Risk prediction and malignant transformation in vocal cord leukoplakia based on electronic laryngoscope
-
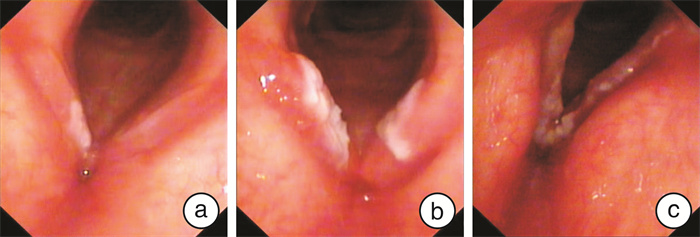
摘要: 目的 探讨电子喉镜下对声带白斑性质的风险预测及癌变的相关影响因素。方法 回顾性分析163例声带白斑患者电子喉镜下病变的部位、范围、形态分型、是否累及前连合与组织病理级别的关系, 并采用多元Logistic回归模型分析癌变的相关因素。结果 163例患者中, 单侧病变者96例(58.9%), 双侧病变者67例(41.1%); 病变范围未超过一侧声带全长1/2共135例(82.8%), 超过一侧声带全长1/2共28例(17.1%); 病变未累及前连合121例(74.2%), 累及前连合42例(25.8%)。电子喉镜下声带白斑形态为平坦型82例(50.3%), 增生型65例(39.9%), 溃疡型16例(9.8%)。组织病理学分型为单纯性增生65例(39.9%), 轻度异型性增生44例(27.0%), 中度异型性增生31例(19.0%), 重度异型性增生和原位癌23例(14.1%)。低危组140例(85.9%), 高危组23例(14.1%)。声带白斑病变的部位与病理等级无相关性(P>0.05);声带白斑的范围是否超过声带全长1/2以及是否累及前连合与病理等级存在相关性(均P < 0.05);声带白斑形态学分型与病理等级存在差异(P < 0.01)。癌变10例, 癌变率为6.1%。多元Logistic回归分析表明, 声带白斑的病理学等级和是否累及前连合是声带白斑癌变的独立危险因素。结论 通过电子喉镜可以初步判断声带白斑的风险程度, 声带白斑的病变范围越大、形态学分型级别越高和累及前连合者, 病理学等级越高; 组织病理等级及是否累及前连合是癌变的影响因素。Abstract: Objective To investigate the predictive risk factors of vocal fold leukoplakia under electronic laryngoscope and influential factors of malignancy.Methods A total of 163 cases with vocal cord leukoplakia were analyzed retrospectively. The relationship between the clinical features, including site, size, whether involving the anterior commissure, morphology and pathological grade were analyzed. Then the associations with malignant transformation in vocal cord leukoplakia were evaluated by using multiple Logistic regression analysis.Results There were one side lesions in 96 cases(58.9%), and bilateral vocal cord lesions in 67 cases(41.1%). The vocal cord leukoplakia with extension less than half of the vocal cord was observed in 135 cases(82.8%) and beyond half of the vocal cord was seen in 28 cases(17.1%). Lesions involving the anterior commissure were 42 cases(25.8%), without involving the anterior commissure were 121 cases(74.2%). According to morphological features, 82 patients(50.3%) had a superficial type, followed by exophytic type(n=65, 39.9%), and ulcerative type(n=16, 9.8%). The pathological type included squamous epithelial simple hyperplasia in 65 cases(39.9%), mild hyperplasia in 44 cases(27.0%), moderate hyperplasia in 31 cases(19.0%), severe hyperplasia and carcinoma in situ in 23 cases(14.1%). 140 cases(85.9%) were in low risk group, and 23 cases(14.1%) were in high risk group. The site of the vocal fold leukoplakia was not associated with the pathological grade(P>0.05), whether the vocal fold leukoplakia range exceeds 1/2 of the total length of the vocal fold, and whether involving the anterior commissure were associated with the pathological grade(both P < 0.05). There were statistically significant differences between the pathological grade and the morphological type(P < 0.01). Ten cases developed larynx cancer, the ratio of malignant transformation was 6.1%. The multiple Logistic regression showed that whether involving the anterior commissure and histopathological classification were the risk factors of malignant transformation in vocal cord eukoplakia.Conclusion The pathological results of vocal cord leukoplakia can be predicted by laryngoscopy features. Involving of the anterior commissure and histopathological classification are the risk factors of malignant transformation in vocal cord leukoplakia.
-
Key words:
- vocal cord leukoplakia /
- electronic laryngoscope /
- pathology /
- malignant transformation
-

-
表 1 声带白斑喉镜下特征与病理学相关性分析
相关因素 单纯性增生 轻度异型性增生 中度异型性增生 重度异型性增生和原位癌 P(Z或H) 部位 单侧 34(35.4) 26(27.1) 19(19.8) 17(17.7) 0.087(-1.714) 双侧 31(46.3) 18(26.9) 12(17.9) 6(8.9) 范围 ≤1/2 62(45.9) 37(27.4) 20(14.8) 16(11.9) <0.001(-3.947) >1/2 3(10.7) 7(25.0) 11(39.3) 7(25.0) 累及前连合 是 15(35.7) 6(14.3) 9(21.4) 12(28.6) 0.036(-2.091) 否 50(41.3) 38(31.4) 22(18.2) 11(9.1) 白斑形态 平坦型 41(50.0) 27(32.9) 13(15.9) 1(1.2) 增生型 23(35.4) 16(24.6) 14(21.5) 12(18.5 <0.001(31.614) 溃疡型 1(6.2) 1(6.2) 4(25.0) 10(62.5) 表 2 声带白斑癌变与临床病理特征相关性分析
分类 未癌变
(n=153)癌变
(n=10)P(χ2) 部位 单侧 88(91.7) 8(8.3) 0.162(1.960) 双侧 65(97.0) 2(3.0) 范围 ≤1/2 126(93.3) 9(6.7) 0.535(0.386) >1/2 27(96.4) 1(3.6) 累及前连合 是 36(85.7) 6(14.3) 0.011(6.527) 否 117(96.7) 4(3.3) 白斑形态 平坦型 81(98.8) 1(1.2) 增生型 63(96.9) 2(3.1) <0.001(43.808) 溃疡型 9(56.2) 7(43.8) 病理学 低危组 138(98.6) 2(1.4) <0.001(38.164) 高危组 15(65.2) 8(34.8) 表 3 癌变相关因素的Logistic回归分析
相关因素 回归系数 标准误 Wald P 累及前连合 1.584 0.673 5.540 0.019 白斑形态 1.382 1.955 0.964 0.137 病理学 3.065 0.836 18.600 <0.001 -
[1] Panwar A, Lindau R 3rd, Wieland A. Management of premalignant lesions of the larynx[J]. Expert Rev Anticancer Ther, 2013, 13(9): 1045-1051. doi: 10.1586/14737140.2013.829643
[2] Li C, Zhang N, Wang S, et al. A new classification of vocal fold leukoplakia by morphological appearance guiding the treatment[J]. Acta Otolaryngol, 2018, 138(6): 584-589. doi: 10.1080/00016489.2018.1425000
[3] Barnes L, Eveson JW, Reichart P, et, al. World Health Organization classification of tumor. Pathology and genetics of head and neck tumors[M]. Lyon: IARCS Press, 2005: 140-143.
[4] Gale N, Poljak M, Zidar N. Update from the 4th Edition of the World Health Organization Classification of Head and Neck Tumours: What is New in the 2017 WHO Blue Book for Tumours of the Hypopharynx, Larynx, Trachea and Parapharyngeal Space[J]. Head Neck Pathol, 2017, 11(1): 23-32. doi: 10.1007/s12105-017-0788-z
[5] Rutt AL, Wang C, Li Z. Clinicopathologic Aspects of Vocal Fold Leukoplakia in Smokers and Nonsmokers[J]. J Voice, 2020.
[6] 王文伦, 张立红, 曹杰, 等. 声带白斑的发病因素及临床特点分析[J]. 中华耳鼻咽喉头颈外科杂志, 2018, 53(8): 581-586. doi: 10.3760/cma.j.issn.1673-0860.2018.08.005
[7] Parker NP. Vocal fold leukoplakia: incidence, management, and prevention[J]. Curr Opin Otolaryngol Head Neck Surg, 2017, 25(6): 464-468. doi: 10.1097/MOO.0000000000000406
[8] Karatayli-Ozgursoy S, Pacheco-Lopez P, Hillel AT, et al. Laryngeal dysplasia, demographics, and treatment: a single-institution, 20-year review[J]. JAMA Otolaryngol Head Neck Surg, 2015, 141(4): 313-318. doi: 10.1001/jamaoto.2014.3736
[9] Mehanna H, Paleri V, Robson A, et al. Consensus statement by otorhinolaryngologists and pathologists on the diagnosis and management of laryngeal dysplasia[J]. Clin Otolaryngol, 2010, 35(3): 170-176. doi: 10.1111/j.1749-4486.2010.02119.x
[10] Weller MD, Nankivell PC, McConkey C, et al. The risk and interval to malignancy of patients with laryngeal dysplasia; a systematic review of case series and meta-analysis[J]. Clin Otolaryngol, 2010, 35(5): 364-372. doi: 10.1111/j.1749-4486.2010.02181.x
[11] Lu G, Guo W, Zhang Q, et al. Endoscopic diagnosis value of narrow band imaging Ni classification in vocal fold leukoplakia and early glottic cancer[J]. Am J Otolaryngol, 2021, 42(3): 102904. doi: 10.1016/j.amjoto.2021.102904
[12] 朱国臣, 肖大江, 孙屏. 窄带成像内镜技术在克服声带白斑遮蔽黏膜微血管形态中的应用[J]. 临床耳鼻咽喉头颈外科杂志, 2019, 33(6): 542-545. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201906018.htm
[13] Chen M, Li C, Yang Y, et al. A morphological classification for vocal fold leukoplakia[J]. Braz J Otorhinolaryngol, 2019, 85(5): 588-596. doi: 10.1016/j.bjorl.2018.04.014
[14] Fang TJ, Lin WN, Lee LY, et al. Classification of vocal fold leukoplakia by clinical scoring[J]. Head Neck, 2016, 38 Suppl 1: E1998-2003.
[15] Zhang N, Cheng L, Chen M, et al. Relationship between laryngoscopic and pathological characteristics of vocal cords leukoplakia[J]. Acta Otolaryngol, 2017, 137(11): 1199-1203. doi: 10.1080/00016489.2017.1347826
[16] 郑重, 万光伦, 陈浩, 等. 声带白斑的喉镜特征与病理相关性分析[J]. 听力学及言语疾病杂志, 2020, 28(3): 239-242. doi: 10.3969/j.issn.1006-7299.2020.03.001
[17] Anis MM. Correlating laryngoscopic appearance of laryngeal lesions with histopathology[J]. Laryngoscope, 2019, 129(6): 1308-1312. doi: 10.1002/lary.27585
[18] Thompson LD. Laryngeal Dysplasia, Squamous Cell Carcinoma, and Variants[J]. Surg Pathol Clin, 2017, 10(1): 15-33. doi: 10.1016/j.path.2016.10.003
[19] Kim CM, Chhetri DK. Triological Best Practice: When Is Surgical Intervention Indicated for Vocal Fold Leukoplakia?[J]. Laryngoscope, 2020, 130(6): 1362-1363. doi: 10.1002/lary.28527
[20] 崔卫新, 徐文, 杨庆文, 等. 声带白斑临床病理特征及复发癌变的影响因素[J]. 临床耳鼻咽喉头颈外科杂志, 2016, 30(24): 1926-1931. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201624007.htm
-




 下载:
下载: