-
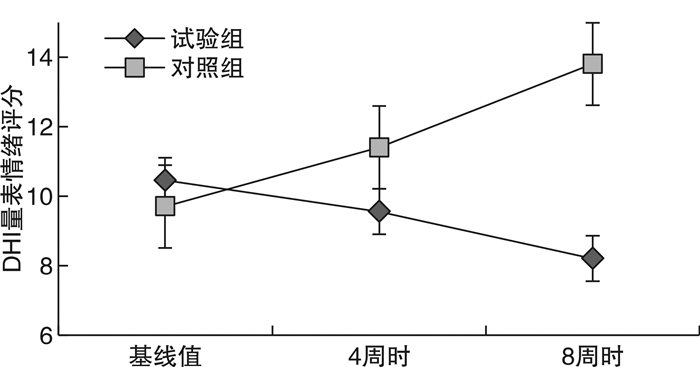
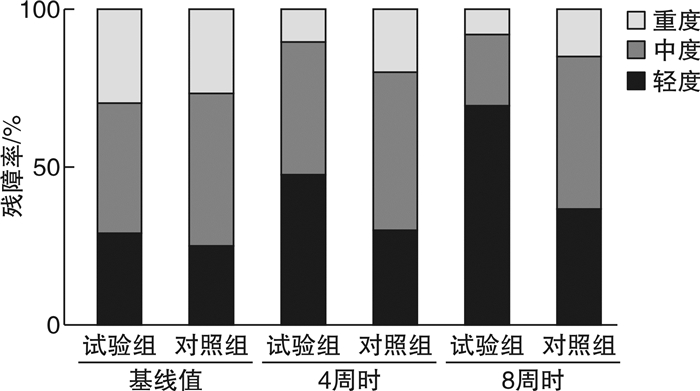
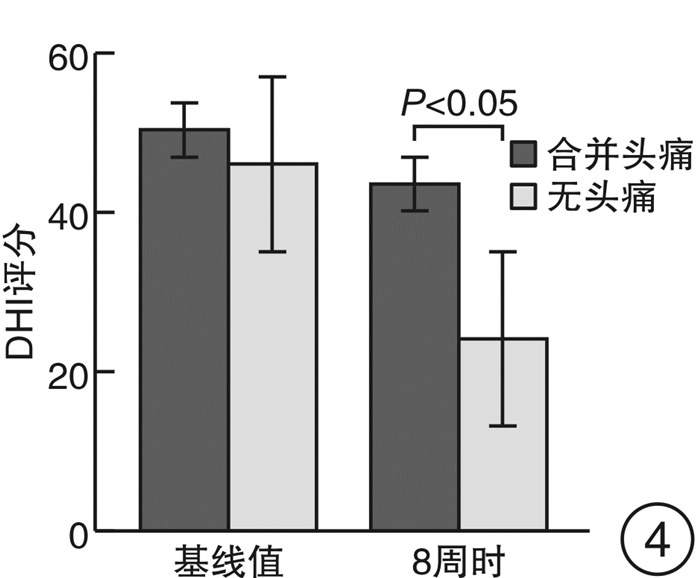
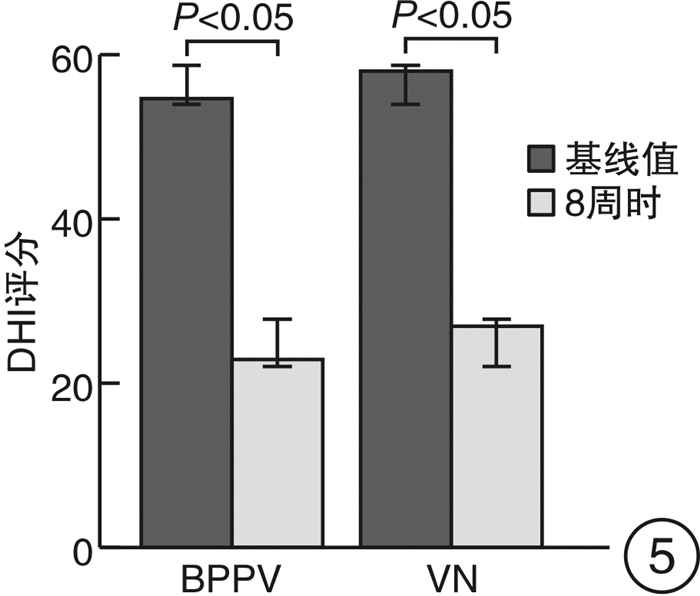
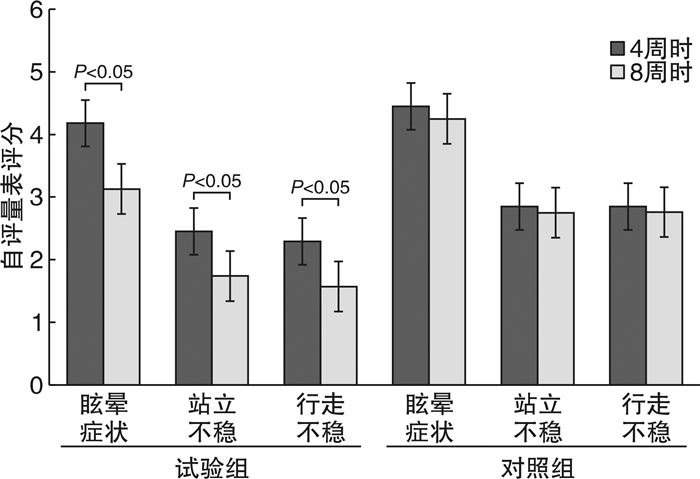
摘要: 目的 评价前庭外周性眩晕患者前庭康复的疗效,并分析其影响因素。方法 收集2018年1月—2021年6月北京康复医院耳鼻咽喉科门诊确诊的前庭外周性眩晕患者153例(其中良性阵发性位置性眩晕47例,梅尼埃病38例,突发性聋伴眩晕26例,前庭性偏头痛23例,前庭神经炎19例),随机按照2∶1样本量匹配,试验组103例患者采用前庭康复联合药物治疗,对照组50例仅口服药物治疗。分别在开始治疗时、治疗4周时和治疗8周时进行自评量表和眩晕残障程度评定量表(DHI)评价,比较两组患者的疗效,同时采用多元线性回归分析影响疗效的独立危险因素。结果 两组临床资料、自评量表和DHI评分各基线值的差异均无统计学意义(P>0.05)。4周和8周时试验组自评量表和DHI评分均优于对照组(均P<0.01),8周时疗效优于4周,尤其表现为行走时情绪得分降低和重度眩晕残障程度比例降低(均P<0.01)。同时,良性阵发性位置性眩晕和前庭神经炎患者自评量表和DHI评分优于梅尼埃病、前庭性偏头痛和突发性聋伴眩晕患者(P<0.05)。合并头痛(P<0.05)、治疗前眩晕残障程度较重(P<0.01)为影响前庭康复疗效的独立危险因素。结论 前庭康复联合药物治疗前庭外周性眩晕的效果优于仅使用药物治疗的效果,尤其在改善情绪障碍和眩晕残障程度方面较为明显。此前庭康复方案更适于良性阵发性位置性眩晕和前庭神经炎患者,合并头痛或重度眩晕的疗效较差。Abstract: Objective To evaluate the efficacy of vestibular rehabilitation in patients with anterior peripheral vertigo and analyze its influencing factors.Methods From January 2018 to June 2021, 153 cases with peripheral vertigo diseases(including 47 cases of benign positional paroxysmal vertigo, 38 cases of Meniere's disease, 26 cases of sudden deafness with vertigo, 23 cases of vestibular migraine and 19 cases of vestibular neuritis) were enrolled. One hundred and three cases were treated with vestibular rehabilitation combined with drugs, and 50 cases only treated with drugs were used as controls. Self-rating scale and vertigo disorder scale were evaluated at the beginning of treatment, 4 weeks and 8 weeks, respectively. The curative effects of the two groups were tested by t-test, and the independent risk factors affecting the curative effects were analyzed by multiple linear regression.Results There was no difference in clinical data, self-assessment scale and vertigo disorder scale between the two groups(P>0.05). At 4 and 8 weeks, the scores of self-assessment scale and vertigo disorder scale in the experimental group were better than those in the control group(all P < 0.01), and the curative effect at 8 weeks was better than that at 4 weeks, especially the decrease of emotional score during walking and the proportion of severe vertigo disability(all P < 0.01). The scores of self-rating scale and vertigo disorder scale of the cases with benign positional paroxysmal vertigo and vestibular neuritis were better than Meniere's disease, vestibular migraine and sudden deafness with vertigo(P < 0.05). Headache(P < 0.05) and severe vertigo disorder before intervention(P < 0.01) were independent risk factors affecting the efficacy of vestibular rehabilitation.Conclusion Vestibular rehabilitation combined with anti-vertigo drugs in the treatment of vestibular peripheral vertigo is better than that of only using drugs, especially in improving the degree of emotional disorder and vertigo disability. It is more suitable for benign positional paroxysmal vertigo and vestibular neuritis, while the effect of combined headache or severe vertigo is relatively poor.
-
Key words:
- vertigo /
- vestibular rehabilitation /
- treatment effectiveness
-

-
表 1 两组临床资料比较
项目 试验组 对照组 P值 性别 0.473 男 33(32.0) 19(38.0) 女 70(68.0) 31(62.0) 年龄/岁 51.4±14.2 50.4±11.6 0.761 主诉a) 0.385 转圈样旋转 56(54.4) 36(72.0) 头晕沉感 38(36.9) 24(48.0) 走路不稳 30(29.1) 10(20.0) 漂浮感 19(18.4) 6(12.0) 表述不清 15(14.6) 8(16.0) 病种 0.935 BPPV 32(31.1) 15(30.0) 梅尼埃病 26(25.2) 12(24.0) 突发性聋伴眩晕 16(15.5) 10(20.0) VM 15(14.6) 8(16.0) VN 14(13.6) 5(10.0) 耳部症状 0.541 耳鸣 7(6.8) 6(12.0) 听力下降 11(10.7) 5(10.0) 耳鸣+听力下降 21(20.4) 13(26.0) 无 64(62.1) 26(52.0) 是否合并头痛 0.495 是 15(14.6) 8(16.0) 否 88(85.4) 42(84.0) 是否存在诱发因素 0.522 是 73(70.9) 36(72.0) 否 30(29.1) 14(28.0) 注:a)同一患者可能伴有2个或2个以上主诉。 表 2 试验组影响DHI评分的多元回归分析
系数 非标准化系数 标准化系数 t值 P值 共线性统计 回归系数 标准差 回归系数 允差 方差膨胀因子 (常数) 11.496 5.242 2.193 0.032 合并耳部症状 3.958 3.804 0.101 1.040 0.303 0.928 1.078 合并头痛 11.015 4.669 0.236 2.359 0.022 0.867 1.153 DHI评分基线值 0.618 0.104 0.705 5.938 <0.010 0.614 1.629 自评量表基线值 -1.346 0.842 -0.192 -1.599 0.115 0.603 1.659 -
[1] Kristiansen L, Magnussen LH, Juul-Kristensen B, et al. Feasibility of integrating vestibular rehabilitation and cognitive behaviour therapy for people with persistent dizziness[J]. Pilot Feasibility Stud, 2019, 5: 69. doi: 10.1186/s40814-019-0452-3
[2] Roh KJ, Kim MK, Kim JH, et al. Role of Emotional Distress in Prolongation of Dizziness: A Cross-Sectional Study[J]. J Audiol Otol, 2017, 22(1): 6-12.
[3] 刘永胜, 朱欣茹, 汤勇, 等. 前庭综合征患者伴发焦虑抑郁情绪的调查[J]. 中华耳科学杂志, 2019, 17(6): 818-822. doi: 10.3969/j.issn.1672-2922.2019.06.003
[4] 徐先荣, 杨军. 眩晕内科诊治和前庭康复[M]. 北京: 科学出版社, 2020: 15-137.
[5] 中华耳鼻咽喉头颈外科杂志编辑委员会, 中华医学会耳鼻咽喉头颈外科学分会. 良性阵发性位置性眩晕诊断和治疗指南(2017)[J]. 中华耳鼻咽喉头颈外科杂志, 2017, 52(3): 173-177. https://cpfd.cnki.com.cn/Article/CPFDTOTAL-ZGZP201709006014.htm
[6] 中华耳鼻咽喉头颈外科杂志编辑委员会, 中华医学会耳鼻咽喉头颈外科学分会. 梅尼埃病诊断和治疗指南(2017)[J]. 中华耳鼻咽喉头颈外科杂志, 2017, 52(3): 167-172. doi: 10.3760/cma.j.issn.1673-0860.2017.03.002
[7] 中国卒中学会卒中与眩晕分会, 中国医师协会神经内科医师分会眩晕专业委员会. 前庭性偏头痛诊疗多学科专家共识[J]. 中华内科杂志, 2019, 58(2): 102-107.
[8] 中国医师协会神经内科分会眩晕专业委员会, 中国卒中学会卒中与眩晕分会, 李斐, 等. 前庭神经炎诊治多学科专家共识[J]. 中华老年医学杂志, 2020, 39(9): 985-994. doi: 10.3760/cma.j.issn.0254-9026.2020.09.001
[9] 姜树军, 孙勍, 荣良群, 等. 常用的前庭康复疗法[J]. 中国听力语言康复科学杂志, 2020, 18(1): 1-4, 10. doi: 10.3969/j.issn.1672-4933.2020.01.001
[10] Meldrum D, Jahn K. Gaze stabilisation exercises in vestibular rehabilitation: review of the evidence and recent clinical advances[J]. J Neurol, 2019, 266(Suppl 1): 11-18.
[11] 林晨珏, 席淑新, 王璟. 前庭康复训练对前庭外周性眩晕患者眩晕残障症状的改善作用[J]. 中华医学杂志, 2020, 100(32): 2503-2506. doi: 10.3760/cma.j.cn112137-20191202-02621
[12] Brandt T, Dieterich M. 'Excess anxiety' and 'less anxiety': both depend on vestibular function[J]. Curr Opin Neurol, 2020, 33(1): 136-141. doi: 10.1097/WCO.0000000000000771
[13] 王欣, 吕建萌, 杨谦. 良性阵发性位置性眩晕复位后残余症状的相关影响因素及治疗研究进展[J]. 疑难病杂志, 2020, 19(11): 1179-1182, 1188. https://www.cnki.com.cn/Article/CJFDTOTAL-YNBZ202011026.htm
[14] 谷李欣, 陈建勇, 张勤, 等. 后半规管良性阵发性位置性眩晕病程对复位成功后残余症状的影响[J]. 临床耳鼻咽喉头颈外科杂志, 2021, 35(11): 976-980. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202111004.htm
[15] Basura GJ, Adams ME, Monfared A, et al. Clinical Practice Guideline: Ménière's Disease[J]. Otolaryngol Head Neck Surg, 2020, 162(2_suppl): S1-S55. doi: 10.1177/0194599820909438
[16] 史珊珊, 江雪梅, 潘永惠. 前庭性偏头痛发病机制及诊疗的研究进展[J]. 中国临床神经科学, 2020, 28(1): 104-109. https://www.cnki.com.cn/Article/CJFDTOTAL-LCSK202001017.htm
[17] 马丹丹, 王乐, 赵堃, 等. 伴眩晕的单侧全聋型突发性聋预后相关因素分析[J]. 中华耳科学杂志, 2021, 19(3): 437-441. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHER202103008.htm
[18] O'Connell Ferster AP, Priesol AJ, Isildak H. The clinical manifestations of vestibular migraine: A review[J]. Auris Nasus Larynx, 2017, 44(3): 249-252.
[19] 王恩彤, 王鹏, 单希征. 美国耳鼻咽喉头颈外科学会梅尼埃病诊疗指南解读[J]. 北京医学, 2020, 42(9): 874-878. https://www.cnki.com.cn/Article/CJFDTOTAL-BJYX202009021.htm
[20] 陈元星, 孙悍军, 张清华, 等. 梅尼埃病与前庭性偏头痛共病患者的临床特点[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(9): 820-823. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202009012.htm
[21] Pyykkö I, Pyykkö N, Manchaiah V. Vestibular drop attacks in Ménière's disease and its association with migraine[J]. Eur Arch Otorhinolaryngol, 2020, 277(7): 1907-1916.
[22] Shin CH, Kim Y, Yoo MH, et al. Management of Ménière's Disease: How Does the Coexistence of Vestibular Migraine Affect Outcomes?[J]. Otol Neurotol, 2019, 40(5): 666-673.
[23] Alghadir AH, Anwer S. Effects of Vestibular Rehabilitation in the Management of a Vestibular Migraine: a Review[J]. FRONT NEUROL, 2018, 9: 440.
[24] Beh SC, Masrour S, Smith SV, et al. The Spectrum of Vestibular Migraine: Clinical Features, Triggers, and Examination Findings[J]. Headache, 2019, 59(5): 727-740.
-

| 引用本文: | 崔庆佳, 王蕊, 闫瑾, 等. 前庭外周性眩晕患者前庭康复短期疗效及其影响因素[J]. 临床耳鼻咽喉头颈外科杂志, 2022, 36(3): 217-221. doi: 10.13201/j.issn.2096-7993.2022.03.012 |
| Citation: | CUI Qingjia, WANG Rui, YAN Jin, et al. Vestibular rehabilitation in patients with vestibular peripheral vertigo[J]. J Clin Otorhinolaryngol Head Neck Surg, 2022, 36(3): 217-221. doi: 10.13201/j.issn.2096-7993.2022.03.012 |
- Figure 1.
- Figure 2.
- Figure 3.
- Figure 4.
- Figure 5.



 下载:
下载: