Granulomatosis with polyangiitis with head and neck symptoms as the first clinical manifestation: clinical analysis of 28 cases
-
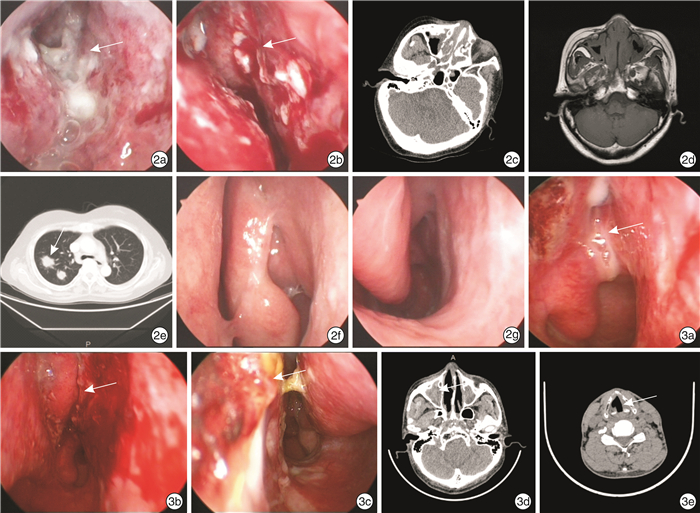
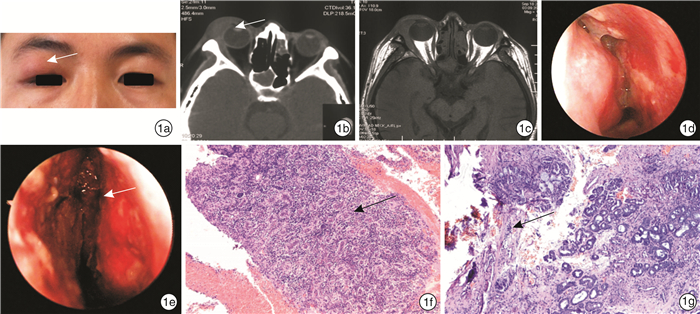
摘要: 目的 探讨以头颈部症状为首发的肉芽肿性多血管炎(GPA)的早期临床特征及诊断。方法 收集2014—2021年就诊于山西医科大学第二医院、首发症状出现于头颈部并确诊为GPA的28例患者资料。所有患者均行相关的影像学检查、实验室检查、内镜检查及病理组织活检。行全身糖皮质激素或联合免疫抑制剂治疗,随访1~5年。结果 2例患者拒绝治疗失访;26例患者出院时症状好转,诉鼻腔通气可,眶上肿物消退,呼吸困难和肾脏症状减轻。5例患者因出现肾脏受累病情反复多次入院治疗。结论 GPA虽常以头颈部症状为首发,但无特异性,易与慢性炎症性疾病混淆,造成误诊。如发现可疑病例,应尽早结合内镜检查、病理组织活检及特异实验室检查以获得早期诊断和治疗。Abstract: Objective To investigate the early clinical features and diagnosis of granulomatous polyangiitis(GPA) with head and neck symptoms as the first presentation.Methods The data of 28 patients with GPA diagnosed in the Second Hospital of Shanxi Medical University from 2014 to 2021, whose first symptoms appeared on the head and neck, were collected. All patients underwent relevant imaging examinations, laboratory tests, endoscopy, and pathological tissue biopsies. Systemic glucocorticoid or combined immunosuppressive therapy was administered and followed up for 1-5 years.Results Two patients refused treatment and were lost to follow-up; 26 patients were discharged with improved symptoms, complaining of nasal ventilation, resolution of supraorbital swelling, reduced dyspnoea, and renal symptoms. Five patients were repeatedly admitted to the hospital due to recurrent renal involvement.Conclusion Although GPA often begins with head and neck symptoms, it is non-specific and can easily be confused with chronic inflammatory disease, leading to misdiagnosis. If suspicious cases are identified, they should be combined with endoscopy, pathological tissue biopsy, and special laboratory tests as early as possible to shorten the time to diagnosis, and obtain early diagnosis and treatment.
-
Key words:
- granulomatosis with polyangiitis /
- nasal endoscope /
- diagnosis /
- prognosis
-

-
表 1 首发症状及伴随症状
症状 例数(%) 首发症状 间断双侧鼻塞 12(42.86) 听力下降伴耳闷 7(25.00) 反复眼部红肿疼痛 5(17.86) 持续双侧鼻塞 4(14.29) 声音嘶哑伴呼吸困难 2(7.14) 伴随症状 视力下降(失明1例) 15(53.57) 反复眼睑红肿(手术2例) 15(53.57) 流脓涕 14(50.00) 泌尿系统症状(蛋白尿、血尿、夜尿增多等) 13(46.43) 呼吸系统症状(咳嗽、咳痰、喘息等) 12(42.86) 发热 9(32.14) 双耳听力下降 9(32.14) 咽部异物感 8(28.57) 耳闷(鼓膜切开置管术5例) 8(28.57) 气紧 6(21.43) 双耳交替性反复听力下降 6(21.43) 涕中带血 5(17.86) 痰中带血 5(17.86) 反复鼻出血 4(14.29) 声音嘶哑 4(14.29) 流清涕 3(10.71) 鞍鼻畸形 1(3.57) -
[1] 李菁, 田新平. 2016年美国风湿病学会年会血管炎速递[J]. 中华风湿病学杂志, 2017, 21(4): 286-288. doi: 10.3760/cma.j.issn.1007-7480.2017.04.019
[2] Kitching AR, Anders HJ, Basu N, et al. ANCA-associated vasculitis[J]. Nat Rev Dis Primers, 2020, 6(1): 71. doi: 10.1038/s41572-020-0204-y
[3] Gao LY, Ding J, Zhao LI. Clinicopathologic characteristics of Weneger's granulomatosis: A report of three cases[J]. Exp Ther Med, 2016, 11(4): 1340-1344. doi: 10.3892/etm.2016.3046
[4] Felicetti M, Cazzador D, Padoan R, et al. Ear, nose and throat involvement in granulomatosis with polyangiitis: how it presents and how it determines disease severity and long-term outcomes[J]. Clin Rheumatol, 2018, 37(4): 1075-1083. doi: 10.1007/s10067-018-4019-0
[5] Jeong SM, Park JH, Lee JI, et al. Progressive Bilateral Facial Palsy as a Manifestation of Granulomatosis With Polyangiitis: A Case Report[J]. Ann Rehabil Med, 2016, 40(4): 734-740. doi: 10.5535/arm.2016.40.4.734
[6] Fokkens WJ, Lund VJ, Hopkins C, et al. European Position Paper on Rhinosinusitis and Nasal Polyps 2020[J]. Rhinology, 2020, 58(Suppl S29): 1-464.
[7] Coordes A, Loose SM, Hofmann VM, et al. Saddle nose deformity and septal perforation in granulomatosis with polyangiitis[J]. Clin Otolaryngol, 2018, 43(1): 291-299. doi: 10.1111/coa.12977
[8] Rahne T, Clauß F, Plontke SK, et al. Prevalence of hearing impairment in patients with rheumatoid arthritis, granulomatosis with polyangiitis(GPA, Wegener's granulomatosis), or systemic lupus erythematosus[J]. Clin Rheumatol, 2017, 36(7): 1501-1510. doi: 10.1007/s10067-017-3651-4
[9] Greco A, Marinelli C, Fusconi M, et al. Clinic manifestations in granulomatosis with polyangiitis[J]. Int J Immunopathol Pharmacol, 2016, 29(2): 151-159. doi: 10.1177/0394632015617063
[10] Blackabey V, Gan R, Buglass H, et al. Granulomatosis with polyangiitis causing subglottic stenosis-two cases and their management[J]. AME Case Rep, 2018, 2: 17. doi: 10.21037/acr.2018.03.01
[11] 陈迪, 闵寒毅, 赵久良, 等. 肉芽肿性多血管炎患者眼部表现临床分析[J]. 中华全科医师杂志, 2016, 15(7): 539-542. doi: 10.3760/cma.j.issn.1671-7368.2016.07.011
[12] Lakhani DA, Balar AB, Adelanwa A, et al. Granulomatosis with polyangiitis: A case report and brief review of literature[J]. Radiol Case Rep, 2021, 16(11): 3445-3450. doi: 10.1016/j.radcr.2021.08.028
[13] Feragalli B, Mantini C, Sperandeo M, et al. The lung in systemic vasculitis: radiological patterns and differential diagnosis[J]. Br J Radiol, 2016, 89(1061): 20150992. doi: 10.1259/bjr.20150992
[14] 何权瀛. 韦格纳肉芽肿病的诊断与治疗[J]. 临床内科杂志, 2020, 37(10): 693-695. doi: 10.3969/j.issn.1001-9057.2020.10.005
[15] Binda V, Moroni G, Messa P. ANCA-associated vasculitis with renal involvement[J]. J Nephrol, 2018, 31(2): 197-208. doi: 10.1007/s40620-017-0412-z
[16] Dagostin MA, Nunes S, Shinjo SK, et al. Mortality predictors in ANCA-associated vasculitis: Experience of a Brazilian monocentric cohort of a rheumatology center[J]. Medicine(Baltimore), 2021, 100(51): e28305.
[17] Ramponi G, Folci M, De Santis M, et al. The biology, pathogenetic role, clinical implications, and open issues of serum anti-neutrophil cytoplasmic antibodies[J]. Autoimmun Rev, 2021, 20(3): 102759. doi: 10.1016/j.autrev.2021.102759
[18] Su F, Xiao W, Yang P, et al. Anti-neutrophil cytoplasmic antibodies in new-onset systemic lupus erythematosus[J]. An Bras Dermatol, 2017, 92(4): 466-469. doi: 10.1590/abd1806-4841.20175476
[19] Yoo J, Ahn SS, Jung SM, et al. Should nasal biopsy inevitably be performed for classifying granulomatosis with polyangiitis in patients with rhinosinusitis? A retrospective chart review study[J]. Rheumatol Int, 2019, 39(5): 885-892. doi: 10.1007/s00296-019-04282-z
[20] 闫利娟, 朱剑. 肉芽肿性多血管炎临床病理特点并文献复习[J]. 外科研究与新技术, 2016, 5(1): 44-48. https://www.cnki.com.cn/Article/CJFDTOTAL-TJYE201601018.htm
[21] Coates ML, Martinez Del Pero M. Updates in antineutrophil cytoplasmic antibody(ANCA)-associated vasculitis for the ENT surgeon[J]. Clin Otolaryngol, 2020, 45(3): 316-326. doi: 10.1111/coa.13524
[22] Yates M, Watts RA, Bajema IM, et al. EULAR/ERA-EDTA recommendations for the management of ANCA-associated vasculitis[J]. Ann Rheum Dis, 2016, 75(9): 1583-1594. doi: 10.1136/annrheumdis-2016-209133
[23] Jennette JC, Nachman PH. ANCA Glomerulonephritis and Vasculitis[J]. Clin J Am Soc Nephrol, 2017, 12(10): 1680-1691. doi: 10.2215/CJN.02500317
[24] Choi ST, Ahn SV, Lee PH, et al. The cancer risk according to three subtypes of ANCA-associated vasculitis: A propensity score-matched analysis of a nationwide study[J]. Semin Arthritis Rheum, 2021, 51(4): 692-699. doi: 10.1016/j.semarthrit.2021.03.014
-




 下载:
下载: