Application of high frequency jet ventilation system in laryngopharyngeal and tracheal surgery
-
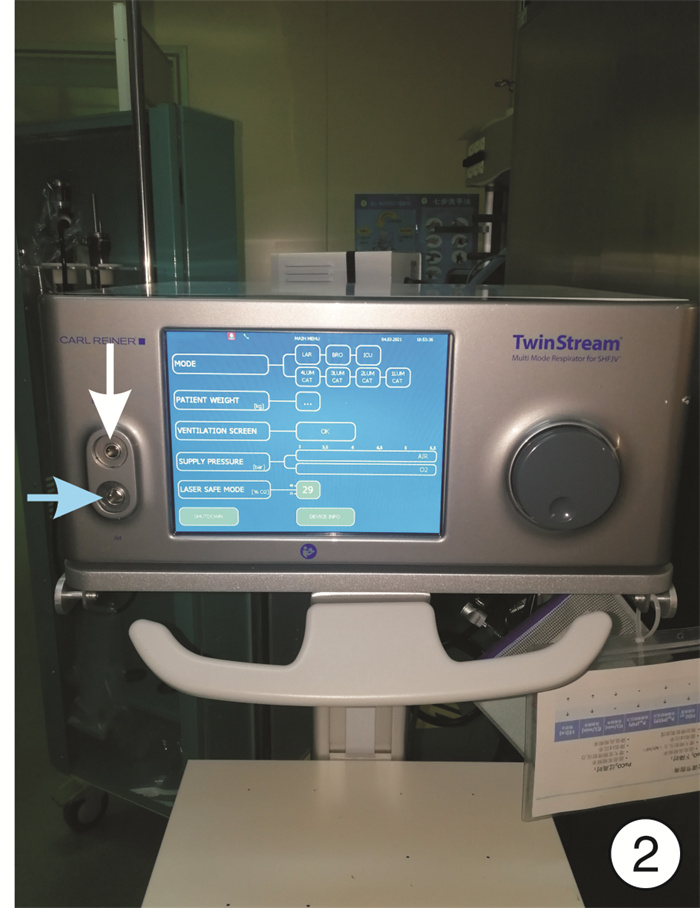
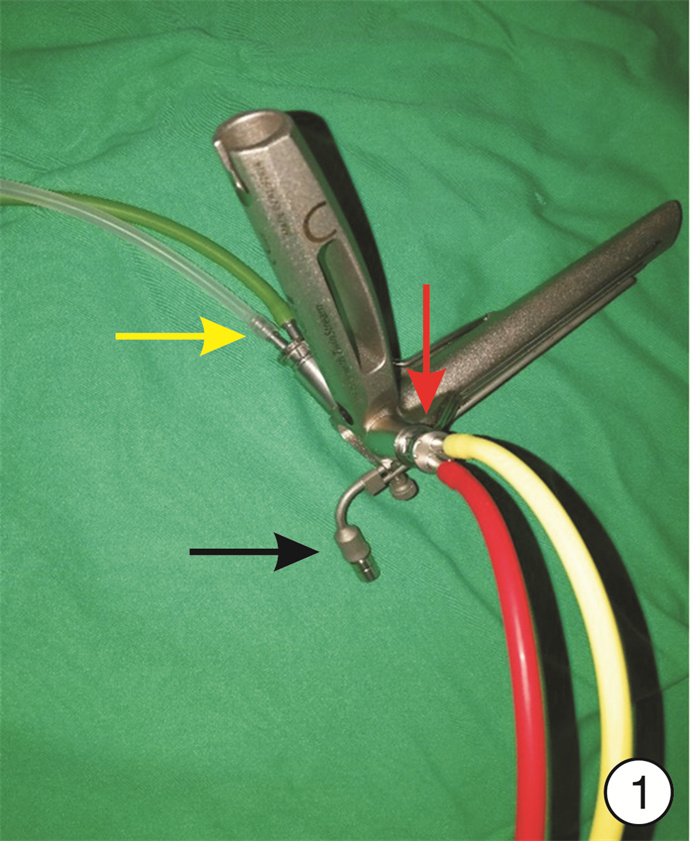
摘要: 目的 探讨高频通气手术系统在咽喉气管手术中应用的有效性及安全性。方法 将符合美国麻醉医师协会分级标准Ⅰ~Ⅱ级, 且拟在全身麻醉下行择期咽喉气管手术的60例患者随机分为高频喷射通气(HFJV)组和间歇正压通气(IPPV)组各30例。HFJV组借助高频喷射呼吸机行HFJV, IPPV组通过小口径气管导管接麻醉机行IPPV。在麻醉前(T0)、支撑喉镜放置成功后(T1)、通气5 min后(T2)及支撑喉镜取出5 min后(T3)各时间点记录血流动力学指标, 在T0、T2和T3各时间点测量动脉血气指标, 同时记录平均气道压、呼气末二氧化碳浓度、手术视野质量、总出血量、手术时间和苏醒时间, 对比2组方案对上述指标的影响并记录不良事件发生情况。结果 HFJV组的平均气道压、平均总出血量明显低于IPPV组(P < 0.01), 而且HFJV组的平均手术视野质量明显更好(P < 0.01), 但对血流动力学、动脉血气等指标的影响与IPPV组相比差异均无统计学意义(P>0.05)。2组均未发生严重不良事件。结论 高频通气手术系统可有效地应用于咽喉气管手术, 减少术中出血量, 改善手术视野质量, 且无明显不良反应。Abstract: Objective The effectiveness and safety of high frequency ventilation system in laryngopharyngeal and tracheal surgery is discussed.Methods According to The American Society of Anesthesiologists Ⅰ-Ⅱ level, 60 cases of selective throat and tracheal surgery undering general anesthesia were randomly divided into high frequency jet ventilation group (group HFJV) and intermittent positive pressure ventilation group (IPPV group), with 30 cases in each group. Group HFJV was treated with HFJV and group IPPV with a small caliber endotracheal tube connected to an anesthesia machine was treated with IPPV.Before anesthesia (T0), after the success of the laryngoscope placed (T1), 5 minites after ventilation (T2) and 5 minites after the laryngoscope removed (T3), hemodynamic parameters were recorded at each time point, in T0, T2 and T3 record, arterial blood gas index, the patient's airway pressure, end-expiratory carbon dioxide concentration, surgical field quality and total blood loss, operating time and awakening time were recorded and compared between the two groups.Results The average airway pressure and intraoperative average total blood loss of group HFJV were significantly lower than that of group IPPV(P < 0.01), and the average operative field quality of group HFJV was significantly better(P < 0.01), but there was no statistical significance in the effects on hemodynamics, arterial blood gas and other indicators compared with group IPPV(P>0.05). No serious adverse events occurred in 2 groups.Conclusion HFJV system can be used effectively in laryngopharyngeal and tracheal surgery, reducing intraoperative blood loss and improving surgical field of vision without obvious adverse reactions.
-

-
表 1 2组患者的疾病分类情况及手术方式
疾病分类 HFJV组
(30例)IPPV组
(30例)手术方式 声带息肉 15 13 支撑喉镜下息肉切除术 会厌囊肿 9 12 支撑喉镜下囊肿切除术 喉乳头状瘤 1 2 支撑喉镜下CO2激光肿瘤切除术 喉恶性肿瘤 3 2 支撑喉镜下CO2激光喉部分切除术 气管异物 2 1 气管异物取出术 表 2 2组患者的HR、MAP及SpO2变化比较
x±s 组别 T0 T1 T2 T3 HFJV组(n=30) HR/(次·min-1) 82.10±13.04 87.30±5.77 85.90±10.84 85.30±10.99 MAP/mmHg 92.05±12.70 85.65±11.14 95.85±15.27 95.05±17.24 SpO2/% 94.20±3.04 98.85±2.23 98.25±3.13 98.00±2.97 IPPV组(n=30) HR/(次·min-1) 79.70±7.06 91.85±8.12 90.20±6.74 87.80±5.79 MAP/mmHg 89.90±11.29 78.20±15.75 86.70±20.32 85.85±18.84 SpO2/% 94.65±3.30 98.60±1.27 99.10±0.85 96.85±9.21 表 3 2组患者的平均动脉血气指标比较
x±s 组别 T0 T2 T3 HFJV组(n=30) PH 7.42±0.04 7.33±0.14 7.36±0.03 PaO2/mmHg 82.56±43.04 189.76±84.74 117.08±32.98 PaCO2/mmHg 34.35±4.92 40.23±10.76 43.38±9.27 SaO2/% 94.38±2.54 97.94±2.32 97.40±1.70 IPPV组(n=30) PH 7.43±0.03 7.39±0.04 7.38±0.04 PaO2/mmHg 71.08±9.95 244.25±79.11 128.22±38.59 PaCO2/mmHg 35.12±4.36 38.21±7.09 41.12±6.36 SaO2/% 93.78±2.08 98.84±0.78 97.46±2.25 表 4 2组患者手术相关指标比较
x±s 指标 HFJV组
(n=30)IPPV组
(n=30)P 平均手术时间/min 21.60±10.76 18.05±9.96 >0.05 平均苏醒时间/min 47.05±7.33 45.15±14.59 >0.05 平均MAWP/mmHg 4.10±0.72 5.45±0.94 <0.01 平均ETCO2/mmHg 33.55±1.67 33.85±2.76 >0.05 平均总出血量/mL 1.50±0.61 2.85±1.09 <0.01 平均手术视野质量 1.29±0.36 1.82±0.49 <0.01 -
[1] Li S, Liu Y, Tan F, et al. Efficacy of manual jet ventilation using Manujet III for bronchoscopic airway foreign body removal in children[J]. Int J Pediatr Otorhinolaryngol, 2010, 74(12): 1401-1404. doi: 10.1016/j.ijporl.2010.09.018
[2] Boezaart AP, van der Merwe J, Coetzee A. Comparison of sodium nitroprusside-and esmolol-induced controlled hypotension for functional endoscopic sinus surgery[J]. Can J Anaesth, 1995, 42(5 Pt 1): 373-376.
[3] Soni N, Williams P. Positive pressure ventilation: what is the real cost?[J]. Br J Anaesth, 2008, 101(4): 446-457. doi: 10.1093/bja/aen240
[4] Dutton RP. Controlled hypotension for spinal surgery[J]. Eur Spine J, 2004, 13 Suppl 1(Suppl 1): S66-71.
[5] Kubitz JC, Kemming GI, Schultheiss G, et al. The influence of PEEP and tidal volume on central blood volume[J]. Eur J Anaesthesiol, 2006, 23(11): 954-961. doi: 10.1017/S0265021506000925
[6] Ihra G, Gockner G, Kashanipour A, et al. High-frequency jet ventilation in European and North American institutions: developments and clinical practice[J]. Eur J Anaesthesiol, 2000, 17(7): 418-430. doi: 10.1097/00003643-200007000-00003
[7] 郭金洋, 吴太虎, 万振. 高频通气的现状与发展[J]. 医疗卫生装备, 2008, 29(4): 35-37. doi: 10.3969/j.issn.1003-8868.2008.04.014
[8] 付丹, 何颜霞. 高频通气的临床应用[J]. 中国实用儿科杂志, 2010, 2(1): 20-24. https://www.cnki.com.cn/Article/CJFDTOTAL-ZSEK201002010.htm
[9] Ross-Anderson DJ, Ferguson C, Patel A. Transtracheal jet ventilation in 50 patients with severe airway compromise and stridor[J]. Br J Anaesth, 2011, 106(1): 140-144. doi: 10.1093/bja/aeq278
[10] Altun D, Çamcı E, Orhan-Sungur M, et al. High frequency jet ventilation during endolaryngeal surgery: Risk factors for complications[J]. Auris Nasus Larynx, 2018, 45(5): 1047-1052. doi: 10.1016/j.anl.2017.12.003
[11] Biro P. Jet ventilation for surgical interventions in the upper airway[J]. Anesthesiol Clin, 2010, 28(3): 397-409. doi: 10.1016/j.anclin.2010.07.001
[12] Klain M, Keszler H. High-frequency jet ventilation[J]. Surg Clin North Am, 1985, 65(4): 917-930. doi: 10.1016/S0039-6109(16)43687-X
[13] Berkenbosch JW, Tobias JD. Transcutaneous carbon dioxide monitoring during high-frequency oscillatory ventilation in infants and children[J]. Crit Care Med, 2002, 30(5): 1024-1027. doi: 10.1097/00003246-200205000-00011
[14] Evans KL, Keene MH, Bristow AS. High-frequency jet ventilation--a review of its role in laryngology[J]. J Laryngol Otol, 1994, 108(1): 23-25. doi: 10.1017/S0022215100125733
[15] Guenard H, Cros AM, Boudey C. Variations in flow and intraalveolar pressure during jet ventilation: theoretical and experimental analysis[J]. Respir Physiol, 1989, 75(2): 235-245. doi: 10.1016/0034-5687(89)90067-4
[16] Dias NH, Martins RH, Braz JR, et al. Larynx and cervical trachea in humidification and heating of inhaled gases[J]. Ann Otol Rhinol Laryngol, 2005, 114(5): 411-415. doi: 10.1177/000348940511400514
[17] Doyle HJ, Napolitano AE, Lippman HR, et al. Different humidification systems for high-frequency jet ventilation[J]. Crit Care Med, 1984, 12(9): 815-819. doi: 10.1097/00003246-198409000-00031
[18] Galmén K, Harbut P, Freedman J, et al. The use of high-frequency ventilation during general anaesthesia: an update[J]. F1000Res, 2017, 6: 756. doi: 10.12688/f1000research.10823.1
[19] Galmén K, Jakobsson JG, Freedman J, et al. Post-operative hypertension during early recovery following liver tumour ablation: A retrospective study[J]. Acta Anaesthesiol Scand, 2021.
-




 下载:
下载: