Comparison of different laryngeal preservation strategies based on chemoradiotherapy in locally advanced hypopharyngeal carcinoma
-
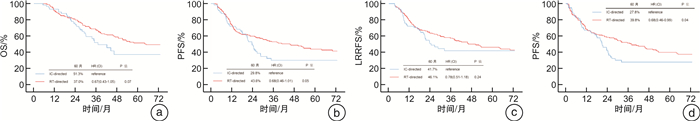
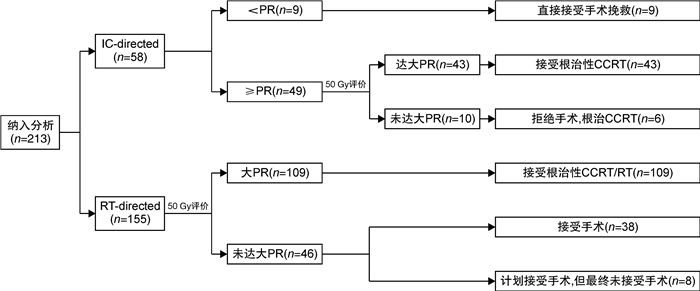
摘要: 目的 研究基于诱导化疗筛选放疗敏感患者(IC-directed)和基于早期放疗反应筛选放疗敏感患者(RT-directed)的保喉治疗策略在局部晚期可切除下咽癌中的临床特征和疗效比较。方法 回顾性分析中国医学科学院肿瘤医院2010年9月至2020年9月经病理证实的可切除局部晚期下咽癌患者,纳入接受IC-directed和RT-directed保喉治疗策略的231例患者。IC-directed模式是指患者先接受2个周期TPF方案诱导化疗,根据诱导化疗后的反应来决定后续治疗模式。如果原发灶缩小达到部分缓解(partial response,PR),则进行根治性同步放化疗;若原发灶缩小未达PR,则进行手术干预。RT-directed是利用早期放疗反应来筛选放疗敏感患者的综合治疗模式,具体是在放疗剂量达到50 Gy时,进行全面的分期检查和头颈部MDT评估,若原发灶缩小达到大PR(缩小达80%以上),则接受根治性放疗或同步放化疗;若原发灶缩小未达大PR,则休息4~6周后接受早期手术干预。研究终点为总生存时间(overall survival,OS)、无进展生存时间(progression free survival,PFS)、无局部区域复发生存(locoregional recurrence-free survival,LRRFS)、功能喉生存(survival with a functional larynx,SFL)。结果 本研究的中位随访时间为63.8个月。IC-directed组中有75.0%(57/76)患者在2个周期诱导化疗后达到PR,而RT-directed组中有70.3%(109/155)患者在放疗50 Gy时候疗效评价为大PR。全组患者的5年OS、PFS、LRRFS和SFL分别为47.9%、39.6%、44.3%和36.2%。比较2组治疗模式5年OS分别为51.3%和37.0%(HR 0.67;95%CI 0.43~1.05,P=0.07)。RT-directed治疗模式较IC-diercted治疗模式,在功能喉保留方面有显著优势,5年SFL分别为39.8%和27.8%(HR 0.68;95%CI 0.46~0.99;P=0.04),且两者手术并发症的发生率相似(P=0.60)。结论 在局部晚期可切除下咽癌中,相比于IC-directed的保喉治疗策略,RT-directed取得了较好的生存率和喉功能保全,且不增加手术并发症的发生。Abstract: Objective This study aimed to evaluate the clinical features and treatment outcomes of the value of response-adapted treatment following radiotherapy and induction chemotherapy follwing subsequent comprehensive therapy in patients with resectable locally advanced hypopharyngeal carcinoma.Methods This cohort study was conducted from September 2010 to September 2020 in our hospital, 231 patients pathologically confirmed stage Ⅲ and ⅣB resectable locally advanced hypopharyngeal carcinoma included. For the IC-directed ART strategy, IC is used to select good candidates to receive radical RT or CCRT, and others undergo surgery. He response-adapted strategy was determined based on the primary tumor response, which was evaluated at a dose of 50 Gy. If the response reached complete response or partial response(more than 80% tumor regression), patients received radical RT or CCRT; otherwise, they received surgery, if possible, at 4 to 6 weeks after RT. The end points of the study were OS(overall survival), progression free survival(PFS), locoregional recurrence-free survival(LRRFS) and LDFS.Results In IC-directed group, 75.0%(57/76) patients reached PR after 2 cycles of induction chemotherapy. While in RT-directed group, 70.3%(109/155) patients reached large PR at dose of 50 Gy. The median interquartile range follow-up period of the whole cohort was 63.8 months. The 5-year OS, PFS, LRRFS and SFL of the whole cohort were 47.9%、39.6%、44.3% and 36.2%, respectively. In evaluations based on the different treatment strategies, the 5-year OS and SFL were 51.3% versus 37.0%(HR 0.67; 95%CI 0.43-1.05; P=0.07) and 27.8% versus 39.8%(HR 0.68; 95%CI 0.46-0.99; P=0.04) between IC-directed and RT-directed groups. In additional, surgery complications did not significantly differ between these two groups.Conclusion In this cohort study, the response-adapted strategy based on an early RT response facilitated better treatment tailoring, and higher laryngeal preservation compared with IC-directed strategies. This approach could provide a feasible laryngeal preservation strategy in patients with resectable locally advanced hypopharyngeal carcinoma.
-

-
表 1 231例下咽癌患者一般临床资料比较
例(%) 特征 全组(231例) IC-directed组(76例) RT-directed组(155例) P 性别 0.06 男 222(96.1) 70(92.1) 152(98.1) 女 9(3.9) 6(7.9) 3(1.9) 年龄/岁 0.43 >56 101(43.7) 36(47.4) 65(41.9) ≤56 130(56.3) 40(52.6) 90(58.1) ECOG 0.05 0 28(12.1) 14(18.4) 14(9.0) 1 203(87.9) 62(81.6) 141(91.0) 病理类型 0.60 鳞状细胞癌 227(98.3) 74(97.4) 153(98.7) 其他 4(1.7) 2(2.6) 2(1.3) 亚区 0.12 梨状窝 198(85.7) 64(84.2) 134(86.5) 咽后壁 21(9.1) 5(6.6) 16(10.3) 环后区 12(5.2) 7(9.2) 5(3.2) 淋巴结ENE状态 0.29 ENE(+) 49(21.2) 13(17.1) 36(23.2) 临床T分期 0.34 T1~2 71(30.7) 19(25.0) 52(33.5) T3 70(30.3) 23(30.3) 47(30.3) T4a 90(39.0) 34(44.7) 56(36.1) 临床N分期 0.48 N0 25(10.8) 6(7.9) 19(12.3) N1 20(8.7) 8(10.5) 12(7.7) N2 135(58.4) 48(63.2) 87(56.1) N3 51(22.1) 14(18.4) 37(23.9) 临床分期 0.59 Ⅲ 29(12.6) 9(11.8) 20(12.9) ⅣA 151(65.4) 53(69.7) 98(63.2) ⅣB 51(22.0) 14(18.4) 37(23.9) 治疗前评估 0.85 需行全喉切除术 199(86.1) 65(85.5) 134(86.5) 可行保喉手术 32(13.9) 11(14.5) 21(13.5) 是否接受挽救手术 0.96 是 24(10.4) 8(10.5) 16(10.3) ENE为淋巴结包膜外侵犯。 表 2 213例下咽癌患者一般临床资料比较
例(%) 特征 全组(213例) IC-directed组(58例) RT-directed组(155例) P 性别 0.62 男 205(96.2) 56(96.6) 152(98.1) 女 8(3.8) 2(3.4) 3(1.9) 年龄/岁 0.20 >56 95(44.6) 30(51.7) 65(41.9) ≤56 118(55.4) 28(48.3) 90(58.1) ECOG 0.18 0 23(10.8) 9(15.5) 14(9.0) 1 190(89.2) 49(84.5) 141(91.0) 亚区 0.21 梨状窝 183(85.9) 49(84.5) 134(86.5) 咽后壁 10(4.7) 5(8.6) 16(10.3) 环后区 20(9.4) 4(6.9) 5(3.2) 淋巴结ENE状态 0.22 ENE(+) 45(21.1) 9(15.5) 36(23.2) 临床T分期 0.51 T1~2 67(31.5) 15(25.9) 52(33.5) T3 65(30.5) 18(31.0) 47(30.3) T4a 81(38.0) 25(43.1) 34(44.7) 临床N分期 0.38 N0 24(11.3) 5(8.6) 19(12.3) N1 20(9.4) 8(13.8) 12(7.7) N2 122(57.3) 35(60.3) 48(63.2) N3 47(22.1) 10(17.2) 37(23.9) 临床分期 0.56 Ⅲ 29(13.6) 9(15.5) 20(12.9) ⅣA 137(64.3) 39(67.2) 98(63.2) ⅣB 47(22.1) 10(17.2) 14(18.4) 治疗前评估 0.50 需行全喉切除术 182(85.4) 48(82.8) 134(86.5) 可行保喉手术 31(14.6) 10(17.2) 21(13.5) 是否接受挽救手术 1.00 是 22(10.3) 6(10.3) 16(10.3) -
[1] Machiels JP, René Leemans C, Golusinski W, et al. Squamous cell carcinoma of the oral cavity, larynx, oropharynx and hypopharynx: EHNS-ESMO-ESTRO Clinical Practice Guidelines for diagnosis, treatment and follow-up[J]. Ann Oncol, 2020, 31(11): 1462-1475. doi: 10.1016/j.annonc.2020.07.011
[2] Hall SF, Groome PA, Irish J, et al. The natural history of patients with squamous cell carcinoma of the hypopharynx[J]. Laryngoscope, 2008, 118(8): 1362-1371. doi: 10.1097/MLG.0b013e318173dc4a
[3] Luo X, Huang X, Liu S, et al. Synchronous Second Primary Cancers of Hypopharyngeal Carcinoma in the Image-Enhanced Endoscopy Era[J]. Laryngoscope, 2023, 133(8): 1906-1913. doi: 10.1002/lary.30420
[4] Luo X, Huang X, Liu S, et al. Evaluation of the prevalence of metachronous second primary malignancies in hypopharyngeal carcinoma and their effect on outcomes[J]. Cancer Med, 2022, 11(4): 1059-1067. doi: 10.1002/cam4.4501
[5] Blanchard P, Baujat B, Holostenco V, et al. Meta-analysis of chemotherapy in head and neck cancer(MACH-NC): a comprehensive analysis by tumour site[J]. Radiother Oncol, 2011, 100(1): 33-40. doi: 10.1016/j.radonc.2011.05.036
[6] Lefebvre JL, Chevalier D, Luboinski B, et al. Larynx preservation in pyriform sinus cancer: preliminary results of a European Organization for Research and Treatment of Cancer phase Ⅲ trial. EORTC Head and Neck Cancer Cooperative Group[J]. J Natl Cancer Inst, 1996, 88(13): 890-899. doi: 10.1093/jnci/88.13.890
[7] Pignon JP, le Maître A, Maillard E, et al. Meta-analysis of chemotherapy in head and neck cancer(MACH-NC): an update on 93 randomised trials and 17, 346 patients[J]. Radiother Oncol, 2009, 92(1): 4-14. doi: 10.1016/j.radonc.2009.04.014
[8] Yang YF, Wang R, Fang JG, et al. [A single-arm prospective study on induction chemotherapy and subsequent comprehensive therapy for advanced hypopharyngeal squamous cell carcinoma: report of 260 cases in a single center][J]. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi, 2020, 55(12): 1143-1153.
[9] Forastiere AA, Goepfert H, Maor M, et al. Concurrent chemotherapy and radiotherapy for organ preservation in advanced laryngeal cancer[J]. N Engl J Med, 2003, 349(22): 2091-2098. doi: 10.1056/NEJMoa031317
[10] Forastiere AA, Zhang Q, Weber RS, et al. Long-term results of RTOG 91-11: a comparison of three nonsurgical treatment strategies to preserve the larynx in patients with locally advanced larynx cancer[J]. J Clin Oncol, 2013, 31(7): 845-852. doi: 10.1200/JCO.2012.43.6097
[11] Henriques De Figueiredo B, Fortpied C, Menis J, et al. Long-term update of the 24954 EORTC phase Ⅲ trial on larynx preservation[J]. Eur J Cancer, 2016, 65: 109-112. doi: 10.1016/j.ejca.2016.06.024
[12] Lefebvre JL, Rolland F, Tesselaar M, et al. Phase 3 randomized trial on larynx preservation comparing sequential vs alternating chemotherapy and radiotherapy[J]. J Natl Cancer Inst, 2009, 101(3): 142-152. doi: 10.1093/jnci/djn460
[13] Luo X, Huang X, Liu S, et al. Response-Adapted Treatment Following Radiotherapy in Patients With Resectable Locally Advanced Hypopharyngeal Carcinoma[J]. JAMA Netw Open, 2022, 5(2): e220165. doi: 10.1001/jamanetworkopen.2022.0165
[14] Avinçsal MO, Shinomiya H, Teshima M, et al. Impact of alcohol dehydrogenase-aldehyde dehydrogenase polymorphism on clinical outcome in patients with hypopharyngeal cancer[J]. Head Neck, 2018, 40(4): 770-777. doi: 10.1002/hed.25050
[15] Dietz A, Wichmann G, Kuhnt T, et al. Induction chemotherapy(IC)followed by radiotherapy(RT)versus cetuximab plus IC and RT in advanced laryngeal/hypopharyngeal cancer resectable only by total laryngectomy-final results of the larynx organ preservation trial DeLOS-Ⅱ[J]. Ann Oncol, 2018, 29(10): 2105-2114. doi: 10.1093/annonc/mdy332
[16] Lefebvre JL, Andry G, Chevalier D, et al. Laryngeal preservation with induction chemotherapy for hypopharyngeal squamous cell carcinoma: 10-year results of EORTC trial 24891[J]. Ann Oncol, 2012, 23(10): 2708-2714. doi: 10.1093/annonc/mds065
[17] Lefebvre JL, Pointreau Y, Rolland F, et al. Induction chemotherapy followed by either chemoradiotherapy or bioradiotherapy for larynx preservation: the TREMPLIN randomized phase Ⅱ study[J]. J Clin Oncol, 2013, 31(7): 853-859. doi: 10.1200/JCO.2012.42.3988
[18] Pointreau Y, Garaud P, Chapet S, et al. Randomized trial of induction chemotherapy with cisplatin and 5-fluorouracil with or without docetaxel for larynx preservation[J]. J Natl Cancer Inst, 2009, 101(7): 498-506. doi: 10.1093/jnci/djp007
[19] Posner MR, Hershock DM, Blajman CR, et al. Cisplatin and fluorouracil alone or with docetaxel in head and neck cancer[J]. N Engl J Med, 2007, 357(17): 1705-1715. doi: 10.1056/NEJMoa070956
[20] Department of Veterans Affairs Laryngeal Cancer Study Group, Wolf GT, Fisher SG, et al. Induction chemotherapy plus radiation compared with surgery plus radiation in patients with advanced laryngeal cancer[J]. N Engl J Med, 1991, 324(24): 1685-1690. doi: 10.1056/NEJM199106133242402
[21] Singer S, Danker H, Guntinas-Lichius O, et al. Quality of life before and after total laryngectomy: results of a multicenter prospective cohort study[J]. Head Neck, 2014, 36(3): 359-368. doi: 10.1002/hed.23305
[22] Qian W, Zhu G, Wang Y, et al. Multi-modality management for loco-regionally advanced laryngeal and hypopharyngeal cancer: balancing the benefit of efficacy and functional preservation[J]. Med Oncol, 2014, 31(9): 178. doi: 10.1007/s12032-014-0178-2
[23] Takes RP, Strojan P, Silver CE, et al. Current trends in initial management of hypopharyngeal cancer: the declining use of open surgery[J]. Head Neck, 2012, 34(2): 270-281. doi: 10.1002/hed.21613
-




 下载:
下载: