The relationship between vestibular function and gait parameters in vestibular dysfunctional patients with idiopathic sudden sensorineural hearing loss
-
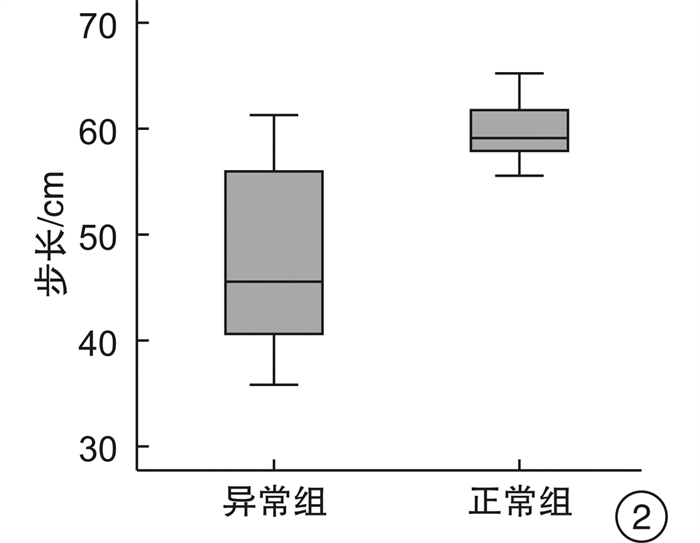
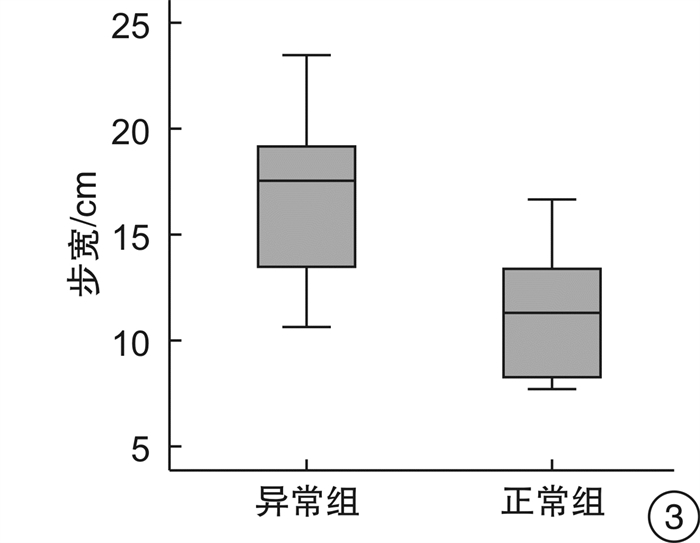
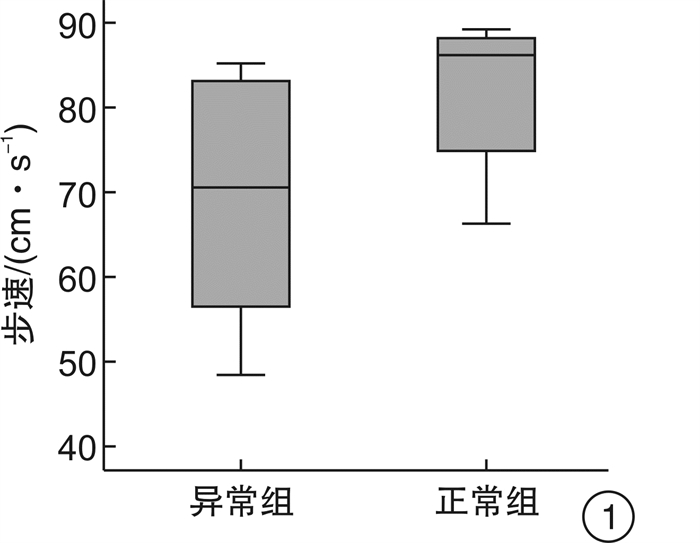
摘要: 目的 本研究以特发性突发性感音神经性聋(ISSNHL)患者为外周前庭功能异常疾病的模型, 在应用视频头脉冲试验(vHIT)、颈性前庭诱发肌源性电位(cVEMP)测试、眼性前庭诱发肌源性电位(oVEMP)测试定位前庭病变部位的基础上, 探讨半规管、球囊和椭圆囊功能对行走平衡的影响。方法 对23例单侧ISSNHL患者(其中14例伴眩晕)进行了纯音测听、步行试验、vHIT试验、cVEMP测试和oVEMP测试。结果 椭圆囊功能与步长显著相关, 球囊功能分别与步速和步宽显著相关。半规管功能和步态参数没有关系。结论 ISSNHL患者耳石器功能受损可能导致步速减缓、步长变短、步宽变宽。Abstract: Objective Based on the application of vHIT, cVEMP test and oVEMP test to locate the peripheral vestibular lesions, we aimed to explore the relationship between vestibular function(semicircular canal and otolith function) and gait parameters in vestibular dysfunctional patients with idiopathic sudden sensorineural hearing loss(ISSNHL).Methods In this study, 23 ISSNHL patients(including 14 patients with vertigo) were enrolled. All patients underwent audiometry, Walk Across, vHIT, cVEMP test and oVEMP test.Results Vestibular otolith function was significantly associated with gait parameters. Semicircular canal function was not associated with any gait parameter.Conclusion Reduced otolith function was associated with slower and wider steps in patients with ISSNHL. These results indicate that vestibular signals may contribute to specific aspects of gait.
-
Key words:
- deafness, sudden /
- vestibular function /
- walking balance
-

-
[1] Bent LR, Inglis JT, McFadyen BJ. When is vestibular information important during walking?[J]. J Neurophysiol, 2004, 92(3): 1269-1275. doi: 10.1152/jn.01260.2003
[2] Liu J, Zhou RH, Liu B, et al. Assessment of balance and vestibular functions in patients with idiopathic sudden sensorineural hearing loss[J]. J Huazhong Univ Sci Technolog Med Sci, 2017, 37(2): 264-270. doi: 10.1007/s11596-017-1726-8
[3] Fujimoto C, Murofushi T, Chihara Y, et al. Effects of unilateral dysfunction of the inferior vestibular nerve system on postural stability[J]. Clin Neurophysiol, 2010, 121(8): 1279-1284. doi: 10.1016/j.clinph.2010.02.149
[4] Kim SC, Kim JY, Lee HN, et al. A quantitative analysis of gait patterns in vestibular neuritis patients using gyroscope sensor and a continuous walking protocol[J]. J Neuroeng Rehabil, 2014, 11: 58. doi: 10.1186/1743-0003-11-58
[5] Angunsri N, Ishikawa K, Yin M, et al. Gait instability caused by vestibular disorders-analysis by tactile sensor[J]. Auris Nasus Larynx, 2011, 38(4): 462-468. doi: 10.1016/j.anl.2011.01.016
[6] Allum JH, Adkin AL. Improvements in trunk sway observed for stance and gait tasks during recovery from an acute unilateral peripheral vestibular deficit[J]. Audiol Neurootol, 2003, 8(5): 286-302. doi: 10.1159/000071999
[7] Agrawal Y, Davalos-Bichara M, Zuniga MG, et al. Head impulse test abnormalities and influence on gait speed and falls in older individuals[J]. Otol Neurotol, 2013, 34(9): 1729-1735. doi: 10.1097/MAO.0b013e318295313c
[8] Chang TP, Schubert MC. Association of the Video Head Impulse Test With Improvement of Dynamic Balance and Fall Risk in Patients With Dizziness[J]. JAMA Otolaryngol Head Neck Surg, 2018, 144(8): 696-703. doi: 10.1001/jamaoto.2018.0650
[9] Allum JH, Honegger F. Relation between head impulse tests, rotating chair tests, and stance and gait posturography after an acute unilateral peripheral vestibular deficit[J]. Otol Neurotol, 2013, 34(6): 980-989. doi: 10.1097/MAO.0b013e31829ce5ec
[10] Stachler RJ, Chandrasekhar SS, Archer SM, et al. American Academy of Otolaryngology-Head and Neck Surgery. Clinical practice guideline: sudden hearing loss[J]. Otolaryngol Head Neck Surg, 2012, 146(3 Suppl): S1-35.
[11] 张青, 胡娟, 许信达, 等. 突发性聋患者前庭耳石器传导通路功能的客观评价[J]. 中华耳鼻咽喉头颈外科杂志, 2013, 48(5): 389-393. doi: 10.3760/cma.j.issn.1673-0860.2013.05.008
[12] Hong SM, Byun JY, Park CH, et al. Saccular damage in patients with idiopathic sudden sensorineural hearing loss without vertigo[J]. Otolaryngol Head Neck Surg, 2008, 139(4): 541-545. doi: 10.1016/j.otohns.2008.07.003
[13] 牛晓蓉, 张青, 韩鹏, 等. 不伴眩晕的突发性感音神经性耳聋患者隐匿的前庭机能障碍研究[J]. 四川大学学报(医学版), 2015, 46(3): 426-430. https://www.cnki.com.cn/Article/CJFDTOTAL-HXYK201503019.htm
[14] 刘东冬, 张甦琳, 刘波, 等. 基于机器学习的前庭康复决策研究[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(7): 21-27. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202007005.htm
[15] Mamoto Y, Yamamoto K, Imai T, et al. Three-dimensional analysis of human locomotion in normal subjects and patients with vestibular deficiency[J]. Acta Otolaryngol, 2002, 122(5): 495-500. doi: 10.1080/00016480260092282
[16] Yamamoto K, Mamoto Y, Imai T, et al. Effects of caloric vestibular stimulation on head and trunk movements during walking[J]. Gait Posture, 2002, 15(3): 274-281. doi: 10.1016/S0966-6362(01)00152-7
[17] Layman AJ, Li C, Simonsick E, et al. Association between saccular function and gait speed: data from the Baltimore Longitudinal Study of Aging[J]. Otol Neurotol, 2015, 36(2): 260-266. doi: 10.1097/MAO.0000000000000544
[18] Grossman GE, Leigh RJ, Abel LA, et al. Frequency and velocity of rotational head perturbations during locomotion[J]. Exp Brain Res, 1988, 70(3): 470-476.
[19] Goldberg JM, Cullen KE. Vestibular control of the head: possible functions of the vestibulocollic reflex[J]. Exp Brain Res, 2011, 210(3/4): 331-345.
[20] Mergner T, Becker W. A modeling approach to the human spatial orientation system[J]. Ann N Y Acad Sci, 2003, 1004: 303-315. doi: 10.1196/annals.1303.028
[21] Basta D, Todt I, Scherer H, et al. Postural control in otolith disorders[J]. Hum Mov Sci, 2005, 24(2): 268-279. doi: 10.1016/j.humov.2005.04.002
[22] Schneider AD, Jamali M, Carriot J, et al. The increased sensitivity of irregular peripheral canal and otolith vestibular afferents optimizes their encoding of natural stimuli[J]. J Neurosci, 2015, 35(14): 5522-5536. doi: 10.1523/JNEUROSCI.3841-14.2015
[23] Zangemeister WH, Bulgheroni MV, Pedotti A. Normal gait is differentially influenced by the otoliths[J]. J Biomed Eng, 1991, 13(6): 451-458. doi: 10.1016/0141-5425(91)90089-P
[24] Valerio S, Taube JS. Head Direction Cell Activity Is Absent in Mice without the Horizontal Semicircular Canals[J]. J Neurosci, 2016, 36(3): 741-754. doi: 10.1523/JNEUROSCI.3790-14.2016
[25] Fitzpatrick RC, Butler JE, Day BL. Resolving head rotation for human bipedalism[J]. Curr Biol, 2006, 16(15): 1509-1514. doi: 10.1016/j.cub.2006.05.063
[26] Black FO, Shupert CL, Peterka RJ, et al. Effects of unilateral loss of vestibular function on the vestibulo-ocular reflex and postural control[J]. Ann Otol Rhinol Laryngol, 1989, 98(11): 884-889. doi: 10.1177/000348948909801109
[27] Han BI, Song HS, Kim JS. Vestibular rehabilitation therapy: review of indications, mechanisms, and key exercises[J]. J Clin Neurol, 2011, 7(4): 184-196. doi: 10.3988/jcn.2011.7.4.184
[28] Halmagyi GM, Weber KP, Curthoys IS. Vestibular function after acute vestibular neuritis[J]. Restor Neurol Neurosci, 2010, 28(1): 37-46.
[29] O′Connor SM, Kuo AD. Direction-dependent control of balance during walking and standing[J]. J Neurophysiol, 2009, 102(3): 1411-1419. doi: 10.1152/jn.00131.2009
[30] Mark AS, Fitzgerald D. Segmental enhancement of the cochlea on contrast-enhanced MR: correlation with the frequency of hearing loss and possible sign of perilymphatic fistula and autoimmune labyrinthitis[J]. AJNR Am J Neuroradiol, 1993, 14(4): 991-996.
[31] Horner KC. Old theme and new reflections: hearing impairment associated with endolymphatic hydrops[J]. Hear Res, 1991, 52(1): 147-156. doi: 10.1016/0378-5955(91)90194-E
[32] Tonndorf J. Endolymphatic hydrops: mechanical causes of hearing loss[J]. Arch Otorhinolaryngol, 1976, 212(4): 293-299. doi: 10.1007/BF00453677
-




 下载:
下载: