-
摘要: 目的 探讨预测鼻腔鼻窦内翻性乳头状瘤(SNIP)恶变的相关危险因素, 提高术前诊断肿瘤恶变的准确性。方法 回顾性分析89例SNIP及内翻性乳头状瘤恶变(IP-SCC)患者的临床资料, 其中SNIP组60例, IP-SCC组29例。选取长期吸烟史和长期感染史、内镜检查所见肿瘤特征、鼻窦CT和MRI示肿瘤特征等多种临床指标, 对两组患者进行比较, 进一步选择两组间有显著性差异的指标进行多因素Logistic回归分析, 通过建立回归模型分析预测SNIP恶变的相关危险因素和模型的预测能力。结果 SNIP组与IP-SCC组患者相关症状(涕中带血)、长期吸烟史, 内镜下见肿瘤附着脓涕, 鼻窦CT示眶壁骨质破坏、颅底骨质破坏, 鼻窦MRI示脑回征、眶内受累、颅底硬脑膜强化等指标差异有统计学意义。进一步行多因素Logistic回归分析, 结果示涕中带血、长期吸烟史、内镜下见肿瘤附着脓涕、CT示眶壁骨质破坏、MRI示脑回征消失、眶内受累6个因素是提示SNIP恶变的危险因素。这一模型对SNIP恶变的预测准确率为75.0%, 对SNIP的预测准确率为96.7%, 模型总体预测准确率为89.8%。结论 预测SNIP恶变的相关危险因素是涕中带血、长期吸烟史、内镜下见肿瘤附着脓涕、CT示眶壁骨质破坏、MRI示脑回征消失、眶内受累6个因素。综合分析临床多项指标可提高术前对SNIP恶变诊断的准确性。Abstract: Objective To explore the risk factors of malignant transformation of sinonasal inverted papilloma (SNIP), and to improve the accuracy of preoperative diagnosis of tumor.Methods The clinical data of 89 patients with sinonasal inverted papilloma (SNIP group, n = 60) and malignant transformation of sinonasal inverted papilloma (IP-SCC, n = 29) were analyzed retrospectively. Clinical symptoms, medical history, endoscopic examination, characteristic of sinonasal CT scan and MR imaging were collected and compared between two groups. Then the indicators with significant differences between the two groups were used for binary logistic regression analysis. The logistic regression model was established to predict the malignant transformation risk factors of inverted papilloma and the prediction ability of the regression model was estimated.Results The significant differences between the two groups were: symptoms, including nasal obstruction, purulent mucus, blood in the nasal discharge; long-term smoking history; tumor attached with purulent mucus; CT scan showing bone destruction of the orbital wall and skull base; MR Imaging showing convoluted cerebriform pattern (CCP) sign, intraorbital involvement, and dural enhancement of the skull base. The results of logistic regression analysis showed that the risk factors of malignant transformation of SNIP were blood in the nasal discharge, long-term smoking history, tumor with purulent discharge, orbital wall destruction on CT scan, disappearance of CCP and orbital involvement on MRI. The accuracy rate of regression model for predicting malignant transformation of IP is 75.0%, and the accuracy rate for benign inverted papilloma is 96.7%, and the overall accuracy of the model is 89.8%.Conclusion The risk factors for predicting malignant transformation of SNIP are blood in the nasal discharge, long-term smoking history, tumor with purulent discharge, orbital wall destruction on CT scan, and disappearance of CCP sign and orbital involvement on MRI. It′s necessary to analyze all of clinical factors in order to improve the accuracy of preoperative diagnosis of sinonasal inverted papilloma.
-
Key words:
- nasal neoplasms /
- inverted papilloma /
- risk factors /
- malignant transformation
-

-
表 1 两组间各项临床特征的比较
指标 SNIP组(n=60) IP-SCC组(n=29) χ2 P 年龄/岁 54 (28~85) 58 (25~88) 677.50a) 0.145 性别 0.002 0.962 男 39 19 女 21 10 症状 鼻塞 39 24 2.982 0.084 脓涕 21 16 3.275 0.070 涕中带血 10 14 9.918 0.002 嗅觉减退 15 9 0.361 0.548 吸烟史 19 16 4.257 0.033 鼻部感染史 30 18 1.146 0.284 既往手术史 16 4 1.860 0.173 内镜检查 息肉样新生物 12 2 2.532 0.112 分叶状新生物 42 11 8.347 0.004 伴脓性分泌物 12 14 7.559 0.006 注a) 为非参数检验Mann-Whitney U检验的统计量U值。 表 2 两组间肿瘤累及部位的比较分析
肿瘤累及部位 SNIP组(n=60) IP-SCC组(n=29) χ2 P 额窦 12 9 1.320 0.251 筛窦 30 13 0.209 0.647 上颌窦 31 15 0 0.996 蝶窦 1 3 3.430 0.064 鼻腔外侧壁 7 5 0.521 0.470 表 3 肿瘤影像学特征的两组间比较分析
SNIP组(n=60) IP-SCC组(n=29) χ2 P 鼻窦CT 鼻腔鼻窦骨质破坏吸收 25 20 5.829 0.016 眶壁骨质破坏 1 5 7.543 0.006 颅底骨质破坏 0 6 13.311 < 0.01 鼻窦骨质增生硬化 37 5 15.483 < 0.01 鼻窦MRI 脑回征 46 6(局部) 25.220 < 0.01 眶内受累 1 5 7.543 0.006 颅底硬膜强化 0 3 6.423 0.05 表 4 内翻性乳头状瘤恶变的多因素回归分析
因素 b S.E Wald χ2 P OR 95%CI 下限 上限 涕中带血 -2.913 1.055 7.628 0.006 0.054 0.007 0.429 吸烟史 -2.040 0.970 4.428 0.035 0.130 0.019 0.869 内镜见脓涕 -3.263 1.076 9.196 0.002 0.038 0.005 0.315 CT示眶壁骨质破坏 -2.803 2.106 4.152 0.042 0.061 0.001 3.764 CT示颅底骨质破坏 -15.459 28 420.737 0.000 0.999 0 0.000 — MRI示眶内组织受累 -2.079 1.752 6.296 0.022 0.125 0.004 3.875 MRI示颅底硬脑膜强化 -3.959 34 338.972 0.000 0.999 0.019 0.000 — MRI脑回征消失 3.790 1.074 12.450 0.001 44.237 5.390 363.062 -
[1] Anari S, Carrie S.Sinonasal inverted papilloma:narrative review[J]. J Laryngol Otol, 2010,124(7):705-15. doi: 10.1017/S0022215110000599
[2] Wang MJ, Noel JE.Etiology of sinonasal inverted papilloma:A narrative review[J]. World J Otorhinolaryngol Head Neck Surg, 2017, 3(1):54-58. doi: 10.1016/j.wjorl.2016.11.004
[3] Zhang L, Fang G, Yu W, et al.Prediction of malignant sinonasal inverted papilloma transformation by preoperative computed tomography and magnetic resonance imaging[J]. Rhinology, 2020, 58(3):248-256.
[4] Thompson L.World Health Organization classification of tumours:pathology and genetics of head and neck tumours[J]. Ear Nose Throat J, 2006, 85(2):74. doi: 10.1177/014556130608500201
[5] Yan CH, Tong C, Penta M, et al.Imaging predictors for malignant transformation of inverted papilloma[J]. Laryngoscope, 2019,129(4):777-782. doi: 10.1002/lary.27582
[6] Re M, Gioacchini FM, Bajraktari A, et al.Malignant transformation of sinonasal inverted papilloma and related genetic alterations:a systematic review[J]. Eur Arch Otorhinolaryngol, 2017,274(8):2991-3000. doi: 10.1007/s00405-017-4571-2
[7] Tong C, Palmer JN.Updates in the cause of sinonasal inverted papilloma and malignant transformation to squamous cell carcinoma[J]. Curr Opin Otolaryngol Head Neck Surg, 2021, 29(1):59-64. doi: 10.1097/MOO.0000000000000692
[8] Uchi R, Jiromaru R, Yasumatsu R, et al.Genomic Sequencing of Cancer-related Genes in Sinonasal Squamous Cell Carcinoma and Coexisting Inverted Papilloma[J]. Anticancer Res, 2021, 41(1):71-79. doi: 10.21873/anticanres.14752
[9] Zhao RW, Guo ZQ, Zhang RX.Human papillomavirus infection and the malignant transformation of sinonasal inverted papilloma:A meta-analysis[J]. J Clin Virol, 2016, 79:36-43. doi: 10.1016/j.jcv.2016.04.001
[10] Sahnane N, Ottini G, Turri-Zanoni M, et al.Comprehensive analysis of HPV infection, EGFR exon 20 mutations and LINE1 hypomethylation as risk factors for malignant transformation of sinonasal-inverted papilloma to squamous cell carcinoma[J]. Int J Cancer, 2019,144(6):1313-1320. doi: 10.1002/ijc.31971
[11] Frasson G, Cesaro S, Cazzador D, et al.High prevalence of human papillomavirus infection in sinonasal inverted papilloma:a single-institution cohort of patients[J]. Int Forum Allergy Rhinol, 2020, 10(5):629-635. doi: 10.1002/alr.22539
[12] Hakim SA, Abd Raboh NM, Shash LS.IMP3 Immunohistochemical Expression in Inverted Papilloma and Inverted Papilloma-Associated Sinonasal Squamous Cell Carcinoma[J]. Anal Cell Pathol(Amst), 2021, 2021:6639834.
[13] Miyazaki T, Haku Y, Yoshizawa A, et al.Clinical features of nasal and sinonasal inverted papilloma associated with malignancy[J]. Auris Nasus Larynx, 2018, 45(5):1014-1019. doi: 10.1016/j.anl.2018.02.009
[14] 黎庆辉, 朱江.鼻腔-鼻窦内翻性乳头状瘤复发与恶变的临床分析[J].临床耳鼻咽喉头颈外科杂志, 2014, 28(11):797-800. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201411014.htm
[15] Kasbekar AV, Swords C, Attlmayr B, et al.Sinonasal papilloma:what influences the decision to request a magnetic resonance imaging scan?[J]. J Laryngol Otol, 2018,132(7):584-590. doi: 10.1017/S0022215118000804
[16] 房高丽, 王成硕.鼻腔鼻窦内翻性乳头状瘤起源部位的影像学研究进展[J].临床耳鼻咽喉头颈外科杂志, 2014, 28(23):1902-1906. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201423033.htm
[17] 王新艳, 陈青华, 王英, 等.多参数MRI鉴别鼻腔鼻窦内翻性乳头状瘤恶变的价值[J].中华放射学杂志, 2017, 51(7):500-504. doi: 10.3760/cma.j.issn.1005-1201.2017.07.005
[18] 梁青壮, 李德志, 徐震纲.鼻腔-鼻窦内翻性乳头状瘤临床及其相关研究进展[J].中国耳鼻咽喉颅底外科杂志, 2015, 21(1):80-84. https://www.cnki.com.cn/Article/CJFDTOTAL-ZEBY201501031.htm
[19] Hong SL, Kim BH, Lee JH, et al.Smoking and malignancy in sinonasal inverted papilloma[J]. Laryngoscope, 2013,123(5):1087-1091. doi: 10.1002/lary.23876
[20] 杨凤娟, 甘卫刚, 刘锋, 等.鼻腔菌群多样性与慢性鼻窦炎伴鼻息肉手术预后相关性分析[J].临床耳鼻咽喉头颈外科杂志, 2020, 34(9):799-804. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202009008.htm
-

| 引用本文: | 王明婕, 侯丽珍, 周兵, 等. 鼻腔鼻窦内翻性乳头状瘤恶变的相关危险因素分析[J]. 临床耳鼻咽喉头颈外科杂志, 2021, 35(7): 627-632. doi: 10.13201/j.issn.2096-7993.2021.07.011 |
| Citation: | WANG Mingjie, HOU Lizhen, ZHOU Bing, et al. Risk factors of malignant transformation of sinonasal inverted papilloma[J]. J Clin Otorhinolaryngol Head Neck Surg, 2021, 35(7): 627-632. doi: 10.13201/j.issn.2096-7993.2021.07.011 |
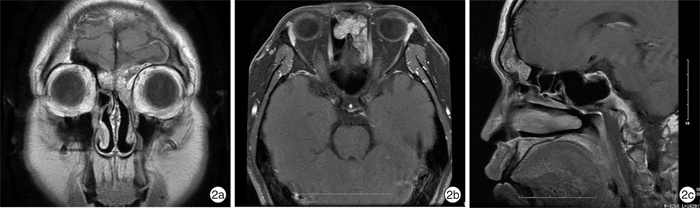
- Figure 1.
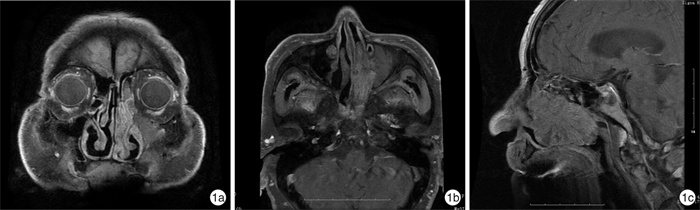
- Figure 2.



 下载:
下载: