Analysis of related factors for postoperative recurrence of antrochoanal polyps in children
-
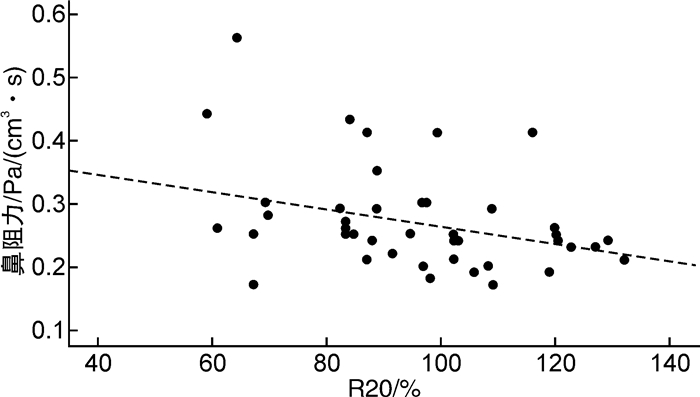
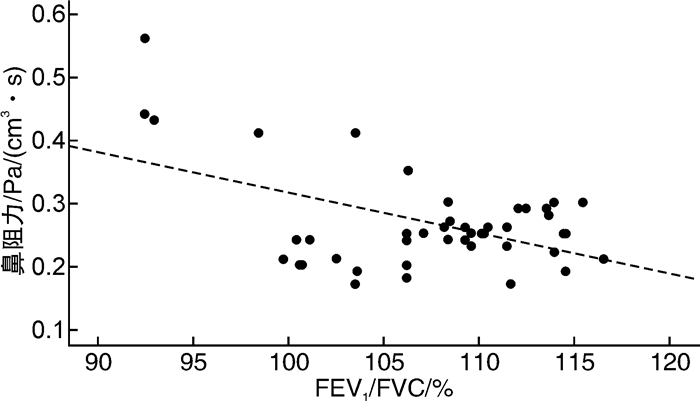
摘要: 目的 分析变应性鼻炎(allergic rhinitis,AR)患儿鼻阻力和肺功能之间的相关性,探究鼻阻力升高的AR患儿是否伴有潜在的下呼吸道受累。方法 选取2021年12月—2022年12月确诊为AR的88例患儿作为研究组,同期20例正常儿童作为对照组。研究组及对照组儿童均进行肺功能检查、支气管舒张试验、鼻阻力测定,将鼻阻力和肺功能检查结果进行Spearman相关性分析和多重性线性回归分析,探究两者间的关系及影响因素。根据鼻阻力测定结果将鼻阻力升高伴肺功能异常的患儿分为鼻阻力轻度升高伴肺功能异常组及鼻阻力中-重度升高伴肺功能异常组,分析鼻阻力升高的程度是否会影响肺功能。结果 研究组用力呼出25%、50%、75%肺活量时的平均呼气流量(FEF25、FEF50、FEF75)明显低于对照组(P < 0.05)。AR鼻阻力中-重度升高的患儿第一秒用力呼气量(FEV1)明显低于AR鼻阻力轻度升高的患儿(P < 0.05)。AR患儿鼻阻力与一秒率(FEV1/FVC)、中心呼吸道阻力(R20)具有相关性,FEV1/FVC、R20是AR患儿鼻阻力的影响因素(P < 0.05)。AR患儿血清总IgE与肺功能及支气管舒张试验均无相关性(P>0.05)。结论 AR患儿鼻腔通气功能发生了改变,小气道功能有下降趋势。AR鼻阻力中-重度升高的患儿比轻度升高的患儿肺通气功能下降更明显。AR患儿鼻阻力受FEV1/FVC、R20的影响,FEV1/FVC、R20随着鼻阻力值升高而降低。肺功能和FEV1改善率不是血清总IgE升高的影响因素。Abstract: Objective To analyze the correlation between nasal resistance and lung function in children with allergic rhinitis(AR), and explore whether AR children with increased nasal resistance are accompanied by potential lower respiratory tract involvement.Methods A total of 88 children diagnosed with AR from December 2021 to December 2022 were selected as the study group, while 20 normal children were selected as the control group during the same period. Both the study group and the control group children underwent lung function tests, bronchodilator tests, and nasal resistance measurements. Spearman correlation analysis and multiple linear regression analysis were performed on the results of nasal resistance and lung function tests to explore the relationship and influencing factors between the two groups.According to the results of nasal resistance measurement, children with increased nasal resistance and abnormal lung function were divided into a mild increase in nasal resistance with abnormal lung function group and a moderate to severe increase in nasal resistance with abnormal lung function group. The degree of increased nasal resistance was analyzed to determine whether it would affect lung function.Results The FEF25, FEF50, and FEF75 levels in the study group were significantly lower than those in the control group(P < 0.05). The FEV1of children with moderate to severe increase in AR nasal resistance was significantly lower than that of children with mild increase in AR nasal resistance(P < 0.05). There was a correlation between nasal resistance and FEV1/FVC, R20 in AR children, and FEV1/FVC, R20 were the influencing factors of nasal resistance in AR children(P < 0.05). There was no correlation between total serum IgE, lung function, and bronchodilation test in AR patients(P>0.05).Conclusion The nasal ventilation function of AR patients has changed, and there is a downward trend in small airway function. Children with moderate to severe increase in AR nasal resistance have a more significant decrease in lung ventilation function than those with mild increase. The nasal resistance of AR children is influenced by FEV1/FVC and R20, and FEV1/FVC and R20 decrease as the nasal resistance value increases. The improvement rate of lung function and FEV1 are not influencing factors for the elevation of total serum IgE.
-
Key words:
- allergic rhinitis /
- children /
- nasal resistance /
- lung function
-

-
表 1 研究组与对照组基线资料比较
X±S 组别 例数 男∶女/例 年龄/岁 身高/cm 体重/kg 研究组 88 56∶32 6.11±0.83 121.86±0.83 23.93±0.83 对照组 20 12∶8 6.25±0.79 122.43±0.77 24.21±0.56 F 1.45 1.27 1.63 P 0.318 0.536 0.196 表 2 研究组与对照组鼻阻力值和肺功能检查结果比较
X±S 指标 研究组(n=88) 对照组(n=20) t P FVC/% 100.49±13.86 99.98±6.49 -0.165 0.870 FEV1/% 108.60±12.74 110.37±5.96 0.604 0.550 FEV1/FVC/% 102.49±9.11 108.16±5.23 1.241 0.225 FEF25/% 102.66±15.83 114.93±10.98 3.024 0.004 FEF50/% 93.23±16.69 109.49±16.30 3.225 0.002 FEF75/% 95.83±19.59 106.99±14.70 2.114 0.040 FEV1/% 3.87±1.30 3.44±1.14 -0.321 0.750 R5/% 100.40±17.09 94.32±15.59 -1.244 0.220 R20/% 94.66±21.15 92.86±18.72 -0.302 0.764 X5/% 0.02±0.01 0.06±0.01 1.918 0.062 鼻阻力/Pa/(cm3·s) 0.30±0.07 0.24±0.03 3.500 0.002 表 3 对照组与AR鼻阻力升高的患儿比较
%,X±S 指标 对照组(n=20) AR鼻阻力升高的患儿(n=69) t P FVC 99.98±6.49 97.58±12.71 0.750 0.459 FEV1 110.37±5.96 106.66±12.63 1.188 0.242 FEV1/FVC 108.16±5.23 106.30±7.04 0.948 0.349 FEF25 114.93±10.98 102.48±14.58 3.050 0.004 FEF50 109.49±16.30 93.65±18.10 2.908 0.006 FEF75 106.99±14.70 95.38±21.09 1.429 0.161 R5 94.32±15.59 100.70±18.49 -1.179 0.246 R20 92.86±18.72 99.76±20.19 -1.121 0.269 表 4 对照组与AR鼻阻力升高伴肺功能异常的患儿比较
%,X±S 指标 对照组(n=20) AR鼻阻力升高伴肺功能异常的患儿(n=28) t P FVC 99.98±6.49 101.79±13.58 -0.616 0.541 FEV1 110.37±5.96 112.44±11.81 -0.795 0.431 FEV1/FVC 108.16±5.23 104.19±6.86 2.169 0.035 FEF25 114.93±10.98 109.26±13.85 1.521 0.135 FEF50 109.49±16.30 99.34±17.51 2.038 0.047 FEF75 106.99±14.70 89.80±38.21 1.744 0.089 R5 94.32±15.59 123.02±21.86 -5.023 < 0.001 R20 92.86±18.72 96.43±18.62 -0.655 0.516 表 5 AR鼻阻力轻度升高伴肺功能异常组与AR鼻阻力中-重度升高伴肺功能异常组比较
%,X±S 指标 AR鼻阻力轻度升高伴肺功能异常组(n=18) AR鼻阻力中-重度升高伴肺功能异常组(n=10) t P FVC 107.22±11.41 99.52±14.58 -1.492 0.147 FEV1 114.56±12.96 102.87±14.63 -2.176 0.038 FEV1/FVC 105.20±4.26 103.87±8.06 -0.503 0.619 FEF25 107.52±11.57 98.40±21.89 -1.266 0.217 FEF50 98.65±19.49 87.82±25.94 -1.183 0.247 FEF75 87.46±31.32 86.44±30.34 -0.087 0.932 R5 119.00±25.96 123.26±21.54 0.478 0.637 R20 94.91±19.11 101.22±21.62 0.796 0.433 表 6 AR患儿鼻阻力与肺功能相关性分析
指标 r P FVC 0.20 0.190 FEV1 0.20 0.112 FEV1/FVC -0.44 0.003 FEF25 0.06 0.714 FEF50 0.08 0.615 FEF75 -0.04 0.808 R5 -0.09 0.544 R20 -0.33 0.025 X5 -0.12 0.436 支气管舒张试验FEV1改善率 0.08 0.590 表 7 AR患儿鼻阻力与FEV1/FVC、R20多重性线性回归分析
指标 β 标准误 t P FEV1/FVC -0.01 0.01 -2.961 0.005 R20 -0.01 0.01 -2.082 0.043 常量 0.57 0.08 7.274 < 0.001 表 8 AR患儿血清总IgE与肺功能相关性分析
指标 r P FVC -0.07 0.498 FEV1 -0.04 0.720 FEV1/FVC 0.09 0.413 FEF25 0.07 0.495 FEF50 0.10 0.340 FEF75 0.11 0.322 R5 -0.14 0.203 R20 0.02 0.852 支气管舒张试验FEV1改善率 0.13 0.224 -
[1] Kou W, Li X, Yao H, et al. Meta-analysis of the comorbidity rate of allergic rhinitis and asthma in Chinese children[J]. Int J Pediatr Otorhinolaryngol, 2018, 107: 131-134. doi: 10.1016/j.ijporl.2018.02.001
[2] 中华耳鼻咽喉头颈外科杂志编辑委员会鼻科组, 中华医学会耳鼻咽喉头颈外科学分会鼻科学组、小儿学组. 儿童变应性鼻炎诊断和治疗指南(2022年, 修订版)[J]. 中华耳鼻咽喉头颈外科杂志, 2022, 57(4): 392-404. https://www.cnki.com.cn/Article/CJFDTOTAL-YRBH202202017.htm
[3] Zhang YM, Zhang J, Liu SL, et al. Prevalence and associated risk factors of allergic rhinitis in preschool children in Beijing[J]. Laryngoscope, 2013, 123(1): 28-35. doi: 10.1002/lary.23573
[4] Shen Y, Zeng JH, Hong SL, et al. Prevalence of allergic rhinitis comorbidity with asthma and asthma with allergic rhinitis in China: A meta-analysis[J]. Asian Pac J Allergy Immunol, 37(4): 220-225.
[5] Ferguson B, Powell-Davis A. The link between upper and lower respiratory disease[J]. Curr Opin Otolaryngol Head Neck Surg, 2003, 11: 192-195. doi: 10.1097/00020840-200306000-00011
[6] Grossman J. One airway, one disease[J]. Chest, 1997, 111(2 Suppl): 11S-16S. http://dx.doi.org/10.7748/phc2005.03.15.2.31.c537
[7] 陈亚秋. 儿童变应性鼻炎肺功能及相关因素的研究[J]. 中国耳鼻咽喉颅底外科杂志, 2008, 14(2): 111-114. https://www.cnki.com.cn/Article/CJFDTOTAL-ZEBY200802011.htm
[8] Kessel A. The impact of intranasal corticosteroids on lung function in children with allergic rhinitis[J]. Pediatr Pulmonol, 2014, 49(9): 932-937. doi: 10.1002/ppul.22912
[9] Kuo RW, Chan R, Lipworth B. Does unified allergic airway disease impact on lung function and type 2 biomarkers?[J]. Allergy Asthma Clin Immunol, 2019, 15: 75. doi: 10.1186/s13223-019-0388-4
[10] 古丽波斯坦, 阿不都如苏力, 尤乐都斯, 等. 变应性鼻炎患者肺功能改变及临床意义探讨[J]. 临床耳鼻咽喉头颈外科杂志, 2010, 24(23): 1068-1070. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201023006.htm
[11] Iyer A, Athavale A. Nasal Airway Resistance and Latent Lower Airway Involvement in Allergic Rhinitis[J]. J Assoc Physicians India, 2020, 68(3): 43-47. http://www.researchgate.net/publication/339774972_Nasal_Airway_Resistance_and_Latent_Lower_Airway_Involvement_in_Allergic_Rhinitis
[12] 曹春婷, 张罗, 韩德民. 鼻阻力测量的临床应用[J]. 国际耳鼻咽喉头颈外科杂志, 2007, 31(2): 77-80. https://www.cnki.com.cn/Article/CJFDTOTAL-ZEBY201602029.htm
[13] 胡晓东, 尤乐都斯. 鼻阻力测压的临床应用[J]. 国际耳鼻咽喉头颈外科杂志, 2014, 38(5): 300-303.
[14] 中华医学会. 常规肺功能检查基层指南(2018年)[J]. 中华全科医师杂志, 2019, 18(6): 511-518.
[15] 上海市医学会儿科学分会呼吸学组, 上海儿童医学中心儿科医疗联合体(浦东), 上海智慧儿科临床诊治技术工程技术研究中心. 儿童哮喘小气道功能障碍评估及治疗专家共识[J]. 中华实用儿科临床杂志, 2021, 36(23): 1761-1768.
[16] 儿童肺功能系列指南(二): 肺容积和通气功能[J]. 中华实用儿科临床杂志, 2016, 31(10): 744-750.
[17] 儿童肺功能系列指南(三): 脉冲振荡[J]. 中华实用儿科临床杂志, 2016, 31(11): 821-825.
[18] Valero A, Quirce S, Dávila I, et al. Allergic respiratory disease: Different allergens, different symptoms[J]. Allergy, 2017, 72(9): 1306-1316.
[19] Thayyezhuth D, Venkataram R, Bhat V, et al. A study of Spirometric parameters in non asthmatic allergic rhinitis[J]. Heliyon, 2021, 7(11): e08270.
[20] Leonardy JG, Peacock LB. An evaluation of quantitative serum immunoglobulin determinations in clinical practice[J]. Ann Allergy, 1972, 30(7): 378-390. http://europepmc.org/abstract/MED/4625094
[21] 周彤, 方明玉, 吴安然, 等. 正常儿童及成年人血清IgE水平[J]. 中华医学杂志, 1979, 59(11): 681-685. https://www.cnki.com.cn/Article/CJFDTOTAL-XYXX198002011.htm
-




 下载:
下载: