Correlation between conventional ultrasound features and BRAFV600E gene mutation and central lymph node metastasis in thyroid papillary carcinoma
-
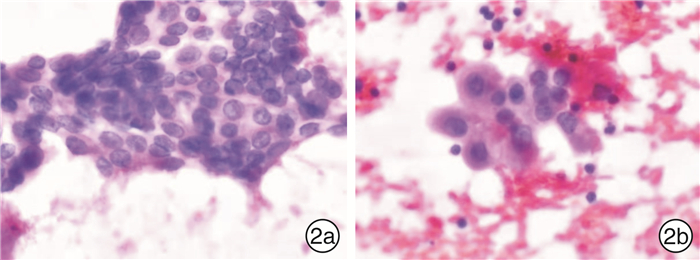
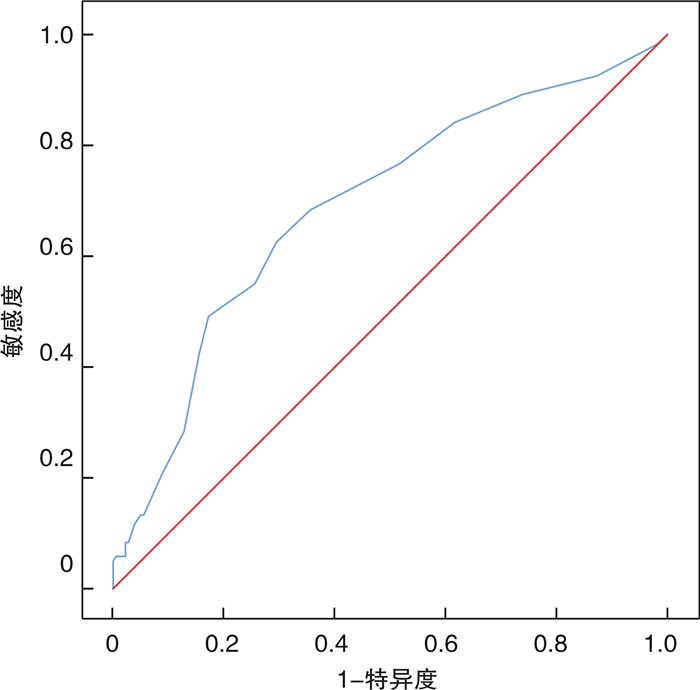
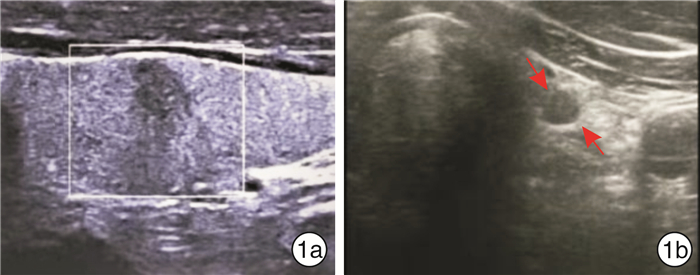
摘要: 目的 探讨甲状腺乳头状癌(PTC)中央区淋巴结转移(CLNM)与原发灶常规超声特征及BRAFV600E基因突变的相关性。方法 收集2019年10月—2021年6月经锦州医科大学附属第一医院手术病理确定为PTC并行中央区淋巴结清扫术的300例患者,根据中央区淋巴结是否发生转移分为转移组与非转移组,通过对两组患者原发病灶的常规超声特征及BRAFV600E基因检测结果分析确定其相关性。结果 300例PTC患者中,120例(40%)发生CLNM。单因素分析结果显示:性别、最大径线、病灶数、边界、形态、纵横比、靠近被膜、钙化及BRAFV600E基因突变的组间差异有统计学意义(P<0.05);Logistic多因素回归分析结果显示:性别、最大径线、纵横比、靠近被膜、微钙化及BRAFV600E为PTC患者CLNM的危险因素(P<0.05)。ROC曲线显示:当最大径为8.5 mm时,约登指数为最大值。结论 当PTC患者出现男性、最大径≥8.5 mm、纵横比≥1、微钙化、病灶靠近被膜及BRAFV600E(+)的危险因素时,应高度重视,尽早行预防性中央区淋巴结清扫。
-
关键词:
- 甲状腺乳头状癌 /
- BRAFV600E基因 /
- 淋巴结转移 /
- 超声特征
Abstract: Objective To investigate whether central lymph node metastasis(CLNM) in the central region of thyroid papillary carcinoma(PTC) is related to conventional ultrasound features of the primary lesion and BRAFV600E gene mutation.Methods A total of 300 patients with PTC confirmed by surgical pathology and central lymph node dissection in the First Affiliated Hospital of Jinzhou Medical University from October 2019 to June 2021 were collected. The subjects were divided into the metastatic group and the non-metastatic group according to whether CLNM occurred. The correlation was determined by analyzing the conventional ultrasound characteristics and BRAFV600E gene test results of the two groups of patients.Results Among 300 PTC patients, 120(40%) had CLNM. Univariate analysis showed that there were statistically significant differences between groups in gender, nodule maximum diameter line, number of lesions, boundaries, morphology, aspect ratio, proximity to the membrane, calcification and BRAFV600E gene mutation(P < 0.05). Logistic multivariate regression analysis showed that gender, maximum diameter line, aspect ratio, proximity to the membrane, microcalcification and BRAFV600E were the risk factors for CLNM in PTC patients(P < 0.05). ROC curve showed that when the maximum diameter was 8.5 mm, the Yooden index was the maximum.Conclusion When the risk factors of male, maximum diameter ≥8.5 mm, aspect ratio ≥1, microcalcification, proximity to capsule and BRAFV600E(+) appear in PTC patients, high attention should be paid to preventive CLN dissection as soon as possible. -

-
表 1 300例PTC患者常规超声特征及BRAFV600E基因突变与CLNM的单因素分析
研究因素 转移组(n=120) 非转移组(n=180) χ2/t P值 研究因素 转移组(n=120) 非转移组(n=180) χ2/t P值 年龄/岁 44±12 47±10 1.865 >0.05 纵横比 4.504 <0.05 性别 10.192 <0.01 ≥1 90(44.1) 114(55.9) 男 39(56.5) 30(43.5) <1 30(31.2) 66(68.8) 女 81(35.1) 150(64.9) 钙化 43.637 <0.01 结节数目 10.133 <0.01 无钙化 33(23.9) 105(76.1) 单发 69(33.8) 135(66.2) 微钙化 64(53.3) 56(46.7) 多发 51(53.1) 45(46.9) 粗钙化 10(34.5) 19(65.5) 最大径线/mm 11.4±7.9 7.5±4.3 4.922 <0.01 微-粗钙化 13(100.0) 0(0.0) 内回声 6.623 >0.05 位置 1.753 >0.05 极低回声 7(46.7) 8(53.3) 上极 26(35.1) 48(64.9) 低回声 102(38.5) 163(61.5) 中极 37(38.5) 59(61.5) 等回声 7(43.8) 9(56.2) 下极 46(44.7) 57(55.3) 强弱不均 4(100.0) 0(0.0) 峡部 11(40.7) 16(59.3) 边界 6.001 <0.05 合并桥本病 3.172 >0.05 清 25(29.1) 61(70.9) 是 17(54.8) 14(45.2) 不清 95(44.4) 119(55.6) 否 103(38.3) 166(61.7) 形态 4.792 <0.05 BRAFV600E 15.137 <0.01 规整 26(30.2) 60(69.8) 阳性 97(47.5) 107(52.5) 不规整 94(43.9) 120(56.1) 阴性 23(24.0) 73(76.0) 靠近被膜 46.808 <0.01 是 76(63.9) 43(36.1) 否 44(24.3) 137(75.7) 表 2 多因素Logistic回归分析CLNM的危险因素
研究因素 回归系数 标准误 Wald值 P值 OR值 95%CI 性别 0.766 0.352 4.742 <0.05 2.152 1.080~4.289 最大径线 0.086 0.033 6.874 <0.01 0.918 0.861~0.979 病灶数 0.515 0.328 2.467 >0.05 0.597 0.314~1.136 边界 0.194 0.351 0.307 >0.05 0.823 0.414~1.637 形态 0.033 0.359 0.008 >0.05 1.034 0.511~2.090 纵横比 0.822 0.350 5.517 <0.05 2.275 1.146~4.515 靠近被膜 1.508 0.310 23.617 <0.01 4.518 2.459~8.301 BRAFV600E 0.794 0.340 5.445 <0.05 2.212 1.135~4.308 微钙化 1.099 0.325 11.440 <0.01 0.333 0.176~0.630 -
[1] Erickson LA, Chen B. Papillary Thyroid Carcinoma BRAF Immunopositivity[J]. Mayo Clin Proc, 2021, 96(1): 267-268. doi: 10.1016/j.mayocp.2020.11.021
[2] Yuan J, Li J, Chen X, et al. Identification of risk factors of central lymph node metastasis and evaluation of the effect of prophylactic central neck dissection on migration of staging and risk stratification in patients with clinically node-negative papillary thyroid microcarcinoma[J]. Bull Cancer, 2017, 104(6): 516-523. doi: 10.1016/j.bulcan.2017.03.005
[3] 李云雪, 王刚, 孙备, 等. 甲状腺乳头状癌颈部淋巴结转移的处理态度和诊疗现状[J]. 实用肿瘤学杂志, 2020, 34(6): 530-534. https://www.cnki.com.cn/Article/CJFDTOTAL-SYZL202006012.htm
[4] Hu D, Zhou J, He W, et al. Risk factors of lateral lymph node metastasis in cN0 papillary thyroid carcinoma[J]. World J Surg Oncol, 2018, 16(1): 30. doi: 10.1186/s12957-018-1336-3
[5] 庄玲玲. 声像图所示甲状腺恶性结节钙化特点与组织病理类型分析[J]. 中国医学影像技术, 2019, 35(8): 1271-1273. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYXX201908054.htm
[6] Song L, Zhou J, Chen W, et al. Lymph node metastasis between the sternocleidomastoid and sternohyoid muscle in papillary thyroid carcinoma patients: A prospective study at multiple centers[J]. Asian J Surg, 2021, 44(8): 1043-1049. doi: 10.1016/j.asjsur.2021.01.005
[7] Zong S, Wang J, Wang Y, et al. Retrospective analysis of BRAFV600E gene mutation in 179 patients with papillary thyroid carcinoma[J]. J Modern Oncol, 2017, 25(13): 2052-2054.
[8] 江晶晶, 王建华, 丁文波, 等. FNAC联合BRAFV600E基因检测对甲状腺癌颈部淋巴结转移的诊断价值[J]. 中国普外基础与临床杂志, 2018, 25(9): 1083-1086. https://www.cnki.com.cn/Article/CJFDTOTAL-ZPWL201809012.htm
[9] Kim BY, Choi N, Kim SW, et al. Randomized trial of prophylactic ipsilateral central lymph node dissection in patients with clinically node negative papillary thyroid microcarcinoma[J]. Eur Arch Otorhinolaryngol, 2020, 277(2): 569-576. doi: 10.1007/s00405-019-05702-3
[10] 孙可敏, 何秀丽, 郭玲玲. 甲状腺微小乳头状癌临床及超声特征与中央区淋巴结转移的危险因素[J]. 临床耳鼻咽喉头颈外科杂志, 2021, 35(3): 260-263. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202103016.htm
[11] 兰雨, 宋青, 金壮, 等. 常规超声特征及BRAFV600E基因突变与甲状腺乳头状癌颈部淋巴结转移的相关性[J]. 解放军医学杂志, 2019, 44(9): 747-752. https://www.cnki.com.cn/Article/CJFDTOTAL-JFJY201909006.htm
[12] Shu X, Tang L, Hu D, et al. Prediction Model of Pathologic Central Lymph Node Negativity in cN0 Papillary Thyroid Carcinoma[J]. Front Oncol, 2021, 11: 727984. doi: 10.3389/fonc.2021.727984
[13] 詹玲, 孙圣荣. BRAFV600E基因突变与甲状腺乳头状癌腺外侵犯的相关性[J]. 中国普外基础与临床杂志, 2021, 28(9): 1159-1164. https://www.cnki.com.cn/Article/CJFDTOTAL-ZPWL202109003.htm
[14] 王欢, 柴芳, 林本瑞, 等. 合并桥本甲状腺炎的甲状腺乳头状癌中央区淋巴结转移的危险因素[J]. 中国老年学杂志, 2021, 41(7): 1396-1399. doi: 10.3969/j.issn.1005-9202.2021.07.015
[15] 李建聪, 梁荣华, 吴堂珍. 甲状腺钙化病灶在鉴别甲状腺良恶性结节中的作用[J]. 世界最新医学信息文摘, 2017, 17(35): 15-16. https://www.cnki.com.cn/Article/CJFDTOTAL-WMIA201735008.htm
[16] 陈名正, 符尚宏, 王雪峰, 等. 单发乳头状甲状腺癌患者侧颈淋巴结转移风险影响因素及与术前超声关系[J]. 临床军医杂志, 2021, 49(2): 151-152. https://www.cnki.com.cn/Article/CJFDTOTAL-JYGZ202102010.htm
[17] 傅迎霞, 张羽, 朱红, 等. 甲状腺乳头状癌颈侧区淋巴结转移的危险因素及影像诊断价值评估[J]. 医学影像学杂志, 2021, 31(8): 1287-1292. https://www.cnki.com.cn/Article/CJFDTOTAL-XYXZ202108008.htm
[18] 罗杰, 耿成义, 罗斌. 单侧甲状腺乳头状癌颈部中央区淋巴结转移的临床特点及影响因素[J]. 中国现代普通外科进展, 2020, 23(9): 704-707. https://www.cnki.com.cn/Article/CJFDTOTAL-PWJZ202009008.htm
-




 下载:
下载: