Establishment of a predictive model for central cervical lymph node metastasis of papillary thyroid carcinoma based on ACR TI-RADS score and evaluation of its diagnostic efficacy
-
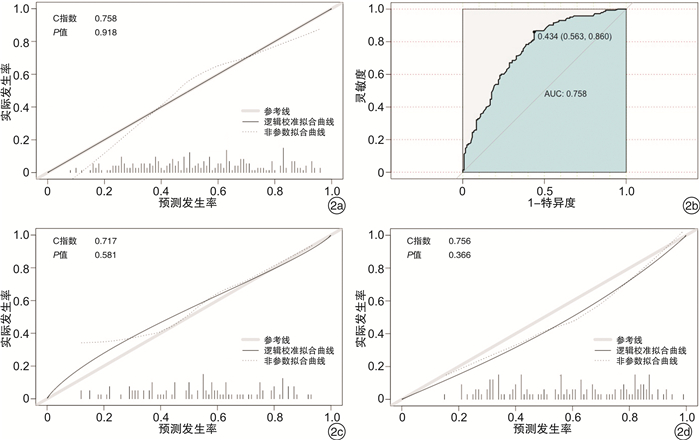
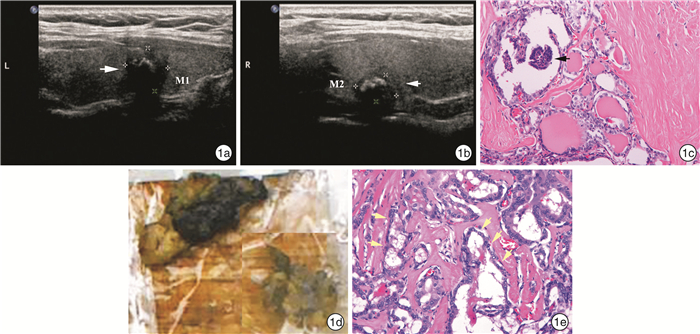
摘要: 目的 基于美国放射学会甲状腺影像报告和数据系统(ACR TI-RADS)构建甲状腺乳头状癌(PTC)颈中央区淋巴结转移(CLNM)的风险预测模型,并评估其诊断效能。方法 纳入2019年1月—2020年5月确诊为PTC的患者319例,共366枚结节作为建模队列,构建风险预测模型(ATR模型);纳入2020年6—8月的PTC患者105例,共121枚结节作为外部验证队列。计算模型C统计量(C-index)并进行拟合优度检验,对比ATR模型与颈部超声(C-US)、电子计算机断层扫描(CT)的诊断效能。结果 ATR模型为:Y=-3.719+0.765×性别+1.094×病灶数量+0.08×最大径+0.266×ACR评分。在建模队列训练集、测试集及外部验证队列中,模型C-index分别为:0.758(95%CI:0.699~0.817),0.717(95%CI:0.619~0.815)及0.756(95%CI:0.671~0.840)。Hosmer-Lemeshow拟合优度检验表明模型预测率与实际发生率的一致性好(P=0.918,P=0.581,P=0.366)。以≥0.434为诊断截值,模型的诊断效能最高(灵敏度:86.0%,特异度:56.3%,约登指数:0.423),在外部验证队列中,C-US与CT的诊断效能比较,各指标均无明显差异(P>0.05);与C-US、CT检查相比,ATR模型诊断灵敏度(66.1%和16.1%,P < 0.001;66.1%和9.7%,P < 0.001),符合率(68.6%和55.4%,P=0.041;68.6%和52.9%,P=0.012)均较高,阴性预测值高于CT(66.7%和50.9%,P=0.042),而与C-US无差异(66.7%和52.3%,P=0.066);阳性预测值(70.7%和83.3%,P=0.211;70.7%和85.7%,P=0.319;83.3%和85.7%,P=0.713)三者无明显差异,而模型特异度(71.2%和96.6%,P=0.001;71.2%和98.3%,P < 0.001)较低。结论 基于ACR TI-RADS评分所构建的风险预测模型较传统影像学检查可以更准确、敏感地预测CLNM。Abstract: Objective To establish a predictive model for central lymph node metastasis(CLNM) of papillary thyroid carcinoma(PTC) based on ACR TI-RADS grades(ATR model) and evaluate its diagnostic efficacy.Methods A total of 319 patients with PTC diagnosed from January 2019 to May 2020 were included, including 366 nodules were used as the modeling cohort to construct the risk prediction model. A total of 105 PTC patients with 121 nodules from June to August 2020 were included as the external validation cohort. The C-index of the model was calculated and the Hosmer-Lemeshow goodness-of-fit test was performed to compare the diagnostic efficiency of ACR model and those conventional imaging models.Results The ATR model, Y=-3.719+0.765×gender+1.094×multifocality+0.08×maximum diameter+0.266×ACR TI-RADS score. In the training set, validation set and external validation cohort, the model C-index was 0.758(95%CI: 0.699-0.817), 0.717(95%CI: 0.619-0.815) and 0.756(95%CI: 0.671-0.840), respectively. The Hosmer-Lemeshow goodness of fit test showed that the prediction rate of the model was consistent with the actual incidence rate(P=0.918; P=0.581; P=0.366). With ≥0.434 as the diagnostic threshold, the model had the highest diagnostic efficacy (sensitivity: 86.0%, specificity: 56.3%, Youden index: 0.423). In the external validation cohort, there was no significant difference between C-US and CT(P>0.05). Compared with C-US and CT, the sensitivity(66.1% vs 16.1%, P < 0.001; 66.1% vs 9.7%, P < 0.001) and accuracy(68.6% vs 55.4%, P=0.041; 68.6% vs 52.9%, P=0.012) of ATR model were higher, and the negative predictive value was higher than that of CT(66.7% vs 50.9%, P=0.042), but there was no difference between ATR model and C-US(66.7% vs 52.3%, P=0.066); There was no significant difference among the three positive predictive values(70.7% vs 83.3%, P=0.211; 70.7% vs 85.7%, P=0.319; 83.3% vs 85.7%, P=0.713), but the specificity of the model was low (71.2% vs 96.6%, P=0.001; 71.2% vs 98.3%, P < 0.001).Conclusion The predictive model based on ACR TI-RADS grades can predict CLNM of PTC more accurately and sensitively than traditional imaging examination.
-
Key words:
- thyroid neoplasms /
- central lymph node /
- computed tomography
-

-
表 1 ACR TI-RADS评分标准
征象 分值 征象 分值 成分 钙化 囊性 0 彗星尾征或无钙化 0 囊实性 1 大钙化 1 实性 2 环状钙化 2 边缘 微钙化 3 光滑或不确定状 0 回声 分叶或不规则 2 无回声 0 腺外侵犯 3 高回声或等回声 1 形状 低回声 2 高宽比<1 0 极低回声 3 高宽比≥1 3 注:ACR为美国放射学会;TI-RADS为甲状腺影像报告和数据系统。 表 2 建模队列及外部验证队列PTC患者的一般资料和超声特征
建模队列 外部验证队列 CLNM阴性 CLNM阳性 CLNM阴性 CLNM阳性 患者/例 148 171 49 56 结节/枚 162 204 59 62 年龄/岁 47.50[38.00,53.00] 45.00[33.00,53.00] 50.00[37.00,54.00] 47.50[35.75,52.25] 性别/例(%) 女 120(81.1) 120(70.2) 39(79.6) 39(69.6) 男 28(18.9) 51(29.8) 10(20.4) 17(30.4) 多发/例(%) 否 117(72.2) 112(54.9) 48(81.4) 28(45.2) 是 45(27.8) 92(45.1) 11(18.6) 34(54.8) 位置/例(%) 左叶 77(47.5) 88(43.1) 28(47.5) 25(40.3) 右叶 83(51.2) 106(52.0) 30(50.8) 29(46.8) 峡部 2(1.2) 10(4.9) 1(1.7) 8(12.9) 最大径 7.00[5.00,11.00] 10.50[7.00,16.00] 7.00[4.60,10.00] 9.50[6.25,15.00] ACR评分 9.00[7.00,10.00] 10.00[8.00,12.00] 10.00[9.00,11.00] 11.00[10.00,13.00] 超声颈部淋巴结情况/例(%) 阴性 153 (94.4) 155 (76.0) 57 (96.6) 52 (83.9) 阳性 9 (5.6) 49 (24.0) 2 (3.4) 10 (16.1) 表 3 预测PTC伴CLNM的单变量分析、全变量模型及ATR模型OR(95%CI)
单变量分析 P 全变量模型 P ATR模型 P 年龄 0.99(0.97,1.01) 0.211 1.00(0.98,1.03) 0.889 - - 性别 1.9(1.08,3.33) 0.026 2.23(1.16,4.3) 0.016 2.15(1.12,4.12) 0.021 多发 2.23(1.32,3.76) 0.001 2.88(1.57,5.31) < 0.001 2.99(1.63,5.47) < 0.001 位置 左叶 参考指标 - 参考指标 - - - 右叶 1.23(0.75,2.01) 0.412 1.04(0.6,1.8) 0.903 - - 峡部 6.23(0.74,52.22) 0.091 6.77(0.71,64.82) 0.097 - - 最大径 1.09(1.05,1.13) < 0.001 1.09(1.04,1.13) < 0.001 1.08(1.04,1.13) < 0.001 ACR评分 1.25(1.13,1.38) < 0.001 1.31(1.16,1.47) < 0.001 1.31(1.16,1.46) < 0.001 表 4 C-US、CT及ATR模型的诊断效能对比
% 项目 符合率 灵敏度 特异度 阳性预测值 阴性预测值 C-US 55.4 16.1 96.6 83.3 52.3 CT 52.9 9.7 98.3 85.7 50.9 ATR模型 68.6 66.1 71.2 70.7 66.7 χ2a) 0.24 0.64 0.00 0.13 0.04 χ2b) 4.17 25.71 10.32 1.56 3.38 χ2c) 6.35 33.03 14.06 0.99 4.12 Pa) 0.624 0.423 1.000 0.713 0.832 Pb) 0.041 < 0.001 0.001 0.211 0.066 Pc) 0.012 < 0.001 < 0.001 0.319 0.042 注:a)C-US与CT比较;b)C-US与ATR模型比较;c)CT与ATR模型比较。 -
[1] Jiang LH, Yin KX, Wen QL, et al. Predictive Risk-scoring Model For Central Lymph Node Metastasis and Predictors of Recurrence in Papillary Thyroid Carcinoma[J]. Sci Rep, 2020, 10(1): 710. doi: 10.1038/s41598-019-55991-1
[2] Welch HG, Doherty GM. Saving Thyroids-Overtreatment of Small Papillary Cancers[J]. N Engl J Med, 2018, 379(4): 310-312. doi: 10.1056/NEJMp1804426
[3] Xing Z, Qiu Y, Yang Q, et al. Thyroid cancer neck lymph nodes metastasis: Meta-analysis of US and CT diagnosis[J]. Eur J Radiol, 2020, 129: 109103. doi: 10.1016/j.ejrad.2020.109103
[4] Tessler FN, Middleton WD, Grant EG, et al. ACR Thyroid Imaging, Reporting and Data System(TI-RADS): White Paper of the ACR TI-RADS Committee[J]. J Am Coll Radiol, 2017, 14(5): 587-595. doi: 10.1016/j.jacr.2017.01.046
[5] 柯晓丽, 沈浩霖, 吕国荣, 等. 颈部淋巴结超声良恶性风险预测模型的构建及价值[J]. 中国超声医学杂志, 2020, 36(4): 314-317. doi: 10.3969/j.issn.1002-0101.2020.04.008
[6] Kim SK, Woo JW, Park I, et al. Computed Tomography-Detected Central Lymph Node Metastasis in Ultrasonography Node-Negative Papillary Thyroid Carcinoma: Is It Really Significant?[J]. Ann Surg Oncol, 2017, 24(2): 442-449. doi: 10.1245/s10434-016-5552-1
[7] 黄云霞, 周瑾, 刘桐桐, 等. 超声影像组学与传统影像模式对甲状腺乳头状癌颈部中央区淋巴结转移的诊断价值比较[J]. 中华超声影像学杂志, 2019, 28(10): 882-887.
[8] Lu W, Zhong L, Dong D, et al. Radiomic analysis for preoperative prediction of cervical lymph node metastasis in patients with papillary thyroid carcinoma[J]. Eur J Radiol, 2019, 118: 231-238. doi: 10.1016/j.ejrad.2019.07.018
[9] 孙可敏, 何秀丽, 郭玲玲. 甲状腺微小乳头状癌临床及超声特征与中央区淋巴结转移的危险因素[J]. 临床耳鼻咽喉头颈外科杂志, 2021, 35(3): 260-263. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202103016.htm
[10] 邓水平, 李泉水, 陈胜华, 等. 甲状腺微小乳头状癌的超声特征与颈部淋巴结转移相关因素分析[J]. 临床超声医学杂志, 2017, 19(6): 424-426. doi: 10.3969/j.issn.1008-6978.2017.06.025
[11] Feng JW, Qu Z, Qin AC, et al. Significance of multifocality in papillary thyroid carcinoma[J]. Eur J Surg Oncol, 2020, 46(10 Pt A): 1820-1828.
[12] Oh HS, Kwon H, Song E, et al. Tumor Volume Doubling Time in Active Surveillance of Papillary Thyroid Carcinoma[J]. Thyroid, 2019, 29(5): 642-649. doi: 10.1089/thy.2018.0609
[13] 林婉玲, 吕国荣, 李伯义, 等. 甲状腺TI-RADS超声指标与肿瘤生物学行为的关系[J]. 中国超声医学杂志, 2016, 32(10): 871-873. doi: 10.3969/j.issn.1002-0101.2016.10.003
[14] 何学森, 钟晓, 蔡华崧, 等. 基于ACR TI-RADS分类对甲状腺乳头状癌淋巴结转移风险模型的预测[J]. 中山大学学报(医学版), 2018, 39(6): 941-947. https://www.cnki.com.cn/Article/CJFDTOTAL-ZSYK201806022.htm
[15] 杨瑞, 张守鹏, 黄韬, 等. cN0期甲状腺微小乳头状癌淋巴结转移模型的构建和验证以及手术方式探讨[J]. 临床耳鼻咽喉头颈外科杂志, 2021, 35(2): 137-140. http://www.cnki.com.cn/Article/CJFDTotal-LCEH202102011.htm
[16] Yu J, Deng Y, Liu T, et al. Lymph node metastasis prediction of papillary thyroid carcinoma based on transfer learning radiomics[J]. Nat Commun, 2020, 11(1): 4807. doi: 10.1038/s41467-020-18497-3
-




 下载:
下载: