Analysis of vocal fold movement and voice onset behavior in patients with laryngopharyngeal reflux based on high speed laryngeal high-speed videoendoscopy
-
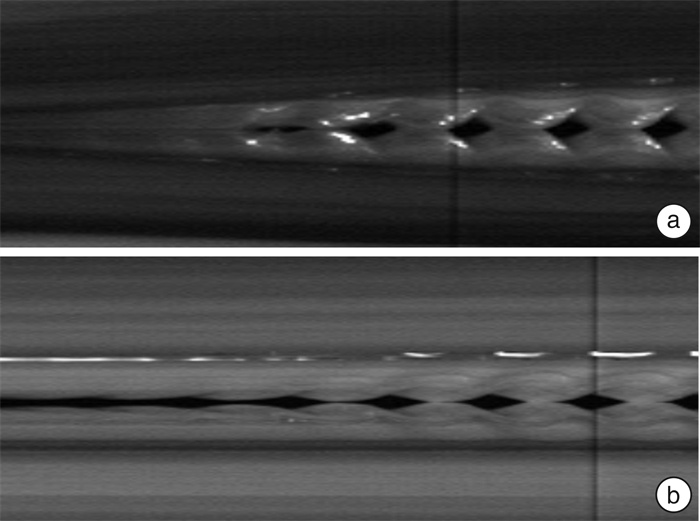
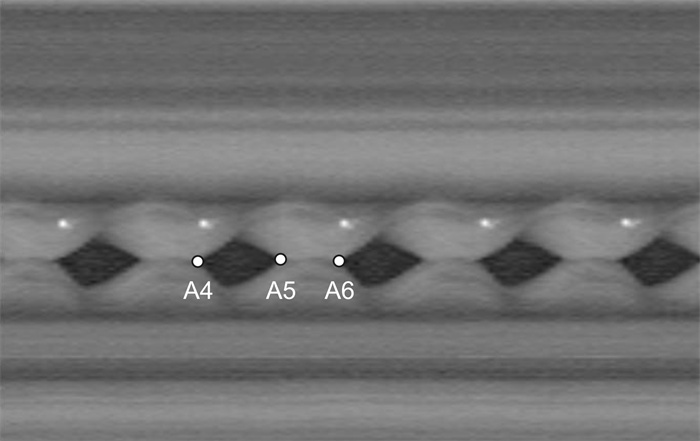
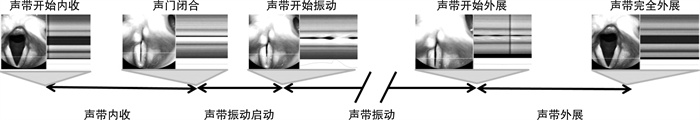
摘要: 目的 咽喉反流(laryngopharyngeal reflux,LPR)患者咽喉部黏膜存在慢性炎症,这些炎症导致咽喉部处于高反应状态,可能会使得声带运动出现过快的表现。本文通过分析LPR患者的喉高速摄影录像,探讨LPR患者的声带运动及发声启动特点。 方法 入选咽喉反流患者40例为LPR组,LPR诊断标准:反流症状指数(RSI)及反流体征评分(RFS)阳性确定疑似LPR;进行客观的口咽部Dx pH监测,Ryan指数阳性提示有反流。根据年龄及性别匹配入选健康志愿者40例为正常对照组。对受试者进行喉高速摄影录像,分析声带运动及振动参数:声带内收时间、声带外展时间、声带振动启动模式(发声启动时间及起音方式)及声带振动周期的开放商。采用SPSS 25.0进行统计学分析。 结果 LPR组声带内收时间(平均225.81 ms)小于对照组(平均277.01 ms)(P<0.05)。LPR组声带两侧的内收时间差与对照组间差异无统计学意义(P>0.05)。LPR组的声带振动启动时间大于对照组(P<0.05)。喉高速摄影下显示LPR组硬起音患者数(17例)多于对照组(8例)(P<0.05)。LPR组声带振动的开放商与对照组的差异无统计学意义(P>0.05)。LPR组的声带外展时间(平均372.92 ms)与对照组(平均426.98 ms)间差异无统计学意义(P>0.05)。LPR组声带两侧外展时间差大于对照组(P<0.05)。 结论 LPR患者声带运动速度较快,且更容易出现硬起音发声模式,导致嗓音功能障碍。Abstract: Objective Patients with Laryngopharyngeal Reflux(LPR) have chronic inflammation of the laryngeal mucosa leading to a high response state in the larynx, which may make the vocal fold movement too fast. This paper discusses the characteristics of vocal fold movement and voice onset by analyzing laryngeal high-speed videoendoscopy in patients with LPR. Methods Forty patients with LPR were enrolled as LPR group. The diagnostic criteria of LPR included positive reflux symptom index(RSI) and reflux syndrome score(RFS) to identify suspected LPR, objective oropharyngeal DX pH monitoring was carried out, and positive Ryan index indicated reflux. According to age and sex matching, 40 healthy volunteers were selected as the normal group. Laryngeal high-speed videoendoscopy, and the vocal fold motion and vibration parameters, including vocal fold adduction time, vocal fold abduction time, vocal fold vibration onset mode(vocal onset time and mode) and the opening quotient of vocal fold vibration cycle. Statistical analysis was performed using SPSS 25.0. Results The time of vocal fold adduction in LPR group(mean 225.81ms) was less than that in normal group(mean 277.01 ms), and the difference was statistically significant(P < 0.05). There was no significant difference in adduction time between LPR group and normal group(P>0.05). The vocal onset time in LPR group was significantly longer than that in normal group(P < 0.05). High speed video endoscope showed that there were 17 patients with hard onset in LPR group and 8 patients with hard onset in normal group, the difference was statistically significant(P < 0.05). There was no significant difference in the open quotient of vocal fold vibration between LPR group and normal group(P>0.05). The vocal fold abduction time in LPR group(mean 372.92 ms) was less than that in normal group(mean 426.98ms), but the difference was not statistically significant(P>0.05). The time difference of bilateral abduction of vocal fold in LPR group was significantly higher than that in normal group(P < 0.05). Conclusion The larynx of LPR patients is in a high response state, the vocal fold moves faster, and it is more likely to have a hard vocal onset. These may result in voice dysfunction.
-

-
[1] 韩悦, 张森, 皇甫辉, 等. 咽喉反流性疾病诊断量表的应用进展[J]. 临床耳鼻咽喉头颈外科杂志, 2023, 37(4): 313-317. https://lceh.whuhzzs.com/article/doi/10.13201/j.issn.2096-7993.2023.04.016
[2] Lechien JR, Khalife M, Huet K, et al. Perceptual, aerodynamic, and acoustic characteristics of voice changes in patients with laryngopharyngeal reflux disease[J]. Ear Nose Throat J, 2019, 98(6): e44-e50. doi: 10.1177/0145561319840830
[3] Eubanks TR, Omelanczuk PE, Maronian N, et al. Pharyngeal ph monitoring in 222 patients with suspected laryngeal reflux[J]. J Gastrointest Surg, 2001, 5(2): 183-191. doi: 10.1016/S1091-255X(01)80032-9
[4] 侯渊涛, 孙晓红, 李晓青, 等. 胃食管反流病患者食管动力异常及其对食管酸暴露的影响[J]. 中华内科杂志, 2015, 54(10): 865-869. doi: 10.3760/cma.j.issn.0578-1426.2015.10.010
[5] Kahrilas PJ, Dodds WJ, Hogan WJ, et al. Esophageal peristaltic dysfunction in peptic esophagitis[J]. Gastroenterology, 1986, 91(4): 897-904. doi: 10.1016/0016-5085(86)90692-X
[6] 宋冰, 张文婧, 王翀, 等. 难治性胃食管反流病食管动力异常与反流特点的研究[J]. 胃肠病学和肝病学杂志, 2020, 29(2): 160-164. doi: 10.3969/j.issn.1006-5709.2020.02.008
[7] 李莉, 展玉涛, 郭宝娜, 等. 难治性胃食管反流病不同亚型食管动力异常与反流特点的相关性[J]. 中华消化杂志, 2017, 37(12): 796-800. doi: 10.3760/cma.j.issn.0254-1432.2017.12.002
[8] 计亦旻, 胡晔东, 徐文, 等. 无效食管动力在胃食管反流病中作用的探讨[J]. 国际消化病杂志, 2018, 38(3): 187-190. doi: 10.3969/j.issn.1673-534X.2018.03.009
[9] Martinucci I, de Bortoli N, Giacchino M, et al. Esophageal motility abnormalities in gastroesophageal reflux disease[J]. World J Gastrointest Pharmacol Ther, 2014, 5(2): 86-96. doi: 10.4292/wjgpt.v5.i2.86
[10] Tugtepe H, Tugay M, Bozkurt S, et al. Esophageal smooth muscle reactivity is impaired in chronic reflux esophagitis by both receptor-and nonreceptor-mediated mechanisms[J]. J Pediatr Surg, 2007, 42(4): 641-646. doi: 10.1016/j.jpedsurg.2006.12.048
[11] Katada N, Moriya H, Yamashita K, et al. Laparoscopic antireflux surgery improves esophageal body motility in patients with severe reflux esophagitis[J]. Surg Today, 2014, 44(4): 740-747. doi: 10.1007/s00595-013-0704-4
[12] Meyer GW, Austin RM, Brady CE, et al. Muscle anatomy of the human esophagus[J]. J Clin Gastroenterol, 1986, 8(2): 131-134. doi: 10.1097/00004836-198604000-00005
[13] Erdur O, Gul O, Ozturk K. Evaluation of upper oesophageal sphincter in unilateral vocal fold paralysis[J]. J Laryngol Otol, 2019, 133(2): 149-154. doi: 10.1017/S0022215119000045
[14] Lechien JR, De Vos N, Everard A, et al. Laryngopharyngeal reflux: The microbiota theory[J]. Med Hypotheses, 2021, 146: 110460. doi: 10.1016/j.mehy.2020.110460
[15] Wang AM, Wang G, Huang N, et al. Association between laryngopharyngeal reflux disease and autonomic nerve dysfunction[J]. Eur Arch Otorhinolaryngol, 2019, 276(8): 2283-2287. doi: 10.1007/s00405-019-05482-w
[16] Tubbs RS, Benninger B, Loukas M, et al. Cranial roots of the accessory nerve exist in the majority of adult humans[J]. Clin Anat, 2014, 27(1): 102-107. doi: 10.1002/ca.22125
[17] Yanes-Díaz J, García-López I, Pérez SS, et al. Is immobile vocal fold related to the spinal accessory nerve agenesis?: a case report[J]. J Voice, 2023, 37(5): 799. e13-799. e15. doi: 10.1016/j.jvoice.2021.04.015
[18] 王刚, 王阿敏, 黄宁, 等. 咽喉反流性疾病与自主神经功能障碍的相关性研究[J]. 听力学及言语疾病杂志, 2020, 28(3): 243-247. doi: 10.3969/j.issn.1006-7299.2020.03.002
[19] Park CH, Lee YT, Yi YB, et al. Ability of high-resolution manometry to determine feeding method and to predict aspiration pneumonia in patients with dysphagia[J]. Am J Gastroenterol, 2017, 112(7): 1074-1083. doi: 10.1038/ajg.2017.81
[20] Vance D, Heyd C, Pier M, et al. Paradoxical vocal fold movement: a retrospective analysis[J]. J Voice, 2021, 35(6): 927-929. doi: 10.1016/j.jvoice.2020.04.007
[21] Amberger P. Paradoxical vocal fold motion, a real breathing problem: diagnosis and treatment[J]. Rev Med Suisse, 2017, 13(570): 1390-1392.
[22] Holley D, Mendez A, Donald C. Paroxysmal laryngospasm: Episodic closure of the upper airway[J]. JAAPA, 2019, 32(2): 31-34. doi: 10.1097/01.JAA.0000552724.72939.4c
[23] 郑杰元, 张立红, 李晶兢, 等. 咽喉反流症状指数量表中文版的信度及效度评价[J]. 中华耳鼻咽喉头颈外科杂志, 2012, 47(11): 894-898. doi: 10.3760/cma.j.issn.1673-0860.2012.11.004
[24] Iwahashi T, Ogawa M, Hosokawa K, et al. A detailed motion analysis of the angular velocity between the vocal folds during throat clearing using high-speed digital imaging[J]. J Voice, 2016, 30(6): 770. e1-770. e8. doi: 10.1016/j.jvoice.2015.11.004
[25] Baken RJ, Watson BC. Research note: vocal attack time-extended analysis[J]. J Voice, 2019, 33(3): 258-262. doi: 10.1016/j.jvoice.2017.12.014
[26] Xu XL, Huang XQ, Tan JJ, et al. The effects of hard voice onset on objective voice function in patients with laryngopharyngeal reflux[J]. J Voice, 2022: S0892-S1997(22)00066-2.
[27] Lechien JR, Saussez S, Nacci A, et al. Association between laryngopharyngeal reflux and benign vocal folds lesions: a systematic review[J]. Laryngoscope, 2019, 129(9): e329-e341.
[28] Lechien JR, Saussez S, Harmegnies B, et al. Laryngopharyngeal reflux and voice disorders: a multifactorial model of etiology and pathophysiology[J]. J Voice, 2017, 31(6): 733-752. doi: 10.1016/j.jvoice.2017.03.015
[29] Johnston N, Wells CW, Blumin JH, et al. Receptor-mediated uptake of pepsin by laryngeal epithelial cells[J]. Ann Otol Rhinol Laryngol, 2007, 116(12): 934-938. doi: 10.1177/000348940711601211
[30] Arslan H, Çandar T, Kuran S, et al. New inflammatory parameters in laryngopharyngeal reflux[J]. J Laryngol Otol, 2016, 130(9): 878-882. doi: 10.1017/S0022215116008653
[31] Lechien JR, Finck C, Costa de Araujo P, et al. Voice outcomes of laryngopharyngeal reflux treatment: a systematic review of 1483 patients[J]. Eur Arch Otorhinolaryngol, 2017, 274(1): 1-23. doi: 10.1007/s00405-016-3984-7
[32] Shock LA, Gallemore BC, Hinkel CJ, et al. Improving the utility of laryngeal adductor reflex testing: a translational tale of mice and men[J]. Otolaryngol Head Neck Surg, 2015, 153(1): 94-101. doi: 10.1177/0194599815578103
[33] Strohl MP, Chang JL, Dwyer CD, et al. Laryngeal adductor reflex movement latency following tactile stimulation[J]. Otolaryngol Head Neck Surg, 2022, 166(4): 720-726. doi: 10.1177/01945998211025517
[34] Shiba TL, Chhetri DK. Dynamics of phonatory posturing at phonation onset[J]. Laryngoscope, 2016, 126(8): 1837-1843. doi: 10.1002/lary.25816
[35] Watson BC, Baken RJ, Roark RM. Effect of voice onset type on vocal attack time[J]. J Voice, 2016, 30(1): 11-14. doi: 10.1016/j.jvoice.2014.12.004
[36] Lohscheller J, Svec JG, Döllinger M. Vocal fold vibration amplitude, open quotient, speed quotient and their variability along glottal length: kymographic data from normal subjects[J]. Logoped Phoniatr Vocol, 2013, 38(4): 182-192. doi: 10.3109/14015439.2012.731083
[37] Nakagawa H, Fukuda H, Kawaida M, et al. Lubrication mechanism of the larynx during phonation: an experiment in excised canine larynges[J]. Folia Phoniatr Logop, 1998, 50(4): 183-194. doi: 10.1159/000021460
[38] 郑念东, 刘江涛, 姜琳琳, 等. 咽喉反流在窄带成像下的特征性表现[J]. 临床耳鼻咽喉头颈外科杂志, 2023, 37(10): 804-808. https://lceh.whuhzzs.com/article/doi/10.13201/j.issn.2096-7993.2023.10.008
-




 下载:
下载: