-
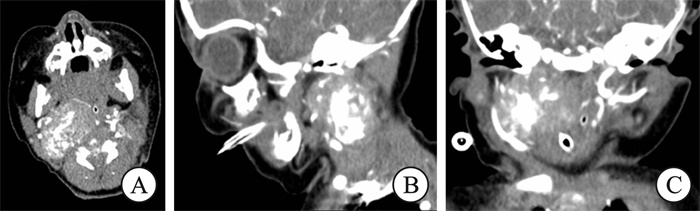
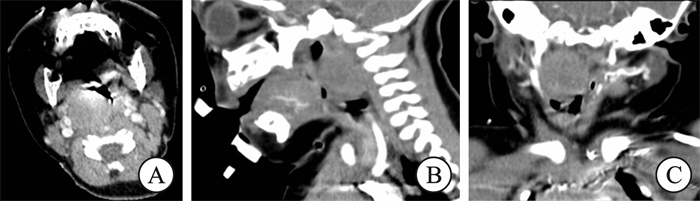
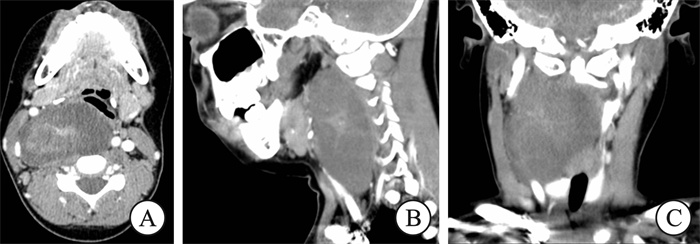
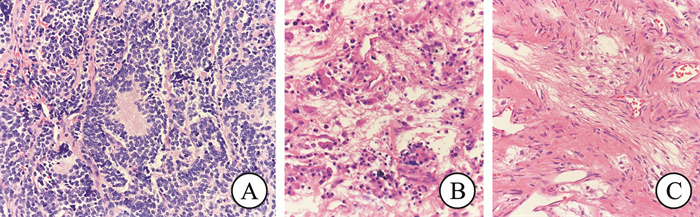
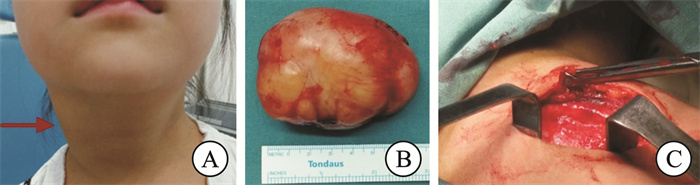
摘要: 目的 探讨儿童原发于颈部的神经母细胞瘤的临床特点、诊断、治疗、病理分型以及预后。 方法 回顾性分析2015年4月-2022年4月上海市儿童医院耳鼻咽喉头颈外科收治的11例原发于颈部神经母细胞瘤患儿的临床资料,分析其临床表现、影像学表现、病理类型、治疗方法及预后等特点,并结合文献进行讨论。 结果 11例患儿中男3例,女8例,年龄28 d~7岁4个月,中位年龄24个月。肿块位于颈动脉鞘区4例,颈侧肌间隙4例,咽旁咽后间隙3例。临床表现以无痛性颈部肿块、喉喘鸣为主。其中颈部原发瘤灶伴颈部淋巴结转移3例,伴骨髓转移1例。病理为神经母细胞瘤8例,节细胞神经母细胞瘤3例。本组患儿中7例采用手术联合化疗,2例采用手术联合放化疗,2例单采用手术治疗。所有病例中7例采用颈侧径路肿物切除术,3例采用经口径路肿物切除术,1例首次手术采用经口径路,再次手术时采用颈侧径路。患儿均完成所有治疗,中位随访时间34个月(6~79个月),随访中9例患儿获得完全缓解,2例患儿获得部分缓解,无疾病进展者。 结论 儿童原发于颈部的神经母细胞瘤起病年龄较小,多以颈部肿物起病,具有高度异质性,内镜辅助经口内入路咽旁间隙肿瘤切除与外径路相比,具有周围组织损伤小、颜面部无瘢痕的优点,为临床提供了一种新的治疗手段。儿童神经母细胞瘤要做到定期随访,形成专病管理,全程精细化管理,以提升患儿的生存质量。Abstract: Objective To explore the clinical manifestations, diagnosis, treatment, pathological types and prognosis of primary cervical neuroblastoma in children. Methods The clinical data of 11 children with primary cervical neuroblastoma admitted to the Department of Otolaryngology and Head and Neck Surgery at Shanghai Children's Hospital from April 2015 to April 2022 were retrospectively analyzed. The clinical characteristics, imaging findings, pathological types, treatment methods, and outcomes of these 11 patients were examined in conjunction with a review of the literature. Results The cohort of 11 neuroblastoma patients ranged in age from 28 days to 88 months (median age: 24 months), including 3 males and 8 females. Among the 11 patients, 4 had tumors located in the carotid sheath area, 4 in the cervical space, and 3 in the parapharyngeal and retropharyngeal spaces. The clinical manifestations primarily included painless cervical masses and laryngeal stridor. There were 3 cases of primary cervical tumors with cervical lymph node metastasis and 1 case with bone marrow metastasis. Pathological findings revealed neuroblastoma in 8 cases and ganglionic neuroblastoma in 3 cases. In this group, 7 patients underwent surgery combined with chemotherapy, 2 patients received surgery combined with chemoradiotherapy, and 2 patients underwent surgery alone. Surgical resection was performed via a cervical approach in 7 cases, while 3 cases were treated using a transoral endoscopic approach. Additionally, one patient underwent a transoral endoscopic approach initially and a cervical approach subsequently. All patients completed their treatment and were followed up regularly, with follow-up durations ranging from 6 to 79 months (median: 34 months). Nine patients achieved complete remission, 2 patients achieved partial remission, and none experienced disease progression. Conclusion Primary cervical neuroblastoma exhibits a high degree of heterogeneity and presents at a younger age, primarily with cervical masses. Compared to external approaches, endoscopy-assisted transoral resection of parapharyngeal tumors offers advantages such as reduced damage to surrounding tissue and no visible neck scars, providing a new method for clinical treatment. Regular follow-up is essential for children with neuroblastoma, along with the establishment of specific disease management protocols and comprehensive care to improve survival quality.
-
Key words:
- neck /
- neuroblastoma /
- ganglionic neuroblastoma /
- parapharyngeal space /
- retropharyngeal space /
- carotid sheath /
- children
-

-
表 1 儿童原发于颈部神经母细胞瘤患儿的临床资料
例序 性别 年龄/月 肿块部位 肿块大小/cm 病理特点 主诉 1 男 1 右侧颈部肌间隙 2.2×2.8×3.6 神经母细胞瘤(差分化) 出生后呼吸困难,加重5 d 2 女 3 右侧咽后壁 2.0×2.0×2.4 神经母细胞瘤(差分化) 喉喘鸣半个月 3 男 10 左侧咽旁间隙 2.5×3.0×3.4 神经母细胞瘤(分化型) 睡眠打鼾伴喘憋2个月 4 女 12 右侧颈动脉鞘区 4.4×2.5×4.2 神经母细胞瘤(分化型) 发现右侧颈部肿块半个月 5 女 17 左侧颈部肌间隙 3.1×4.3×6.1 神经母细胞瘤(差分化) 发现左侧颈部肿块2个月 6 女 24 右侧胸锁乳突肌内侧 6.8×5.7×4.9 神经母细胞瘤(分化型) 发现右侧颈部肿块1年 7 女 45 右侧颈动脉鞘区 4.6×3.3×3.9 神经母细胞瘤(分化型) 发现右侧颈部肿块3个月 8 女 48 左侧颈动脉鞘区 3.0×3.3×4.7 节细胞神经母细胞瘤(混合型) 发现左侧颈部肿块3周 9 女 60 左侧颈部肌间隙 7.0×8.3×4.7 神经母细胞瘤(分化型) 发现左侧颈部肿块半年 10 男 76 左侧颈动脉鞘区 3.0×1.8×3.9 节细胞神经母细胞瘤(混合型) 发现左侧颈部肿块半个月 11 女 88 右侧咽旁间隙 3.0×6.0×7.2 节细胞神经母细胞瘤(结节型) 发现右侧颈部肿块1年 表 2 本组患儿的国际神经母细胞瘤病理学分类(INPC)
例序 形态学分类 预后分类 INSS分期 INRG分期 危险度分层(COG) 1 神经母细胞瘤(差分化) 良好型 Ⅰ L2 低危组 2 神经母细胞瘤(差分化) 良好型 Ⅰ L2 低危组 3 神经母细胞瘤(分化型) 良好型 Ⅰ L1 极低危组 4 神经母细胞瘤(分化型) 良好型 Ⅲ L2 中危组 5 神经母细胞瘤(差分化) 良好型 Ⅳ MS 中危组 6 神经母细胞瘤(分化型) 良好型 ⅡA L2 低危组 7 神经母细胞瘤(分化型) 良好型 ⅡB L2 低危组 8 节细胞神经母细胞瘤(混合型) 良好型 ⅡA L2 极低危组 9 神经母细胞瘤(分化型) 不良型 Ⅲ L2 高危组 10 节细胞神经母细胞瘤(混合型) 良好型 ⅡA L2 极低危组 11 节细胞神经母细胞瘤(结节型) 不良型 Ⅲ L2 中危组 注:原发于颈部的神经母细胞瘤影像学危险因子(IDRFs):肿瘤包绕颈动脉和(或)颈内静脉;肿瘤压迫气管;肿瘤延伸到颅底或胸腔(病例5同时累及颈部与胸腔)。 表 3 儿童原发于颈部神经母细胞瘤患儿的临床分析
临床特征 例数(%) 临床特征 例数(%) 临床特征 例数(%) 年龄 转移情况 手术方式 ≤24个月 6(54.5) 颈淋巴结转移 3(27.3) 颈侧径路 7(63.6) >24个月 5(45.5) 骨髓转移 1(9.1) 经口径路 3(27.3) 首发临床表现 预后分类 经口+颈侧 1(9.1) 颈部肿物 8(72.7) 良好型 9(81.8) 并发症 呼吸困难 3(27.3) 不良型 2(18.2) 肺炎支气管炎 8(72.7) 体征 性别 Horner征 2(18.2) 咽侧咽后壁隆起 5(45.5) 男 3(27.3) 转归 危险度分层 女 8(72.7) CR 9(81.8) 低危极低危组 7(63.6) 儿茶酚胺代谢产物 PR 2(18.2) 中高危组 4(36.4) 尿VMA增高 5(45.5) 治疗模式 尿HVA增高 8(72.7) 手术 2(18.2) 病理分型 手术+化疗 7(63.6) 神经母细胞瘤 8(72.7) 手术+化疗+放疗 2(18.2) 节细胞神经母细胞瘤 3(27.3) 表 4 儿童原发于颈部神经母细胞瘤患儿的治疗与转归
例序 手术方式 治疗过程 并发症 化疗 放疗 随访时间/月 转归 1 颈侧入路 手术-化疗 肺炎 有 无 34 CR 2 经口径路 手术-化疗-手术 肺炎、右侧睑裂小 有 无 28 CR 3 经口径路 手术 无 无 无 6 CR 4 颈侧入路 手术-化疗-手术-放疗 颈淋巴结转移、支气管炎 有 有 9 CR 5 颈侧入路 化疗-手术-化疗 骨髓转移、支气管炎 有 无 6 PR 6 颈侧入路 手术-化疗 支气管炎 有 无 75 CR 7 颈侧入路 手术-化疗 颈淋巴结转移 有 无 79 CR 8 颈侧入路 手术-化疗 支气管炎 有 无 65 CR 9 经口+颈侧 手术-化疗-手术-放疗 肺炎、颈淋巴结转移 有 有 57 PR 10 经口径路 手术 左侧上睑下垂 无 无 10 CR 11 颈侧入路 手术-化疗 支气管炎 有 无 43 CR -
[1] Southgate HED, Chen LD, Curtin NJ, et al. Targeting the DNA damage response for the treatment of high risk neuroblastoma[J]. Front Oncol, 2020, 10: 371.
[2] Irwin MS, Naranjo A, Zhang FF, et al. Revised neuroblastoma risk classification system: a report from the children's oncology group[J]. J Clin Oncol, 2021, 39(29): 3229-3241.
[3] Vo KT, Matthay KK, Neuhaus J, et al. Clinical, biologic, and prognostic differences on the basis of primary tumor site in neuroblastoma: a report from the international neuroblastoma risk group project[J]. J Clin Oncol, 2014, 32(28): 3169-3176.
[4] Fisher JPH, Tweddle DA. Neonatal neuroblastoma[J]. Semin Fetal Neonatal Med, 2012, 17(4): 207-215.
[5] 李艳珍, 刘雨薇, 王生才, 等. 儿童头颈部神经源性肿瘤临床分析[J]. 临床耳鼻咽喉头颈外科杂志, 2019, 33(10): 983-986. https://lceh.whuhzzs.com/article/doi/10.13201/j.issn.1001-1781.2019.10.020
[6] 中国抗癌协会小儿肿瘤专业委员会, 中华医学会小儿外科学分会肿瘤学组. 儿童神经母细胞瘤诊疗专家共识CCCG-NB-2021方案[J]. 中华小儿外科杂志, 2022, 43(7): 588-598.
[7] 赵强, 吴晔明. 儿童神经母细胞瘤诊疗专家共识[J]. 中华小儿外科杂志, 2015, 36(1): 3-7.
[8] Meany HJ. Non-high-risk neuroblastoma: classification and achievements in therapy[J]. Children(Basel), 2019, 6(1): 5.
[9] Sokol E, Desai AV, Applebaum MA, et al. Age, diagnostic category, tumor grade, and mitosis-karyorrhexis index are independently prognostic in neuroblastoma: an INRG project[J]. J Clin Oncol, 2020, 38(17): 1906-1918.
[10] Irwin MS, Naranjo A, Zhang FF, et al. Revised neuroblastoma risk classification system: a report from the children's oncology group[J]. J Clin Oncol, 2021, 39(29): 3229-3241.
[11] 刘玥, 张益, 张建国, 等. 多学科诊疗模式治疗颌面颈部巨大神经纤维瘤的临床分析[J]. 口腔疾病防治, 2021, 29(12): 848-853.
[12] 王欣迪, 段超, 张大伟, 等. 神经母细胞瘤患儿首发症状及其诊断意义分析[J]. 中华实用儿科临床杂志, 2019, 34(5): 359-363.
[13] Su Y, Qin H, Chen CH, et al. Treatment and outcomes of 1041 pediatric patients with neuroblastoma who received multidisciplinary care in China[J]. Pediatr Investig, 2020, 4(3): 157-167. doi: 10.1002/ped4.12214
[14] Mallepalli S, Gupta MK, Vadde R. Neuroblastoma: an updated review on biology and treatment[J]. Curr Drug Metab, 2019, 20(13): 1014-1022.
[15] Yao W, Li K, Dong KR, et al. Long-term prognosis of low-risk neuroblastoma treated by surgery alone: an experience from a single institution of China[J]. World J Pediatr, 2019, 15(2): 148-152. doi: 10.1007/s12519-018-0205-z
[16] 罗兴谷, 卢永田, 王晓彬. 内镜下经口径路咽旁间隙肿瘤摘除5例[J]. 山东大学耳鼻喉眼学报, 2014, 28(4): 56-58.
[17] 王德辉, 张焕康. 内镜颅底外科的现状与展望[J]. 临床耳鼻咽喉头颈外科杂志, 2024, 38(6): 463-466.
[18] 薛凯, 王磊, 郑实兴, 等. 咽旁间隙解剖及手术入路研究进展[J]. 临床耳鼻咽喉头颈外科杂志, 2024, 38(6): 534-540.
[19] Strother DR, London WB, Schmidt ML, et al. Outcome after surgery alone or with restricted use of chemotherapy for patients with low-risk neuroblastoma: results of Children's Oncology Group study P9641[J]. J Clin Oncol, 2012, 30(15): 1842-1848.
[20] Ahmed G, Fawzy M, Elmenawi S, et al. Role of surgery in localized initially unresectable neuroblastoma[J]. J Pediatr Urol, 2018, 14(3): 231-236.
[21] Twist CJ, Schmidt ML, Naranjo A, et al. Maintaining outstanding outcomes using response-and biology-based therapy for intermediate-risk neuroblastoma: a report from the children's oncology group study ANBL0531[J]. J Clin Oncol, 2019, 37(34): 3243-3255.
[22] 龙俊汕, 张京, 苏小霞, 等. 儿童神经母细胞瘤靶向治疗的研究进展[J]. 临床小儿外科杂志, 2023, 22(7): 619-624.
[23] Lonergan GJ, Schwab CM, Suarez ES, et al. Neuroblastoma, ganglioneuroblastoma, and ganglioneuroma: radiologic-pathologic correlation[J]. Radiographics, 2002, 22(4): 911-934.
[24] 金眉, 张大伟, 王焕民, 等. 儿童腹膜后神经母细胞瘤56例临床分析[J]. 中国循证儿科杂志, 2012, 7(3): 196-199.
[25] Lerone M, Ognibene M, Pezzolo A, et al. Molecular genetics in neuroblastoma prognosis[J]. Children(Basel), 2021, 8(6): 456.
[26] Liu QL, Feng L, Xue H, et al. Development and validation of a nomogram to predict the overall survival of patients with neuroblastoma[J]. Medicine(Baltimore), 2020, 99(10): e19199.
[27] Sokol E, Desai AV, Applebaum MA, et al. Age, diagnostic category, tumor grade, and mitosis-karyorrhexis index are independently prognostic in neuroblastoma: an INRG project[J]. J Clin Oncol, 2020, 38(17): 1906-1918.
[28] Kaufmann MR, Camilon PR, Janz TA, et al. Factors associated with the improved survival of head and neck neuroblastomas compared to other body sites[J]. Ann Otol Rhinol Laryngol, 2019, 128(3): 241-248.
[29] 杨佩仪, 苏雁, 王生才, 等. 多学科联合诊治颈部神经母细胞瘤临床分析[J]. 中华实用儿科临床杂志, 2020, 35(18): 1411-1415.
[30] Ingarfield K, McMahon AD, Douglas CM, et al. Determinants of long-term survival in a population-based cohort study of patients with head and neck cancer from Scotland[J]. Head Neck, 2019, 41(6): 1908-1917.
[31] 潘新良, 林云. 头颈部恶性肿瘤诊断与治疗的精准评估[J]. 中华耳鼻咽喉头颈外科杂志, 2022, 57(1): 89-94, 97.
[32] Skapek SX, Ferrari A, Gupta AA, et al. Rhabdomyosarcoma[J]. Nat Rev Dis Primers, 2019, 5(1): 1.
-

计量
- 文章访问数: 148
- 施引文献: 0




 下载:
下载: