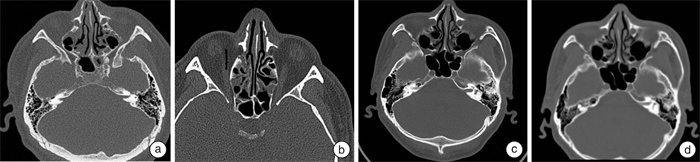
摘要: 目的 探究鼻内镜下2种鼻骨整复器用于缩短移位重叠式外鼻骨折复位的临床效果及对通气功能的影响。 方法 收集2020年1月至2022年2月合肥市第二人民医院耳鼻咽喉科诊治的82例缩短移位重叠式外鼻骨折患者为研究对象,随机数字表法将患者分为对照组(41例)及观察组(41例),2组均实施鼻内镜下闭合性复位术,对照组采用传统平直式鼻骨整复器,观察组采用枪状拉钩式鼻骨整复器。比较2组复位成功率、随访率、临床效果及并发症,术前及术后半年2组采用视觉模拟量表(visual analogue scale,VAS)评分进行美学效果及功能恢复评估,鼻测压仪和鼻声反射仪测量鼻通气功能。 结果 观察组1次复位成功率较对照组明显高,鼻复位适应时间较对照组短(P<0.05),2组术后半年随访率95.12%、92.68%比较差异无统计学意义。观察组临床总有效率高于对照组(94.87% vs 76.32%,P<0.05)。术后2组鼻美观度、鼻塞、嗅觉功能评分较术前明显降低,观察组各项评分均低于对照组(P<0.05)。术后2组鼻腔最小横断面积、鼻腔容积及鼻总呼气量较术前明显增大,观察组明显大于对照组,鼻腔呼气吸气阻力较术前明显减小,观察组明显小于对照组(P<0.05)。观察组并发症总发生率较对照组低(P<0.05)。 结论 枪状拉钩式鼻骨整复器用于缩短移位重叠式外鼻骨折复位患者中,在1次复位成功率、鼻复位适应时间和治疗效果更好,同时在鼻外形美学效果和鼻通气功能、减少并发症方面更具优势。Abstract: Objective To explore the clinical effects of two kinds of nasal bone reductors used for shortened and displaced overlapping external nasal fracture reduction under nasal endoscopy and the impact on ventilation function. Methods From January 2020 to February 2022, 82 patients with shortened and displaced overlapping external nasal fractures diagnosed and treated in the Department of Otolaryngology, the Second People's Hospital of Hefei were collected as the study subjects. The patients were divided into control group(41 cases) and observation group(41 cases) by random number table method. Both groups underwent closed reduction under nasal endoscopy. The control group was treated with traditional straight nasal bone reductor, and the observation group was treated with gun-shaped hook type nasal bone reductor. The success rate of reduction, follow-up rate, clinical effect, and complications were compared between the two groups. The visual analogue scale(VAS) was used to evaluate the aesthetic effect and functional recovery. Rhinomanometry and acoustic rhinometry were used to evaluate nasal ventilation function. Results The success rate of one-time reduction in the observation group was significantly higher than that in the control group, and the nasal reduction adaptation time was shorter than that in the control group(P < 0.05). There was no significant difference in the follow-up rate of 95.12% and 92.68% between the two groups. The success rate of one-time reduction in observation group was significantly higher than that in the control group, and the adaptation time for nasal reduction in observation group was shorter than that in the control group(P < 0.05). There was no significant difference in the follow-up rate of 95.12% and 92.68% between the two groups in six months after surgery. the total clinical effective rate in observation group was higher than that in the control group(94.87% vs 76.32%, P < 0.05). After surgery, the scores of nasal aesthetics, nasal congestion and olfactory function in both groups were significantly lower compared with the preoperative scores. All the scores in the observed group were lower than that in the control group(P < 0.05). After surgery, there were significant increases in the minimum cross-sectional area of nasal cavity, volume of nasal cavity and total nasal expiratory volume in both groups. Above indicators in observation group were significantly greater than that in control group. The nasal exhalation and inhalation resistance was significantly lower than that before operation, and the resistance in observation group was significantly lower than that in control group(P < 0.05). The total incidence of complications was lower than that in observation group(P < 0.05). Conclusion The application of gun-shaped hook-type nasal bone reductor in patients with shortened and displaced overlapping external nasal fractures has better success rate of one-time reduction, adaptation time of nasal reduction and treatment outcome. Moreover, it has more advantages in aesthetic effect of nasal appearance, nasal ventilation function and reduction of complications.
-

-
表 1 2组一般资料比较
组别 例数 性别/例 年龄/岁 骨折至手术时间/d 鼻骨骨折类型/例 鼻骨折原因/例 男 女 Ⅰ型 Ⅱ型 Ⅲ型 车祸 摔伤 其他 观察组 41 30 11 39.66±15.94 6.27±1.91 12 12 17 19 15 7 对照组 41 30 11 42.49±13.76 5.63±2.01 4 11 26 19 16 6 χ2/t <0.001 0.861 1.478 5.927 0.109 P 1.000 0.392 0.143 0.052 0.947 表 2 2组复位成功率及随访率比较
组别 例数 1次复位成功/例(%) 经过1~3次复位成功/例(%) 鼻复位适应时间/月 术后半年随访/例(%) 观察组 41 40(97.56) 41(100.00) 1.53±0.17 39(95.12) 对照组 41 35(85.37) 41(100.00) 1.96±0.20 38(92.68) χ2/t 3.905 - 10.489 <0.001 P 0.048 - <0.001 1.000 表 3 2组临床效果比较
例(%) 组别 例数 显效 有效 无效 总有效 观察组 39 17(43.59) 20(51.28) 2(5.13) 37(94.87) 对照组 38 12(31.58) 17(44.74) 9(23.68) 29(76.32) χ2/t 5.412 P 0.020 表 4 2组鼻外形美学效果、功能恢复比较
分,X±S 组别 例数 鼻美观度 鼻塞 嗅觉功能 术前 术后 术前 术后 术前 术后 观察组 39 6.37±0.83 1.88±0.19 6.22±1.01 2.02±0.21 5.92±0.57 0.62±0.07 对照组 38 6.29±0.87 3.24±0.35 6.39±1.05 3.17±0.38 6.04±0.61 0.98±0.14 t 0.413 21.265 0.724 16.492 0.892 14.327 P 0.681 <0.001 0.471 <0.001 0.375 <0.001 表 5 2组鼻通气功能比较
X±S 组别 例数 鼻腔最小横断面积/cm2 鼻腔容积/cm3 鼻总呼气量/L 鼻腔呼气吸气阻力/(Pa/cm3/s) 术前 术后 术前 术后 术前 术后 术前 术后 观察组 39 0.41±0.05 0.81±0.09 7.06±0.74 17.24±1.95 5.09±0.66 8.04±0.89 2.99±0.29 0.81±0.09 对照组 38 0.39±0.04 0.70±0.08 6.95±0.69 15.03±1.62 5.13±0.58 7.03±0.74 3.04±0.31 0.99±0.14 t 1.935 5.663 0.674 5.402 0.282 5.407 0.731 6.729 P 0.057 <0.001 0.502 <0.001 0.779 <0.001 0.467 <0.001 表 6 2组术后并发症比较
例(%) 组别 例数 鼻血肿 鼻腔粘连 继发性鼻窦炎 通气受限 合计 观察组 39 0(0) 1(2.56) 1(2.56) 0(0) 2(5.13) 对照组 38 1(2.63) 2(5.26) 3(7.89) 3(7.89) 9(23.68) χ2 5.412 P 0.020 -
[1] Raghvi A, Priya K, Rajasekaran S, et al. Evaluating the outcomes of closed reduction of different types of nasal bone fractures[J]. Indian J Otolaryngol Head Neck Surg, 2023, 75(4): 2998-3006. doi: 10.1007/s12070-023-03894-z
[2] 王珮华. 我国鼻骨骨折诊治的现状与建议[J]. 中华耳鼻咽喉头颈外科杂志, 2020, 55(3): 191-194. doi: 10.3760/cma.j.issn.1673-0860.2020.03.001
[3] Kim SY, Nam HJ, Byeon JY, et al. Effectiveness of out-fracture of the inferior turbinate with reduction nasal bone fracture[J]. World J Clin Cases, 2023, 11(27): 6374-6382. doi: 10.12998/wjcc.v11.i27.6374
[4] 周宏, 印爱军, 彭炜, 等. 鼻骨骨折复位术联合鼻中隔成形术对鼻骨骨折伴鼻中隔骨折患者的美学效果分析[J]. 中国美容医学, 2021, 30(12): 37-40.
[5] 汤海, 刘志军. 鼻中隔-鼻骨矫正术治疗外伤性鼻骨骨折合并畸形临床疗效及对鼻腔通气水平影响[J]. 创伤与急危重病医学, 2019, 7(6): 351-354.
[6] 孙虹, 张罗. 耳鼻咽喉头颈外科学[M]. 9版. 北京: 人民卫生出版社, 2018: 192-192.
[7] 钱小飞, 陈建良, 王永军, 等. 鼻骨骨折伴鼻中隔偏曲一期手术疗效观察[J]. 临床耳鼻咽喉头颈外科杂志, 2016, 30(16): 1319-1321. https://lceh.whuhzzs.com/article/doi/10.13201/j.issn.1001-1781.2016.16.015
[8] 张烽, 张勇, 陈伟, 等. 同期行鼻内镜下鼻中隔矫正术联合鼻骨复位对鼻骨骨折患者鼻腔结构及功能的影响[J]. 河北医药, 2023, 45(21): 3293-3296. doi: 10.3969/j.issn.1002-7386.2023.21.021
[9] Äström M, Thet Lwin ZM, Teni FS, et al. Use of the visual analogue scale for health state valuation: a scoping review[J]. Qual Life Res, 2023, 32(10): 2719-2729. doi: 10.1007/s11136-023-03411-3
[10] 宫宇, 胡玮, 张媛霞. 鼻中隔—鼻骨矫正术治疗外伤性鼻骨骨折合并畸形的临床疗效及并发症观察[J]. 贵州医药, 2022, 46(4): 575-576. doi: 10.3969/j.issn.1000-744X.2022.04.037
[11] 武勇进, 王鹏, 韩晓东, 等. 鼻骨CT三维成像技术辅助鼻骨骨折的诊断研究[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(5): 452-455. https://lceh.whuhzzs.com/article/doi/10.13201/j.issn.2096-7993.2020.05.016
[12] 唐旭霞, 张健, 张爱春, 等. 不同分型鼻骨骨折的急诊诊断和治疗[J]. 中华急诊医学杂志, 2014, 23(2): 219-221. doi: 10.3760/cma.j.issn.1671-0282.2014.02.026
[13] 夏世同, 吴四海, 徐婷. 鼻内镜辅助下改良鼻骨骨折复位治疗外伤性歪鼻合并鼻中隔偏曲[J]. 中国耳鼻咽喉头颈外科, 2023, 30(1): 22-25.
[14] 徐希康, 王珮华, 许晨婕, 等. 3D打印鼻骨复位器在骨折复位手术中主观疗效的临床分析[J]. 中国耳鼻咽喉颅底外科杂志, 2019, 25(2): 131-134, 138.
[15] 葛瑜庭, 许晨婕, 王珮华, 等. 两种鼻骨复位器在鼻骨复位术中的应用研究[J]. 中国耳鼻咽喉颅底外科杂志, 2021, 27(2): 131-137.
[16] Gu Y, Yu BQ, Wan X, et al. Effects of modified posterior nasal nerve neurectomy combined with accessory posterior nasal nerve neurectomy on controlling intractable allergic rhinitis[J]. J Cent South Univ Med Sci, 2023, 48(3): 404-413.
[17] 王弦, 吴燕妮, 李宁, 等. 鼻内镜在治疗鼻骨骨折伴外伤性鼻中隔偏曲中的应用[J]. 中国美容医学, 2022, 31(4): 80-82.
[18] 王伟, 曲学华, 崔忠涛. 多层螺旋CT曲面重组联合鼻内镜治疗鼻骨骨折合并畸形的疗效[J]. 中国内镜杂志, 2023, 29(6): 14-19.
[19] 孟新, 刘业海. 内镜下鼻骨骨折复位联合鼻中隔成形术治疗外伤性鼻骨骨折伴鼻中隔骨折的疗效分析[J]. 安徽医学, 2018, 39(8): 978-980.
-




 下载:
下载: