The correlation between preoperative neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio and postoperative recurrence of chronic rhinosinusitis
-
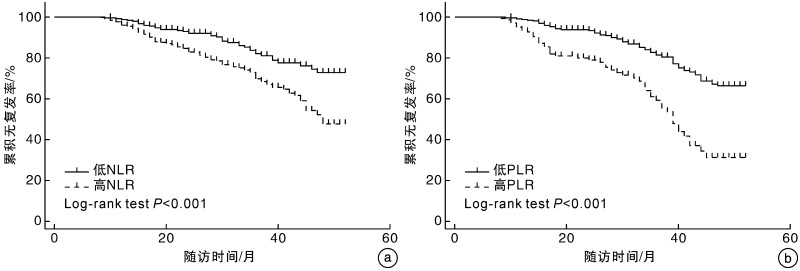
摘要: 目的 探讨术前中性粒细胞与淋巴细胞比值(neutrophil-to-lymphocyte ratio,NLR)和血小板与淋巴细胞比值(platelet-to-lymphocyte ratio,PLR)与慢性鼻窦炎(CRS)术后复发风险的相关性。 方法 收集2018年10月-2022年2月在河南大学淮河医院耳鼻咽喉头颈外科初次行功能性内镜鼻窦手术的CRS患者临床资料。随访至2023年2月,研究终点定义为患者术后复发或随访时间截止。根据受试者工作曲线分析获得术前NLR和PLR最佳临界值,分别将其分为高、低水平亚组,并比较组间患者的临床特征及术后复发率; 根据患者术后复发情况将患者分为未复发CRS和复发CRS,采用Kaplan-Meier生存曲线和logistic回归分析探讨NLR和PLR与CRS术后复发的相关性。 结果 共纳入630例CRS患者,其中高NLR组382例,高PLR组140例。高NLR组和高PLR组CRS患者的术后复发率分别显著高于低NLR组和低PLR组,差异有统计学意义(P<0.05)。复发CRS的NLR、PLR水平和高NLR、高PLR比例均高于未复发CRS,差异有统计学意义(P<0.05),同样复发CRS的病程和变应性鼻炎(AR)伴发率均显著高于未复发CRS,差异有统计学意义(P<0.05)。Kaplan-Meier生存曲线显示,高NLR组和高PLR组CRS较低NLR组和低PLR组术后复发率显著上升,差异有统计学意义(P<0.05)。此外,logistic回归分析显示,高NLR组、高PLR组的病程和合并AR与CRS术后复发风险增加显著相关,差异有统计学意义(P<0.05)。 结论 术前高NLR和高PLR均是CRS术后复发的独立危险因素,其有望成为CRS患者术后预后评估和风险分层的新指标。此外,病程和合并AR与CRS术后复发风险显著相关。
-
关键词:
- 慢性鼻窦炎 /
- 中性粒细胞与淋巴细胞比值 /
- 血小板与淋巴细胞比值 /
- 手术 /
- 复发
Abstract: Objective Neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) play important roles in the poor prognosis of different inflammatory and neoplastic diseases, but their effects on postoperative recurrence of chronic rhinosinusitis(CRS) are unknown. The aim of this study was to investigate the correlation between preoperative NLR and PLR and the risk of postoperative recurrence in CRS. Methods Clinical data were collected from patients with CRS who underwent initial functional endoscopic sinus surgery from October 2018 to February 2022 at our institution. Follow-up was until February 2023, and the study endpoint was defined as patient postoperative recurrence or follow-up time up to date. The optimal preoperative NLR and PLR threshold values were obtained based on subject work curve analysis, and they were divided into high and low level subgroups, respectively, and the clinical characteristics and postoperative recurrence rates of patients were compared between groups; patients were divided into non-recurrent CRS and recurrent CRS according to their postoperative recurrence, and Kaplan-Meier survival curves and logistic regression analysis were performed to explore the correlation between NLR and PLR and CRS The correlation between NLR and PLR and postoperative recurrence was investigated by Kaplan-Meier survival curve and logistic regression analysis. Results A total of 630 patients with CRS were included, including 382 and 140 patients with high NLR and high PLR, respectively. The postoperative recurrence rates of CRS patients in the high NLR and high PLR groups were significantly higher than those in the low NLR and low PLR groups(P < 0.05). The recurrent CRS had higher NLR and PLR levels and higher proportion of high NLR and high PLR than the non-recurrent CRS(P < 0.05), and similarly the duration of recurrent CRS and the rate of allergic rhinitis with recurrence were significantly higher than the non-recurrent CRS(P < 0.05). Kaplan-Meier survival curves showed that postoperative CRS was significantly higher in the high NLR and high PLR groups compared with the low NLR and low PLR groups. recurrence was significantly higher(P < 0.05). In addition, logistic regression analysis showed that high NLR, high PLR, disease duration, and combined allergic rhinitis were significantly associated with an increased risk of postoperative recurrence of CRS(P < 0.05). Conclusion Both high preoperative NLR and high PLR are independent risk factors for postoperative recurrence of CRS, and they are expected to be new indicators for postoperative prognostic assessment and risk stratification of CRS patients. In addition, disease duration and comorbid allergic rhinitis were significantly associated with the risk of postoperative recurrence of CRS. -

-
表 1 纳入患者的临床特征
变量 数值 患者例数 630 年龄/岁 45.0(32.0~55.0) 男/例(%) 428(67.9) 吸烟/例(%) 108(17.1) 饮酒/例(%) 46(7.3) BMI/kg/m2 23.0(20.9~25.7) 病程/月 24.0(6.0~72.5) 糖尿病/例(%) 68(10.8) 高血压病/例(%) 110(17.5) AR/例(%) 168(26.7) 哮喘/例(%) 60(9.5) NLR 1.8(1.4~2.4) NLR>1.65/例(%) 382(60.6) PLR 113.4(89.3~144.4) PLR>149.75/例(%) 140(22.2) CRS表型/例(%) CRSsNP 129 (20.5) CRSwNP 501 (79.5) 复发性CRS/例(%) 141 (22.4) 随访时间/月 29.0 (23.0~39.0) 表 2 低NLR组与高NLR组CRS患者的临床特征比较
变量 低NLR组(n=248) 高NLR组(n=382) P 年龄/岁 42.0(31.0~54.0) 46.0(32.0~55.5) 0.059 男/例(%) 165(66.5) 263(68.8) 0.849 吸烟/例(%) 44(17.7) 64(16.8) 0.913 饮酒/例(%) 14(5.7) 33(8.6) 0.162 BMI/kg/m2 23.0(20.7~24.3) 23.0(21.1~25.6) 0.988 病程/月 24.0(12.0~84.0) 24.0(6.0~72.0) 0.180 糖尿病/例(%) 18(7.3) 50(13.1) 0.021 高血压病/例(%) 42(16.9) 68(17.8) 0.780 收缩压/mmHg 125.0(115.1~137.6) 126.1(116.0~136.0) 0.402 舒张压/mmHg 79.0(73.0~86.0) 80.0(72.8~87.0) 0.853 AR/例(%) 87(35.1) 81(21.2) <0.001 哮喘/例(%) 32(12.9) 28(7.3) 0.020 CRS表型/例(%) 0.008 CRSsNP 64(25.8) 65(17.0) CRSwNP 184(74.2) 317(83.0) 复发性CRS/例(%) 40(16.1) 101(26.4) 0.002 表 3 低PLR组与高PLR组CRS患者的临床特征比较
变量 低PLR(n=490) 高PLR(n=140) P 年龄/岁 45.0(31.0~55.0) 46.0(32.0~55.5) 0.192 男/例(%) 334(68.2) 94(67.1) 0.923 吸烟/例(%) 82(16.7) 26(18.6) 0.611 饮酒/例(%) 32(6.5) 15(10.7) 0.097 BMI/kg/m2 23.0(20.8~25.3) 22.8(20.8~25.2) 0.549 病程/月 24.5(6.0~71.0) 24.0(6.5~84.0) 0.770 糖尿病/例(%) 43(8.8) 25(17.9) 0.002 高血压病/例(%) 89(18.2) 21(15.0) 0.385 AR/例(%) 134(27.4) 34(24.3) 0.470 哮喘/例(%) 51(10.4) 9(6.4) 0.157 CRS表型/例(%) <0.001 CRSsNP 115(23.5) 14(10.0) CRSwNP 375(76.5) 126(90.0) 复发性CRS/例(%) 88(18.0) 53(37.9) <0.001 表 4 未复发CRS组与复发CRS组患者的临床特征比较
变量 未复发CRS(n=489) 复发CRS(n=141) P 年龄/岁 44.0(31.0~55.0) 47.0(32.5~55.5) 0.174 男/例(%) 327(66.9) 101(71.6) 0.286 吸烟/例(%) 82(16.8) 26(18.4) 0.643 饮酒/例(%) 33(6.8) 14(9.9) 0.205 BMI/kg/m2 22.9(20.7~25.4) 23.5(21.2~25.9) 0.202 病程/月 24.0(6.0~60.0) 36.5(11.5~117.5) <0.001 糖尿病/例(%) 48(9.8) 20(14.2) 0.141 高血压病/例(%) 86(17.6) 24(17.0) 0.876 AR/例(%) 121(24.7) 47(33.3) 0.042 哮喘/例(%) 43(8.8) 17(12.1) 0.245 高NLR/例(%) 281(57.5) 101(71.6) 0.002 NLR 1.8(1.4~2.4) 1.9(1.6~3.0) 0.001 高PLR/例(%) 87(17.8) 53(37.6) <0.001 PLR 110.1(88.4~137.0) 126.2(91.1~186.1) <0.001 CRS表型/例(%) 0.359 CRSsNP 104(21.3) 25(17.7) CRSwNP 385(78.7) 116(82.3) 表 5 影响CRS患者术后复发的多因素logistic回归分析
变量 OR 95%CI P 病程 1.004 1.002~1.007 <0.001 AR 有 1.742 1.131~2.684 0.012 无 1.000 高NLR 有 1.731 1.107~2.706 0.016 无 1.000 高PLR 有 2.498 1.611~3.872 <0.001 无 1.000 -
[1] 王晓燕, 孟一帆, 王成硕, 等. 慢性鼻窦炎钩突内外侧面黏膜组织病理学差异[J]. 临床耳鼻咽喉头颈外科杂志, 2022, 36(2): 95-100. https://lceh.whuhzzs.com/article/doi/10.13201/j.issn.2096-7993.2022.02.004
[2] 中华耳鼻咽喉头颈外科杂志编辑委员会鼻科组, 中华医学会耳鼻咽喉头颈外科学分会鼻科学组. 中国慢性鼻窦炎诊断和治疗指南(2018)[J]. 中华耳鼻咽喉头颈外科杂志, 2019, 54(2): 81-100.
[3] 贺星华, 李静波, 王俊杰, 等. 鼻内镜术后慢性鼻窦炎患者主观症状缓解效果与负面情绪状态的关系研究[J]. 中国耳鼻咽喉头颈外科, 2022, 29(11): 721-723.
[4] Bachert C, Marple B, Schlosser RJ, et al. Adult chronic rhinosinusitis[J]. Nat Rev Dis Primers, 2020, 6(1): 86. doi: 10.1038/s41572-020-00218-1
[5] Shi JB, Fu QL, Zhang H, et al. Epidemiology of chronic rhinosinusitis: results from a cross-sectional survey in seven Chinese cities[J]. Allergy, 2015, 70(5): 533-539. doi: 10.1111/all.12577
[6] 张罗. 生物制剂治疗慢性鼻窦炎鼻息肉的现状和展望[J]. 临床耳鼻咽喉头颈外科杂志, 2023, 37(11): 853-855. https://lceh.whuhzzs.com/article/doi/10.13201/j.issn.2096-7993.2023.11.001
[7] 史慕寒, 王冲, 王旻, 等. 慢性鼻窦炎术后复发额窦炎患者额隐窝气房残留情况的影像及再手术结果分析[J]. 首都医科大学学报, 2022, 43(6): 911-918.
[8] Kohanski MA, Toskala E, Kennedy DW. Evolution in the surgical management of chronic rhinosinusitis: Current indications and pitfalls[J]. J Allergy Clin Immunol, 2018, 141(5): 1561-1569. doi: 10.1016/j.jaci.2018.03.003
[9] Veloso-Teles R, Cerejeira R. Endoscopic sinus surgery for chronic rhinosinusitis with nasal polyps: Clinical outcome and predictive factors of recurrence[J]. Am J Rhinol Allergy, 2017, 31(1): 56-62. doi: 10.2500/ajra.2017.31.4402
[10] Bai J, Huang JH, Price C, et al. Prognostic factors for polyp recurrence in chronic rhinosinusitis with nasal polyps[J]. J Allergy Clin Immunol, 2022, 150(2): 352-361. e7. doi: 10.1016/j.jaci.2022.02.029
[11] El-Gazzar AG, Kamel MH, Elbahnasy O, et al. Prognostic value of platelet and neutrophil to lymphocyte ratio in COPD patients[J]. Expert Rev Respir Med, 2020, 14(1): 111-116. doi: 10.1080/17476348.2019.1675517
[12] Enersen CC, Egelund GB, Petersen PT, et al. The ratio of neutrophil-to-lymphocyte and platelet-to-lymphocyte and association with mortality in community-acquired pneumonia: a derivation-validation cohort study[J]. Infection, 2023, 51(5): 1339-1347. doi: 10.1007/s15010-023-01992-2
[13] Li H, Song J, Cao M, et al. Preoperative neutrophil-to-lymphocyte ratio is a more valuable prognostic factor than platelet-to-lymphocyte ratio for nonmetastatic rectal cancer[J]. Int Immunopharmacol, 2016, 40: 327-331. doi: 10.1016/j.intimp.2016.09.014
[14] Zhu Y, Zhou S, Liu Y, et al. Prognostic value of systemic inflammatory markers in ovarian Cancer: a PRISMA-compliant meta-analysis and systematic review[J]. BMC Cancer, 2018, 18(1): 443. doi: 10.1186/s12885-018-4318-5
[15] Wang JH, Chen YY, Kee KM, et al. The Prognostic Value of Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio in Patients with Hepatocellular Carcinoma Receiving Atezolizumab Plus Bevacizumab[J]. Cancers(Basel), 2022, 14(2): 343.
[16] Kang J, Chang Y, Ahn J, et al. Neutrophil-to-lymphocyte ratio and risk of lung cancer mortality in a low-risk population: A cohort study[J]. Int J Cancer, 2019, 145(12): 3267-3275. doi: 10.1002/ijc.32640
[17] 张正强, 杜军, 单智慧. 慢性鼻-鼻窦炎手术预后的相关因素分析[J]. 中国耳鼻咽喉颅底外科杂志, 2016, 22(6): 510-512.
[18] Kato A, Schleimer RP, Bleier BS. Mechanisms and pathogenesis of chronic rhinosinusitis[J]. J Allergy Clin Immunol, 2022, 149(5): 1491-1503. doi: 10.1016/j.jaci.2022.02.016
[19] Ogulur I, Pat Y, Ardicli O, et al. Advances and highlights in biomarkers of allergic diseases[J]. Allergy, 2021, 76(12): 3659-3686. doi: 10.1111/all.15089
[20] Ambrosino P, Molino A, Spedicato GA, et al. Nasal Nitric Oxide in Chronic Rhinosinusitis with or without Nasal Polyps: A Systematic Review with Meta-Analysis[J]. J Clin Med, 2020, 9(1): 200. doi: 10.3390/jcm9010200
[21] Klingler AI, Stevens WW, Tan BK, et al. Mechanisms and biomarkers of inflammatory endotypes in chronic rhinosinusitis without nasal polyps[J]. J Allergy Clin Immunol, 2021, 147(4): 1306-1317. doi: 10.1016/j.jaci.2020.11.037
[22] Yuan T, Zheng R, Liu J, et al. Role of yes-associated protein in interleukin-13 induced nasal remodeling of chronic rhinosinusitis with nasal polyps[J]. Allergy, 2021, 76(2): 600-604. doi: 10.1111/all.14699
[23] Kato A, Peters AT, Stevens WW, et al. Endotypes of chronic rhinosinusitis: Relationships to disease phenotypes, pathogenesis, clinical findings, and treatment approaches[J]. Allergy, 2022, 77(3): 812-826. doi: 10.1111/all.15074
[24] Eschenbacher W, Kim M, Mattos J, et al. Activation of platelet-adherent basophils in chronic rhinosinusitis with alcohol hypersensitivity[J]. Ann Allergy Asthma Immunol, 2022, 128(4): 443-450. doi: 10.1016/j.anai.2022.01.013
[25] Succar EF, Li P, Ely KA, et al. Neutrophils are underrecognized contributors to inflammatory burden and quality of life in chronic rhinosinusitis[J]. Allergy, 2020, 75(3): 713-716. doi: 10.1111/all.14071
[26] Shaghayegh G, Cooksley C, Ramezanpour M, et al. Chronic Rhinosinusitis, S. aureus Biofilm and Secreted Products, Inflammatory Responses, and Disease Severity[J]. Biomedicines, 2022, 10(6): 1362. doi: 10.3390/biomedicines10061362
[27] Jin J, Guo B, Zhang W, et al. Diagnostic value of myeloperoxidase and eosinophil cationic protein in nasal secretions for endotypes of chronic rhinosinusitis[J]. Eur Arch Otorhinolaryngol, 2023, 280(8): 3707-3720. doi: 10.1007/s00405-023-07903-3
[28] Kim DK, Lim HS, Eun KM, et al. Subepithelial neutrophil infiltration as a predictor of the surgical outcome of chronic rhinosinusitis with nasal polyps[J]. Rhinology, 2021, 59(2): 173-180.
[29] Chen X, Chang L, Li X, et al. Tc17/IL-17A Up-Regulated the Expression of MMP-9 via NF-κB Pathway in Nasal Epithelial Cells of Patients With Chronic Rhinosinusitis[J]. Front Immunol, 2018, 9: 2121. doi: 10.3389/fimmu.2018.02121
[30] Li T, Yang Y, Li Y, et al. Platelets mediate inflammatory monocyte activation by SARS-CoV-2 spike protein[J]. J Clin Invest, 2022, 132(4): e150101. doi: 10.1172/JCI150101
[31] Hottz ED, Azevedo-Quintanilha IG, Palhinha L, et al. Platelet activation and platelet-monocyte aggregate formation trigger tissue factor expression in patients with severe COVID-19[J]. Blood, 2020, 136(11): 1330-1341. doi: 10.1182/blood.2020007252
[32] Lin H, Lin D, Xiong XS, et al. Role of platelet-derived growth factor-α in eosinophilic and non-eosinophilic chronic rhinosinusitis with nasal polyps[J]. Int Forum Allergy Rhinol, 2014, 4(11): 909-914. doi: 10.1002/alr.21419
[33] Pongdee T, Bielinski SJ, Decker PA, et al. White blood cells and chronic rhinosinusitis: a Mendelian randomization study[J]. Allergy Asthma Clin Immunol, 2022, 18(1): 98. doi: 10.1186/s13223-022-00739-2
[34] Zinellu A, Zinellu E, Mangoni AA, et al. Clinical significance of the neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in acute exacerbations of COPD: present and future[J]. Eur Respir Rev, 2022, 31(166): 220095. doi: 10.1183/16000617.0095-2022
[35] Xie S, Jiang S, Fan R, et al. Elevated body mass index increased the risk of recurrence in Chinese patients with chronic rhinosinusitis[J]. Am J Otolaryngol, 2023, 44(4): 103841. doi: 10.1016/j.amjoto.2023.103841
[36] Striz I, Golebski K, Strizova Z, et al. New insights into the pathophysiology and therapeutic targets of asthma and comorbid chronic rhinosinusitis with or without nasal polyposis[J]. Clin Sci(Lond), 2023, 137(9): 727-753. doi: 10.1042/CS20190281
[37] 齐岩, 刘俊其, 彭舒娅, 等. 鼻内镜下选择性翼管神经切断术对伴有变应性鼻炎的慢性鼻窦炎的疗效观察[J]. 山东大学耳鼻喉眼学报, 2019, 33(1): 109-113.
-




 下载:
下载: