Dynamic visual acuity screening test results analysis of 25 patients with peripheral vertigo
-
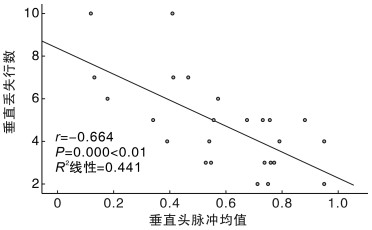
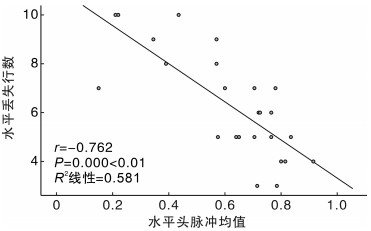
摘要: 目的 观察外周性眩晕患者动态视敏度(dynamic visual acuity, DVA)筛查试验结果并探讨其临床意义。 方法 48名健康志愿者作为对照组,25例外周性眩晕患者作为试验组,其中前庭神经炎患者12例,Hunt综合征患者1例,突发性聋伴眩晕5例,双侧前庭功能下降患者7例。进行水平与垂直动态视敏度筛查试验。将试验组与对照组的水平、垂直动态视敏度丢失行数进行比较; 对试验组内水平、垂直丢失行数进行比较; 将试验组内单、双侧前庭功能分别与对照组进行比较。 结果 对照组水平DVA丢失行数中位数为1.5,垂直DVA丢失行数中位数为1.0; 试验组水平DVA丢失行数中位数为6.0,垂直DVA丢失行数中位数为5.0。对照组和试验组的水平、垂直丢失行数比较差异均有统计学意义(P<0.01)。试验组组内水平和垂直丢失行数比较差异有统计学意义(P<0.01)。将试验组分为单侧前庭功能下降组(18例)和双侧前庭功能下降组(7例),与对照组进行对比,3组两两比较,水平和垂直丢失行数比较差异均有统计学意义(P<0.01),对照组水平和垂直DVA丢失行数明显分别低于单侧前庭功能下降组和双侧前庭功能下降组,单侧前庭功能下降组的水平和垂直丢失行数明显低于双侧前庭功能下降组(P<0.01)。25例外周性眩晕患者水平丢失行数与双侧水平半规管vHIT均值之间呈显著相关关系(P<0.01); 垂直丢失行数与双侧垂直半规管vHIT均值之间呈显著相关关系(P<0.01)。 结论 DVA筛查试验是现有外周前庭功能检查特别是vHIT测试的有效补充,能快速评估前庭功能下降患者的2 Hz前庭眼反射损伤程度。Abstract: Objective To observe the results of dynamic visual acuity screening tests in patients with peripheral vertigo and explore its clinical significance. Methods The number of 48 healthy volunteers were enrolled as control group and 25 peripheral vertigo patients as experimental group. In the experimental group, there are 12 patients with vestibular neuritis, 1 patient with Hunt syndrome, 5 patients with sudden deafness with vertigo and 7 patients with bilateral vestibular dysfunction. Horizontal and vertical dynamic visual acuity screening tests were performed on them. The number of lost rows of horizontal and vertical dynamic visual acuity was compared between the control group and the experimental group to figure out if there is a statistical difference. The number of lost rows of horizontal and vertical dynamic visual acuity was compared within the experimental group to figure out if there is a statistical difference. The two groups of 18 cases of unilateral vestibular function decline and 7 cases of bilateral vestibular function decline in the experimental group were compared with the control group, and figure out if there is a statistical difference. Results The median number of lost rows of horizontal dynamic visual acuity in 48 healthy volunteers was 1.5 and median number of lost rows of vertical dynamic visual acuity was 1.0 in the control group. The median number of lost rows of horizontal dynamic visual acuity of 26 healthy volunteers was 6 and median number of lost rows of vertical dynamic visual acuity was 5 in the experimental group. Compared to the experimental group, the number of lost rows both have statistical significance in horizontal and vertical dynamic visual acuity(P < 0.01). The comparison of horizontal and vertical lost rows within the test group also have statistical significance(P < 0.01). Twenty five patients with exceptional vestibular disease in the experimental group were divided into unilateral vestibular function reduction group(n=18) and bilateral vestibular function reduction group(n=7). Compared with the control group, there was significant differences in the number of horizontal and vertical lost rows(P < 0.01) within the three groups. After pairwise comparison, the number of lost rows of horizontal and vertical in the control group was significantly lower than that in the unilateral vestibular function reduction group and the bilateral vestibular function reduction group(P < 0.01). There was a highly significant correlation between the number of horizontally lost rows of DVA and the mean vHIT values of bilateral horizontal semicircular canals in 25 patients(P < 0.01); and a highly significant correlation between the number of vertically lost rows of DVA and the mean vHIT values of vertical semicircular canals in 4 groups bilaterally(P < 0.01). Conclusion The Dynamic Visual Acuity Screening Test is a useful addition to existing tests of peripheral vestibular function, particularly the vHIT test, and provides a rapid assessment of the extent of 2 Hz VOR impairment in patients with reduced vestibular function.
-
Key words:
- dynamic visual acuity /
- peripheral vertigo /
- vestibular function
-

-
表 1 对照组与试验组丢失行数比较
组别 例数 水平丢失行数 垂直丢失行数 Z P 试验组 25 6(5,8) 5(3,6) -3.683 <0.001 对照组 48 2(1,2) 1(0,1) -4.990 <0.001 Z -6.914 -6.880 P <0.001 <0.001 表 2 对照组与单侧前庭功能下降组、双侧前庭功能下降组比较
组别 例数 水平丢失行数 垂直丢失行数 健康组 48 2(1,2) 1(0,1) 单侧前庭功能下降组 18 5(4,6)1) 4(3,5)1) 双侧前庭功能下降组 7 9(8,10)1)2) 7(6,10)1)2) χ2 49.660 49.303 P <0.001 <0.001 与对照组比较,1)P<0.01;与单侧前庭疾病组比较,2)P<0.01。 -
[1] Herdman SJ, Clendaniel RA. Vestibular rehabilitation[M]. F.A. Daris Company, 2014: 12-13.
[2] 田军茹. 眩晕诊治的进展[J]. 中华老年心脑血管病杂志, 2012, 14(12): 1335-1337.
[3] 吴子明, 张素珍. 前庭功能检查与选择[J]. 中华耳科学杂志, 2013, 11(3): 397-400.
[4] 吴子明, 杜一, 刘兴健, 等. 规范前庭功能检查与临床应用[J]. 中华医学杂志, 2018, 98(16): 1209-1212.
[5] 李斐, 鞠奕, 张甦琳, 等. 前庭神经炎诊治多学科专家共识[J]. 中华老年医学杂志, 2020, 39(9): 985-994.
[6] 李姗姗, 陈太生, 董红, 等. Hunt综合征伴眩晕患者的半规管损伤频率特征[J]. 中华耳鼻咽喉头颈外科杂志, 2012, 47(1): 6-10.
[7] 余力生, 杨仕明. 突发性聋诊断和治疗指南(2015)[J]. 中华耳鼻咽喉头颈外科杂志, 2015, 50(6): 443-447.
[8] 凌霞, 朱扬, 王璟, 等. 双侧前庭病诊断标准: Bárány学会前庭疾病分类委员会共识[J]. 神经损伤与功能建, 2019, 14(12): 595-602.
[9] 黄瑞, 毕国荣. 双侧前庭病[J]. 临床耳鼻咽喉头颈外科杂志, 2017, 31(24): 3-3.
[10] Herdman SJ, Clendaniel RA. Vestibular rehabilitation[M]. F.A. Daris Company, 2014: 144-145.
[11] 张玉忠, 魏馨雨, 陈耔辰, 等. 功能性前庭眼动反射检测试验[J]. 临床耳鼻咽喉头颈外科杂志, 2019, 33(3): 213-215, 219. https://lceh.whuhzzs.com/article/doi/10.13201/j.issn.1001-1781.2019.03.007
[12] 李丽华, 张东颖. 规范进行视力检查[J]. 中国眼镜科技杂志, 2012, 1: 128-130.
[13] 贾宏博, 刘波, 杜一, 等. 前庭功能检查专家共识(二)(2019)[J]. 中华耳科学杂志, 2019, 17(2): 144-149.
[14] Maccaslin DL, Dundas JA, Jacobson GP. The Bedside Assessment of the vestibular system//jacobson G P, shepard N T. Balance Function Assessment and Management[M]. San Diego: Plural publishing Inc, 2008: 72-77.
[15] 何风, 韩军良, 白雅, 等. 前庭功能检查在前庭神经炎急性期患者受损部位分析中的应用[J]. 临床耳鼻咽喉头颈外科杂志, 2023, 37(4): 263-267. https://lceh.whuhzzs.com/article/doi/10.13201/j.issn.2096-7993.2023.04.005
-




 下载:
下载: