-
摘要: 目的 总结分析27例颞骨脑脊液漏患者的诊断及外科治疗。方法 回顾性分析27例颞骨脑脊液漏患者的临床资料,根据漏口部位以及患耳听力状况,采用不同的手术方案。术前漏口定位明确者经乳突径路或中颅窝径路直接修补伴或不伴乳突腹部脂肪填塞。漏口不明确、病变范围大或顽固性颞骨脑脊液漏患者,行岩骨次全切除术+腹部脂肪填塞。病变累及耳蜗者,行颞骨次全切除术+腹部脂肪填塞。结果 颞骨脑脊液漏的原因:内耳畸形患者13例;头外伤和手术后继发5例;特发性颅内高压和脑膜脑膨出5例;内耳感染2例;颞骨朗格汉斯组织细胞增多症2例。13例内耳畸形患者颞骨高分辨CT(HRCT)示内听道底骨质缺损同前庭交通;其余14例患者颞骨HRCT显示中颅窝或后颅窝骨质缺损,12例颞骨MRI显示脑膜连续性中断伴脑脊液流入颞骨或脑膜脑膨出。26例术后随访6个月~6年,1例患者失访。仅1例内耳畸形患者术后脑膜炎复发,行岩骨次全切+腹部脂肪填塞。7例患者术后听力保留或改善。所有患者均未出现严重的并发症,其中仅1例患者经乳突前庭池填塞术后出现HB Ⅱ级面瘫,面瘫1周内恢复。结论 颞骨脑脊液漏发病率低,保守治疗无效时应尽早采取外科干预措施。术前颞骨HRCT和MRI检查有利于漏口的定位,术式选择根据漏口的位置和病变性质不同采取个体化的手术方案。Abstract: Objective To study the clinical manifestations and surgical treatment of temporal bone cerebrospinal fluid leakage.Methods The clinical data of twenty seven cases with temporal bone cerebrospinal fluid leakage were analyzed retrospectively. Different surgical procedures were adopted according to the location of the leak and the hearing status of the affected ear.If the leakage location was clear before surgery, direct repair was performed via mastoid path or middle cranial fossa path with or without mastoid abdominal fat packing.For patients with unclear leak, large lesion or intractable CEREBROspinal fluid leakage of temporal bone, subtotal petrosal resection and abdominal fat packing were performed.Subtotal temporal bone resection and abdominal fat packing were performed for patients with cochlear involvement.Results In this study, cases of temporal bone CSF leakage including 13 cases of inner ear malformation; 5 cases secondary to head trauma or previous surgery, 5 cases of idiopathic intracranial hypertension or meningocele, 2 cases of langerhans histiocytosis in the temporal bone and 2 cases of inner ear inflammation. High resolution CT (HRCT) of temporal bone showed bone defect of inner auditory canal with vestibular communication in 13 patients with inner ear malformation.The temporal bone HRCT of the remaining 14 patients showed bone defects in the middle cranial fossa or posterior cranial fossa, while MRI of the temporal bone showed meningeal continuity interruption with cerebrospinal fluid inflow into the temporal bone or meningoencephalocele in 12 patients. The 26 patients were followed up from 6 months to 6 years. 1 patient lost follow-up.Meningitis recurred in only 1 patient with inner ear malformation, and subtotal resection of rock bone plus abdominal fat packing was performed.Postoperative hearing was preserved or improved in 7 patients.None of the patients had serious complications, and only 1 patient developed HB Grade Ⅱ facial paralysis after vestibular obliteration, and the facial paralysis recovered within one week.Conclusion Temporal bone cerebrospinal fluid leakage is relatively rare. Surgical intervention should be taken as early as possible when conservative treatment is failure. Preoperative HRCT and MRI examination are necessary for the localization of the leakage, and individualized surgical approaches can be adopted according to the location of the leakage and the features of the lesion.
-

-
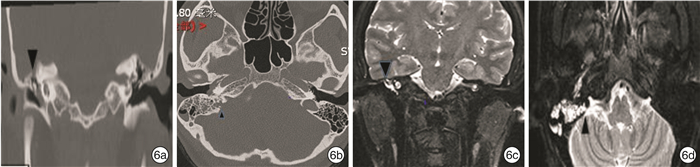
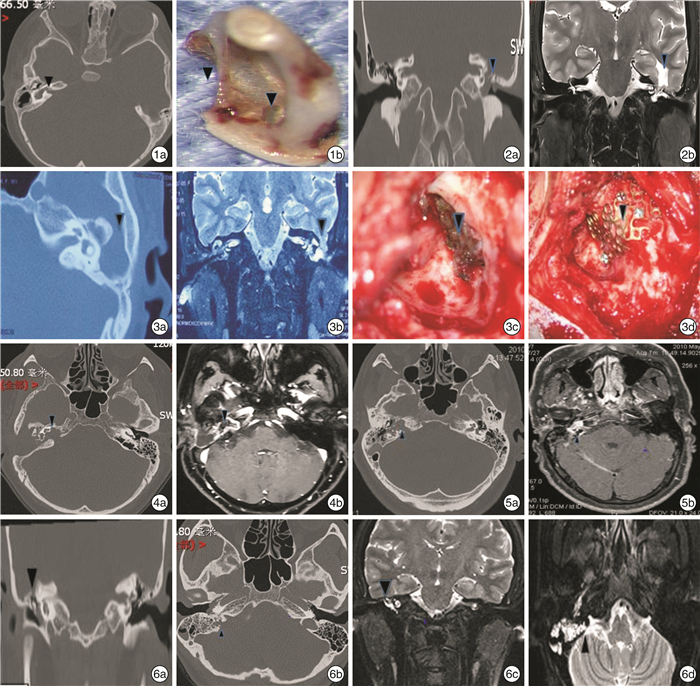
图 1 共同腔畸形患者CT及术中取出的镫骨 1a:右内耳同内听道直接交通(箭头);1b:内耳畸形患者,术中取出镫骨,可见镫骨底板前上及中央骨质缺损(箭头); 图 2 特发性颅高压伴中颅底脑膜脑膨出患者CT及MRI 2a:颞骨冠状位CT示鼓室天盖骨质吸收破坏(箭头);2b:颞骨MRI示脑膜脑膨出(箭头),伴中耳鼓室积液; 图 3 鼓室天盖低位患者外院乳突术后继发脑膜脑膨出及脑脊液漏CT、MRI及术中所见 3a:见鼓室天盖低位(箭头)(CT);3b:乳突手术后继发脑膜脑膨出及脑脊液漏(箭头)(MRI);3c:术中见乳突天盖骨质缺损4 cm×5 cm、脑膜脑膨出、脑脊液渗漏处(箭头),双极电凝后脑组织回缩;3d:中颅底缺损处用颞肌瓣+钛板修复(黑色箭头); 图 4 内耳朗格汉斯组织细胞增多症CT及MRI 4a:颞骨CT示耳蜗被侵蚀累及内听道(箭头);4b:颞骨MRI示内耳软组织部分增强(箭头)(患者乳突术后5年出现脑脊液漏并发脑膜炎,术后病理证实为内耳朗格汉斯组织细胞增多症); 图 5 内耳感染患者CT及MRI 5a:颞骨CT示特异性内耳被侵蚀破坏(箭头),并同内听道交通;5b:MRI见脑膜强化(箭头)(患者因脑膜炎就诊,术后病理为炎性肉芽组织)
表 1 27例患者的临床资料
例 病种 例数 并发症 复发 失访 共同腔畸形 4 0 1 0 Mondini畸形 9 1(面瘫) 0 1 特发性颅内高压 5 0 0 0 颞骨骨折 2 0 0 0 术后继发 3 0 0 0 朗格汉斯组织细胞增多症 2 0 0 0 内耳感染 2 0 0 0 合计 27 1 1 1 表 2 27例患者手术方案
例 病种 乳突入路前庭池填塞 乳突切除+漏口填塞+鼓窦软骨封闭+脂肪填塞 岩骨次全切+ 脂肪填塞+外耳道封闭 颞骨次全切+ 脂肪填塞+外耳道封闭 中颅窝乳突联合径路脑脊液漏修补和(或) 乳突脂肪填塞 共同腔畸形 3 2 Mondini畸形 9 特发性颅内高压 2 2 1 颞骨骨折 2 术后继发 2 1 朗格汉斯组织细胞增多症 1 1 内耳感染 2 合计 12 6 5 3 2 -
[1] Jackler RK, Luxford WM, House WF. Congenital malformations of the inner ear: a classification based on embryogenesis[J]. Laryngoscope, 1987, 97(3 Pt 2 Suppl 40): 2-14.
[2] Jinkins JR, Rudwan M, Krumina G, et al. Intrathecal gadolinium-enhanced MR cisternography in the evaluation of clinically suspected cerebrospinal fluid rhinorrhea in humans: early experience[J]. Radiology, 2002, 222(2): 555-559. doi: 10.1148/radiol.2222010249
[3] Oh MS, Vivas EX, Hudgins PA, et al. The Prevalence of Superior Semicircular Canal Dehiscence in Patients With Mastoid Encephalocele or Cerebrospinal Fluid Otorrhea[J]. Otol Neurotol, 2019, 40(4): 485-490. doi: 10.1097/MAO.0000000000002155
[4] Reddy M, Baugnon K. Imaging of Cerebrospinal Fluid Rhinorrhea and Otorrhea[J]. Radiol Clin N Am, 2017, 55(1): 167-187. doi: 10.1016/j.rcl.2016.08.005
[5] Vimala LR, Jasper A, Irodi A. Non-Invasive and Minimally Invasive Imaging Evaluation of CSF Rhinorrhoea-a Retrospective Study with Review of Literature[J]. Pol J Radiol, 2016, 81: 80-85. doi: 10.12659/PJR.895698
[6] Tolisano AM, Schauwecker N, Baumgart B, et al. Identifying Disadvantaged Groups for Cochlear Implantation: Demographics from a Large Cochlear Implant Program[J]. Ann Otol Rhinol Laryngol, 2020, 129(4): 347-354. doi: 10.1177/0003489419888232
[7] Kim L, Wisely CE, Dodson EE. Transmastoid approach to spontaneous temporal bone cerebrospinal fluid leaks: hearing improvement and success of repair[J]. Otolaryngol Head Neck Surg, 2014, 150(3): 472-478. doi: 10.1177/0194599813518173
[8] Carlson ML, Copeland WR 3rd, Driscoll CL, et al. Temporal bone encephalocele and cerebrospinal fluid fistula repair utilizing the middle cranial fossa or combined mastoid-middle cranial fossa approach[J]. J Neurosurg, 2013, 119(5): 1314-1322. doi: 10.3171/2013.6.JNS13322
[9] Sanna M, Fois P, Russo A, et al. Management of meningoencephalic herniation of the temporal bone: Personal experience and literature review[J]. Laryngoscope, 2009, 119(8): 1579-1585. doi: 10.1002/lary.20510
[10] Jackson CG, Pappas DG Jr, Manolidis S, et al. Brain herniation into the middle ear and mastoid: concepts in diagnosis and surgical management[J]. Am J Otol, 1997, 18(2): 198-205;discussion 205-206.
[11] Mosnier I, Fiky LE, Shahidi A, et al. Brain herniation and chronic otitis media: diagnosis and surgical management[J]. Clin Otolaryngol Allied Sci, 2000, 25(5): 385-391. doi: 10.1046/j.1365-2273.2000.00383.x
[12] Nahas Z, Tatlipinar A, Limb CJ, et al. Spontaneous meningoencephalocele of the temporal bone: clinical spectrum and presentation[J]. Arch Otolaryngol Head Neck Surg, 2008, 134(5): 509-518., doi: 10.1001/archotol.134.5.509
[13] Scurry WC Jr, Ort SA, Peterson WM, et al. Idiopathic temporal bone encephaloceles in the obese patient[J]. Otolaryngol Head Neck Surg, 2007, 136(6): 961-965. doi: 10.1016/j.otohns.2006.11.036
[14] Lundy LB, Graham MD, Kartush JM, et al. Temporal bone encephalocele and cerebrospinal fluid leaks[J]. Am J Otol, 1996, 17(3): 461-469.
[15] Gubbels SP, Selden NR, Delashaw JB Jr, et al. Spontaneous middle fossa encephalocele and cerebrospinal fluid leakage: diagnosis and management[J]. Otol Neurotol, 2007, 28(8): 1131-1139. doi: 10.1097/MAO.0b013e318157f7b6
[16] Sdano MT, Pensak ML. Temporal bone encephaloceles[J]. Curr Opin Otolaryngol Head Neck Surg, 2005, 13(5): 287-289. doi: 10.1097/01.moo.0000179247.51476.f5
[17] Gacek RR, Gacek MR, Tart R. Adult spontaneous cerebrospinal fluid otorrhea: diagnosis and management[J]. Am J Otol, 1999, 20(6): 770-776.
[18] Yi HJ, Guo H, Ch W, et al. Use of the translabyrinthine approach to repair congenital spontaneous cerebrospinal fluid leakage in five Chinese patients with Mondini dysplasia[J]. Int J Pediatr Otorhinolaryngol, 2013, 77(12): 1965-1968. doi: 10.1016/j.ijporl.2013.09.012
[19] Isaacson B, Hunter JB, Rivas A. Endoscopic stapes surgery[J]. Otolaryngol Clin North Am, 2018, 51(2): 415-428. doi: 10.1016/j.otc.2017.11.011
[20] Kou YF, Zhu VF, Kutz JW, et al. Transcanal Endoscopic Management of Cerebrospinal Fluid Otorrhea Secondary to Congenital Inner Ear Malformations[J]. Otol Neurotol, 2016, 37(1): 62-65, doi: 10.1097/MAO.0000000000000898
[21] Deng W, Liu J, Pang F, et al. Diagnosis and management of pediatric cerebrospinal fluid leakage secondary to inner ear malformations: A report of 13 cases[J]. Intl J Pediatr Otorhinolaryngol, 2020, 135: 110049. doi: 10.1016/j.ijporl.2020.110049
[22] Stevens SM, Crane R, Pensak ML, et al. Middle Ear Obliteration with Blind-Sac Closure of the External Auditory Canal for Spontaneous CSF Otorrhea[J]. Otolaryngol Head Neck Surg, 2017, 157(3): 5334-5542.
[23] Stevens SM, Crane R, Pensak ML, et al. Analysis of Audiometric Outcomes following Combined Middle Cranial Fossa/Transmastoid Approaches for Spontaneous Cerebrospinal Fluid Otorrhea[J]. Otolaryngol Head Neck Surg, 2017, 156(5): 924-932. doi: 10.1177/0194599817690726
-

| 引用本文: | 陈晓红, 李伟, 李海同, 等. 颞骨脑脊液漏27例的外科治疗总结[J]. 临床耳鼻咽喉头颈外科杂志, 2021, 35(11): 998-1003. doi: 10.13201/j.issn.2096-7993.2021.11.008 |
| Citation: | CHEN Xiaohong, LI Wei, LI Haitong, et al. Surgical management of 27 cases with temporal bone cerebrospinal fluid leakage[J]. J Clin Otorhinolaryngol Head Neck Surg, 2021, 35(11): 998-1003. doi: 10.13201/j.issn.2096-7993.2021.11.008 |
- Figure 1.
- Figure 6.



 下载:
下载: