Retrospective analysis of risk factors for head and neck multiple space infection with descending necrotic mediastinitis
-
-
Key words:
- head and neck /
- mediastinitis /
- risk factors
-

-
表 1 DNM构成比差异分析
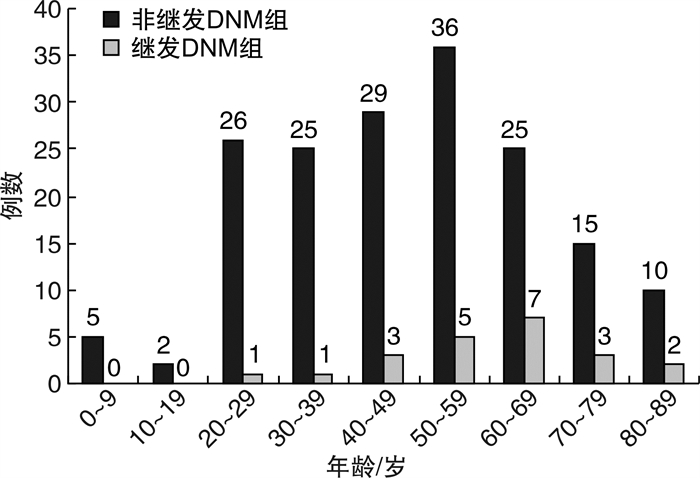
例,x±s 因素 DNM P 否(n=173) 是(n=22) 性别 0.91 男 120 15 女 53 7 年龄/岁 53.91±15.47 66.25±17.83 0.00 心脏病 1.00 是 7 1 否 166 21 肺病 0.45 是 4 1 否 169 21 高血压 1.00 是 24 3 否 149 19 免疫系统疾病 1.00 是 15 2 否 158 20 糖尿病 0.02 是 39 10 否 134 12 表 2 实验室检查结果单因素分析
x±s 项目 非继发DNM组(n=173) 继发DNM组(n=22) P 白细胞计数/ (×109·L-1) 13.59±4.06 13.80±4.17 0.591 中性粒细胞百分比/% 83.10±4.61 85.50±6.08 0.990 空腹血糖/ (mmol·L-1) 9.86±6.36 12.32±6.39 0.041 PCT/ (ng· mL-1) 5.92±2.76 13.08±5.16 < 0.01 CRP/(mg· L-1) 69.19±52.67 186.08±58.18 < 0.01 -
[1] Kimura A, Miyamoto S, Yamashita T. Clinical predictors of descending necrotizing mediastinitis after deep neck infections[J]. Laryngoscope, 2020, 130(11): E567-E572.
[2] 陈国平, 潘忠, 叶飞, 等. 12例颈深部并下行性纵隔感染患者的诊断和治疗[J]. 临床耳鼻咽喉头颈外科杂志, 2021, 35(4): 324-327. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202104009.htm
[3] Razafimanjato N, Ralaizafindraibe TH, Ramarolahy AR, et al. Acute descending necrotizing mediastinitis: four years of experience at a hospital center in Madagascar[J]. Med Sante Trop, 2018, 28(3): 297-301.
[4] Sakai T, Matsutani N, Ito K, et al. Deep cervical and paratracheal drainage for descending necrotizing mediastinitis[J]. Asian Cardiovasc Thorac Ann, 2020, 28(1): 29-32. doi: 10.1177/0218492319896515
[5] 夏韫晖, 曲禄瑶, 梁翔, 等. C反应蛋白在下行性坏死性纵隔炎中的预警作用[J]. 中国口腔颌面外科杂志, 2019, 17(3): 257-260. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGKQ201903022.htm
[6] Scaglione M, Pinto A, Romano S, et al. Determining optimum management of descending necrotizing mediastinitis with CT; experience with 32 cases[J]. Emerg Radiol, 2005, 11(5): 275-280. doi: 10.1007/s10140-005-0422-3
[7] 许雯, 汤玮, 余少卿, 等. 颈部CT、超声与MRI对颈深部脓肿诊断价值的对比研究[J]. 临床耳鼻咽喉头颈外科杂志, 2019, 33(7): 672-674. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201907024.htm
[8] Bartoletti M, Antonelli M, Bruno Blasi FA, et al. Procalcitonin-guided antibiotic therapy: an expert consensus[J]. Clin Chem Lab Med, 2018, 56(8): 1223-1229. doi: 10.1515/cclm-2018-0259
[9] Aloisio E, Dolci A, Panteghini M. Procalcitonin: Between evidence and critical issues[J]. Clin Chim Acta, 2019, 496: 7-12. doi: 10.1016/j.cca.2019.06.010
[10] Schuetz P, Beishuizen A, Broyles M, et al. Procalcitonin(PCT)-guided antibiotic stewardship: an international experts consensus on optimized clinical use[J]. Clin Chem Lab Med, 2019, 57(9): 1308-1318. doi: 10.1515/cclm-2018-1181
[11] Cortegiani A, Misseri G, Ippolito M, et al. Correction to: Procalcitonin levels in candidemia versus bacteremia: a systematic review[J]. Crit Care, 2019, 23(1): 322. doi: 10.1186/s13054-019-2598-z
[12] Watkins EJ, Guerrini J. Procalcitonin-guided treatment of lower respiratory tract infections[J]. JAAPA, 2018, 31(1): 50-52. doi: 10.1097/01.JAA.0000527711.69310.ae
[13] Tujula B, Hämäläinen S, Kokki H, et al. Review of clinical practice guidelines on the use of procalcitonin in infections[J]. Infect Dis(Lond), 2020, 52(4): 227-234. doi: 10.1080/23744235.2019.1704860
[14] Ironson G, Banerjee N, Fitch C, et al. Positive emotional well-being, health Behaviors, and inflammation measured by C-Reactive protein[J]. Soc Sci Med, 2018, 197: 235-243. doi: 10.1016/j.socscimed.2017.06.020
[15] Petel D, Winters N, Gore GC, et al. Use of C-reactive protein to tailor antibiotic use: a systematic review and meta-analysis[J]. BMJ Open, 2018, 8(12): e022133. doi: 10.1136/bmjopen-2018-022133
[16] McFadyen JD, Zeller J, Potempa LA, et al. C-Reactive Protein and Its Structural Isoforms: An Evolutionary Conserved Marker and Central Player in Inflammatory Diseases and Beyond[J]. Subcell Biochem, 2020, 94: 499-520.
[17] Villard MA, Helm MC, Kindel TL, et al. C-Reactive protein as a predictor of post-operative complications in bariatric surgery patients[J]. Surg Endosc, 2019, 33(8): 2479-2484. doi: 10.1007/s00464-018-6534-0
[18] Tsai YW, Liu YH, Su HH. Bacteriology of peritonsillar abscess: the changing trend and predisposing factors[J]. Braz J Otorhinolaryngol, 2018, 84(5): 532-539. doi: 10.1016/j.bjorl.2017.06.007
-




 下载:
下载: