A pedigree study of laryngo-onycho-cutaneous syndrome with a novel mutation on LAMA3 gene
-
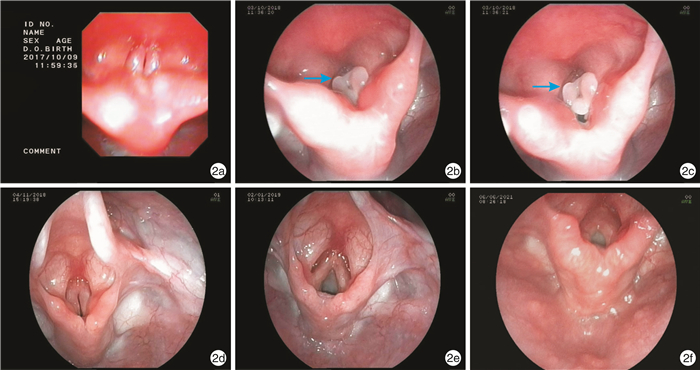
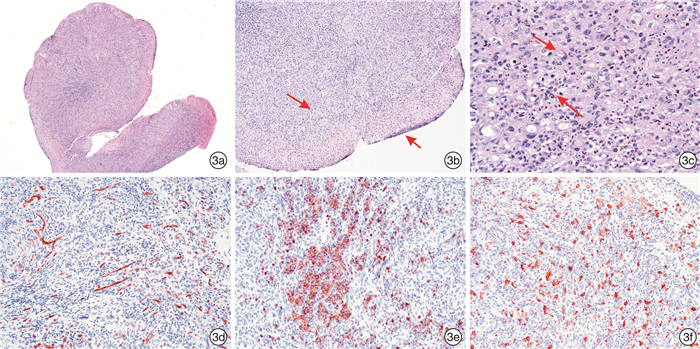
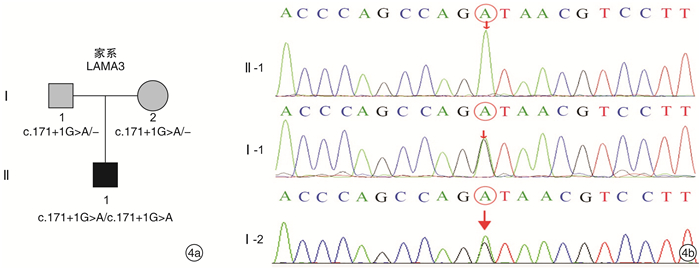
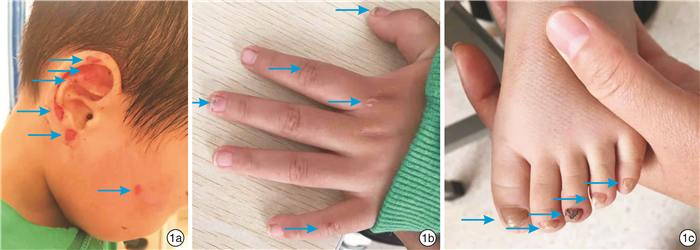
摘要: 目的 报道1例喉甲皮肤综合征,检测其基因突变,探讨可能的分子生物学致病原因。方法 采集先证者及其父母的外周血,提取DNA,高通量测序方法进行基因检测,对先证者及其家属进行突变位点的Sanger测序验证分析。结果 先证者基因检测发现LAMA3基因c.171+1G>A位点纯合突变,为剪接突变,是新发突变位点。先证者父母表型正常,基因检测出该位点杂合突变。结论 LAMA3基因c.171+1G>A纯合突变是先证者的可疑致病突变,该研究扩充了LAMA3基因的突变谱;喉甲皮肤综合征的临床表型表达具有高度可变性,多学科联合诊疗可有效避免漏诊和误诊。Abstract: Objective To detect genetic mutations in a case of laryngo-onycho-cutaneous syndrome, and to explore the possible molecular biological pathogenic causes.Methods With informed consent, the family clinical data of the child with laryngo-onycho-cutaneous syndrome were collected, peripheral blood of the protester and his parents was collected and DNA was extracted, and gene detection was performed by high-throughput sequencing method. Sanger sequencing was used to verify and analyze the mutation sites of the probs and their families.Results Genetic testing of the proband revealed homozygous mutation of LAMA3 gene c.171+1G>A site, which is splicing mutation. There was no report in the literature, which was a new mutation site. The parents of the proband had normal phenotype and heterozygous mutation at this locus was detected.Conclusion Homozygous mutation of LAMA3 c.171+1G>A is the likely pathogenic of the proband, and this study expands the mutant spectrum of LAMA3. The clinical phenotype of laryngo-onycho-cutaneous syndrome is highly variable, and the multidisciplinary diagnosis and treatment can effectively avoid missed diagnosis and misdiagnosis.
-
Key words:
- laryngo-onycho-cutaneous syndrome /
- LAMA3 gene /
- DNA mutational analysis
-

-
表 1 先证者LAMA3基因c.171+1G>A纯合突变
基因 染色体位置 转录本外显子 核苷酸氨基酸 纯合/杂合 正常人频率 REVEL预测 致病性分析 疾病/表型 遗传方式 变异来源 LAMA3 chr18-21453180 NM_001127718;exonl c.171+1G>A(splicing) hom 未知 未知 疑似致病性变异 ①LOCs;②Herlitz型交界型大疱性表皮松解症;③非Herlitz型交界型大疱性表皮松解症 ①常染色体隐性遗传;②常染色体隐性遗传;③常染色体隐性遗传 父母 -
[1] Diociaiuti A, Castiglia D, Naim M, et al. Autosomal recessive epidermolysis bullosa simplex due to KRT14 mutation: two large Palestinian families and literature review[J]. J Eur Acad Dermatol Venereol, 2018, 32(4): e149-e151. doi: 10.1111/jdv.14639
[2] Lin Z, Li S, Feng C, et al. Stabilizing mutations of KLHL24 ubiquitin ligase cause loss of keratin 14 and human skin fragility[J]. Nat Genet, 2016, 48(12): 1508-1516. doi: 10.1038/ng.3701
[3] 蒙岚岚, 杜娟, 李汶, 等. KRT14基因新突变导致的单纯型大疱性表皮松解症家系的研究[J]. 中华医学遗传学杂志, 2017, 34(4): 504-508. doi: 10.3760/cma.j.issn.1003-9406.2017.04.008
[4] 于越乾, 暴芳芳, 刘红. 遗传性大疱性表皮松解症致病基因研究进展[J]. 中国麻风皮肤病杂志, 2019, 35(6): 380-384. https://www.cnki.com.cn/Article/CJFDTOTAL-MALA201906024.htm
[5] 杜姿岑, 牟韵竹, 杨浩, 等. 痒疹样营养不良型大疱性表皮松解症一家系的临床表型及COL7A1基因突变检测[J]. 中华医学遗传学杂志, 2019, 36(5): 516-518. doi: 10.3760/cma.j.issn.1003-9406.2019.05.026
[6] Saxena P, Severi L, Santucci M, et al. Conformational Propensity and Biological Studies of Proline Mutated LR Peptides Inhibiting Human Thymidylate Synthase and Ovarian Cancer Cell Growth[J]. J Med Chem, 2018, 61(16): 7374-7380. doi: 10.1021/acs.jmedchem.7b01699
[7] Shu C, Yan D, Mo Y, et al. Long noncoding RNA lncARSR promotes epithelial ovarian cancer cell proliferation and invasion by association with HuR and miR-200 family[J]. Am J Cancer Res, 2018, 8(6): 981-992.
[8] Feng LY, Huang YZ, Zhang W, et al. LAMA3 DNA methylation and transcriptome changes associated with chemotherapy resistance in ovarian cancer[J]. J Ovarian Res, 2021, 14(1): 67. doi: 10.1186/s13048-021-00807-y
[9] Tang L, Wang P, Wang Q, et al. Correlation of LAMA3 with onset and prognosis of ovarian cancer[J]. Oncol Lett, 2019, 18(3): 2813-2818.
[10] 孔祥生, 刘江波, 陈付英, 等. 一例交界型大疱性表皮松解症患儿LAMA3基因突变检测[J]. 中国麻风皮肤病杂志, 2019, 35(5): 269-272. https://www.cnki.com.cn/Article/CJFDTOTAL-MALA201905004.htm
[11] Reimer A, Schwieger-Briel A, He Y, et al. Natural history and clinical outcome of junctional epidermolysis bullosa generalized intermediate due to a LAMA3 mutation[J]. Br J Dermatol, 2018, 178(4): 973-975. doi: 10.1111/bjd.16088
[12] Ahmad F, Shah K, Umair M, et al. Novel autosomal recessive LAMA3 and PLEC variants underlie junctional epidermolysis bullosa generalized intermediate and epidermolysis bullosa simplex with muscular dystrophy in two consanguineous families[J]. Clin Exp Dermatol, 2018, 43(6): 752-755. doi: 10.1111/ced.13610
[13] Has C, Liu L, Bolling MC, et al. Clinical practice guidelines for laboratory diagnosis of epidermolysis bullosa[J]. Br J Dermatol, 2020, 182(3): 574-592. doi: 10.1111/bjd.18128
[14] Mariath LM, Santin JT, Schuler-Faccini L, et al. Inherited epidermolysis bullosa: update on the clinical and genetic aspects[J]. An Bras Dermatol, 2020, 95(5): 551-569.
[15] Hammersen J, Has C, Naumann-Bartsch N, et al. Genotype, Clinical Course, and Therapeutic Decision Making in 76 Infants with Severe Generalized Junctional Epidermolysis Bullosa[J]. J Invest Dermatol, 2016, 136(11): 2150-2157.
-




 下载:
下载: