Key factors of the severity of chronic subjective tinnitus: a complex network analysis
-
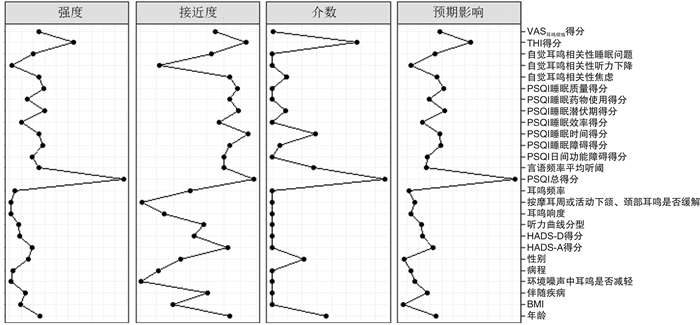
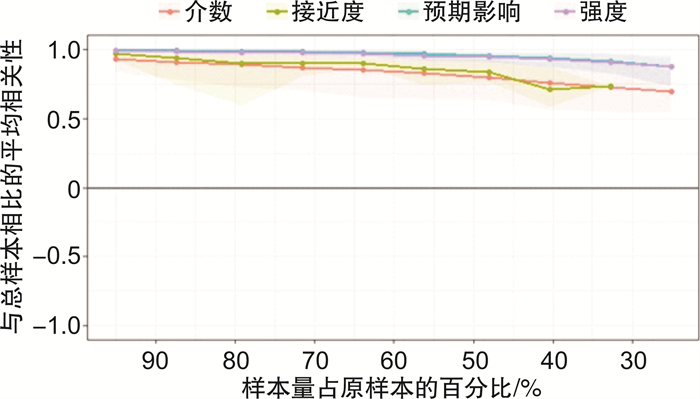
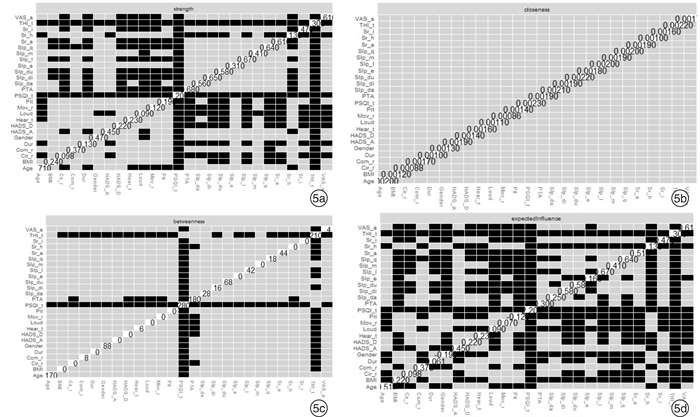
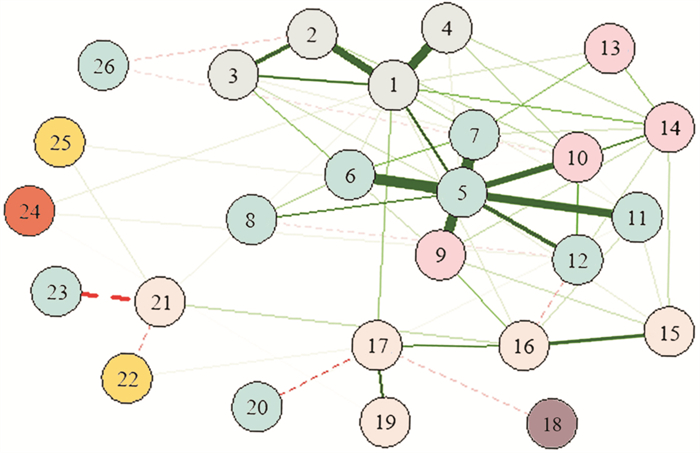
摘要: 目的 通过复杂网络分析探讨影响慢性主观性耳鸣严重程度的关键因素。 方法 回顾性分析2019年12月—2020年10月就诊于北京协和医院耳鼻咽喉头颈外科的慢性主观性耳鸣患者的临床资料, 包括人口学特征、听力学特点及耳鸣相关检查结果, 以患者就诊时填写的中文版耳鸣残障量表(THI)、医院焦虑抑郁量表、匹兹堡睡眠质量指数、耳鸣响度和烦恼程度视觉模拟评分量表得分评估其睡眠及心理声学特征。将以上相关信息作为节点, 利用R语言构建复杂网络模型, 分析以上节点与患者THI得分的相关性。 结果 共183例患者符合入组条件, 其中男99例(54.1%), 女84例(45.9%), 年龄(41.65±1.05)岁。复杂网络分析结果提示THI得分与焦虑、睡眠障碍密切相关, 焦虑较睡眠障碍与THI得分的关系更紧密; 患者自觉耳鸣相关性焦虑与耳鸣相关性睡眠障碍之间有较强的相关性。人口学特征、听力学及耳鸣相关检查与THI得分无明显相关性。 结论 耳鸣严重程度与焦虑和睡眠障碍密切相关, 情绪与睡眠是调控耳鸣的关键因素, 且焦虑的作用更大。睡眠障碍与焦虑存在一定的相关性, 二者可能在调控耳鸣的作用中产生叠加效应, 进一步加重耳鸣的严重程度。未来对于慢性主观性耳鸣的治疗, 应更加关注改善焦虑及睡眠状况以提高疗效。Abstract: Objective To investigate the key factors related to the severity of chronic subjective tinnitus through a complex network analysis. Methods A retrospective study about patients with chronic subjective tinnitus presented to Peking Union Medical College Hospital from December 2019 to October 2020 was conducted. The demographic information, audiometric and tinnitus-related tests, and scores of Tinnitus Handicap Inventory(THI), Hospital Anxiety and Depression Scale(HADS), Pittsburgh Sleep Quality Index(PSQI) and Visual Analogue Scale(VAS) of tinnitus loudness and annoyance were set as nodes in a complex network which was conducted and analyzed through the R package. Results A total of 183 patients were enrolled, including 99(54.1%) males and 84(45.9%) females, with an average age of(41.65±1.05) years. The results of the complex network analysis showed that anxiety and sleep disorder were closely related to THI score, and anxiety was more important than sleep disorder. There was a strong correlation between self-reported anxiety and insomnia. Demographic characteristics, audiologic and tinnitus-associated tests were not significantly related to THI score. Conclusion Anxiety and sleep disturbance were key factors related to tinnitus severity, and anxiety played a more important role. There was an obvious correlation between sleep disorder and anxiety, and they might have a superimposed effect on tinnitus severity. Future therapies of tinnitus should pay more attention on releasing anxiety and insomnia.
-
Key words:
- tinnitus /
- anxiety /
- sleep /
- complex network analysis
-

-
表 1 人口学特征
例(%) 人口学特征 例(%) 人口学特征 例(%) BMI 自觉耳鸣相关性听力下降 ≤24 76(41.5) 否 95(51.9) >24 107(58.5) 是 88(48.1) 耳鸣病程/年 自觉耳鸣相关性焦虑 ≤4 136(74.3) 否 65(35.5) >4 47(25.7) 是 118(64.5) 耳鸣侧别 自觉耳鸣相关性睡眠障碍 左 41(22.4) 否 88(48.1) 右 46(25.1) 是 95(51.9) 双侧 96(52.5) 环境噪声中耳鸣是否缓解 伴随疾病 无变化 96(52.4) 否 139(76.0) 缓解 45(24.6) 是 44(24.0) 加重 42(23.0) 耳相关性疾病 按摩耳周或活动下颌、颈部耳鸣是否缓解 否 156(85.2) 无变化 137(74.8) 是 27(14.8) 缓解 40(21.9) 加重 6(3.3) 表 2 听力检查、耳鸣相关检查、心理声学和睡眠特征
变量 值(n=183) 变量 值(n=183) 听力曲线分型/例(%) HADS 正常 64(35.0) HADS-焦虑/分 7.89±0.22 缓降型 2(1.0) 正常/例(%) 87(47.5) 陡降型 42(23.0) 异常/例(%) 96(52.5) 高频下降型 59(32.2) HADS-抑郁/分 9.50±0.16 上升型 12(6.6) 正常/例(%) 19(10.4) 切迹型 4(2.2) 异常/例(%) 164(89.6) 言语频率平均听阈/dB HL 19.98±1.01 PSQI总分/分 6.84±0.32 耳鸣响度/dB SL 10.50±0.99 正常/例(%) 57(36.6) 最小掩蔽级/dB SL 12.29±1.36 异常/例(%) 116(63.4) 耳鸣频率/例(%) 睡眠质量/分 0.62±0.04 ≤0.5 kHz 20(10.9) 睡眠潜伏期/分 1.52±0.08 1~3 kHz 31(16.9) 睡眠时间/分 0.96±0.08 ≥4 kHz 132(72.2) 睡眠效率/分 1.15±0.10 残余抑制试验/例(%) 睡眠障碍/分 0.87±0.05 无变化或反跳 72(39.3) 睡眠药物使用/分 0.29±0.07 完全或部分缓解 111(60.7) 日间功能障碍/分 0.83±0.06 THI总分/分 41.15±2.21 耳鸣响度VAS/分 4.68±0.19 功能性子量表得分 18.06±1.01 耳鸣烦恼程度VAS/分 4.81±0.21 灾难性子量表得分 9.35±0.48 情感子量表得分 13.73±0.89 -
[1] Payne ME, Porter Starr KN, Orenduff M, et al. Quality of Life and Mental Health in Older Adults with Obesity and Frailty: Associations with a Weight Loss Intervention[J]. J Nutr Health Aging, 2018, 22 (10) : 1259-1265. doi: 10.1007/s12603-018-1127-0
[2] McCormack A, Edmondson-Jones M, Somerset S, et al. Corrigendum to"A systematic review of the sreporting of tinnitus prevalence and severity"[Hear. Res. 337(2016)70-79][J]. Hear Res, 2016, 339: 219. doi: 10.1016/j.heares.2016.08.010
[3] Lee DY, Kim YH. Risk factors of pediatric tinnitus: Systematic review and meta-analysis[J ]. Laryngoscope, 2018, 128(6) : 1462-1468. doi: 10.1002/lary.26924
[4] Basso L, Boecking B, Brueggemann P, et al. Gender Specific Risk Factors and Comorbidities of Bothersome Tinnitus[J]. Front Neurosci, 2020, 14: 706. doi: 10.3389/fnins.2020.00706
[5] Ramage-Morin PL, Banks R, Pineault D, et al. Tinnitusin Canada[J]. Health Rep, 2019, 30(3) : 3-11.
[6] Mathers C, Smith A, Concha M. Global burden of hearing loss in the year 2000[R]. Geneva: WHO, 2000.
[7] Cai Y, Zhou Q, Yang H, et al. Logistic regression analysis of factors influencing the effectiveness of intensive sound masking therapyin patients with tinnitus[J]. BMJ Open, 2017, 7(11) : e018050. doi: 10.1136/bmjopen-2017-018050
[8] Barthel AL, Pinaire MA, Curtiss JE, et al. Anhedonia is central for the association between quality of life, metacognition, sleep, and affective symptoms in generalized anxiety disorder: A complex network analysis [J]. J Affect Disord, 2020, 277: 1013-1021. doi: 10.1016/j.jad.2020.08.077
[9] Epskamp S, Cramer A, Waldorp LJ, et al. qgraph: network visual-izations of relationships in psychometric data[J]. J Stat Softw, 2012, 48(4) : 367-371.
[10] FriedmanJ, Hastie T, Tibshirani R. Sparse inverse covariance estimation with the graphical lasso[J]. Biostatistics, 2008, 9(3) : 432-441. doi: 10.1093/biostatistics/kxm045
[11] Jones PJ, Ma R, McNally RJ. Bridge Centrality: A Network Approach to Understanding Comorbidity [J]. Multivariate Behav Res, 2021, 56(2) : 353-367. doi: 10.1080/00273171.2019.1614898
[12] Opsahl T, Agneessens F, Skvoretz J. Node centrality in weighted networks: Generalizing degree and shortest paths[J]. Social Networks, 2010, 32(3) : 245-251. doi: 10.1016/j.socnet.2010.03.006
[13] Heeren A, Jones PJ, McNally RJ. Mapping network connectivity among symptoms of social anxiety and comorbid depression in people with social anxiety disorder[J]. J Affect Disord, 2018, 228: 75-82. doi: 10.1016/j.jad.2017.12.003
[14] 王灵莉. 复杂网络社团结构稳定性测试模型的仿真分析[J]. 计算机仿真, 2016, 33(6) : 368-371. doi: 10.3969/j.issn.1006-9348.2016.06.082
[15] Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: Atutorial paper[J]. Behav Res Methods, 2018, 50(1) : 195-212. doi: 10.3758/s13428-017-0862-1
[16] Pattyn T, Van Den Eede F, Vanneste S, et al. Tinnitus and anxiety disorders: A review[J]. Hear Res, 2016, 333: 255-265. doi: 10.1016/j.heares.2015.08.014
[17] Karaaslan Ö, Kantekin Y, Hacımusalar Y, et al. Anxiety sensitivities, anxiety and depression levels, and personality traits of patients with chronic subjective tinnitus: a case-control study[J]. IntJ Psychiatry Clin Pract, 2020, 24(3) : 264-269. doi: 10.1080/13651501.2020.1757117
[18] Moon KR, Park S, Jung Y, et al. Effects of Anxiety Sensitivity and Hearing Loss on Tinnitus Symptom Severity[J]. PsychiatryInvestig, 2018, 15(1) : 34-40.
[19] Chen YC, Wang F, Wang J, et al. Resting-State Brain Abnormalities in Chronic Subjective Tinnitus: A Meta-Analysis[J]. Front Hum Neurosci, 2017, 11: 22.
[20] Vanneste S, Plazier M, der Loo Ev, et al. The neural correlates of tinnitus-related distress[J]. Neuroimage, 2010, 52(2) : 470-480. doi: 10.1016/j.neuroimage.2010.04.029
[21] Vanneste S, Joos K, Langguth B, et al. Neuronal correlates of maladaptive coping: an EEG-study in tinnitus patients[J]. PLoS One, 2014, 9(2) : e88253. doi: 10.1371/journal.pone.0088253
[22] Xu Y, YaoJ, Zhang Z, et al. Association between sleep quality and psychiatric disorders in patients with subjective tinnitus in China[J]. Eur Arch Otorhinolaryngol, 2016, 273(10) : 3063-3072. doi: 10.1007/s00405-016-3906-8
[23] Jakes SC, Hallam RS, Chambers C, et al. A factor analytical study of tinnitus complaint behaviour[J]. Audiology, 1985, 24(3) : 195-206. doi: 10.3109/00206098509070103
[24] Lu T, Li S, Ma Y, et al. Positive Correlation between Tinnitus Severity and Poor Sleep Quality Prior to Tinnitus Onset: a Retrospective Study[J]. Psychiatr Q, 2020, 91(2) : 379-388. doi: 10.1007/s11126-019-09708-2
[25] Asplund R. Sleepiness and sleep in elderly persons with tinnitus[J]. Arch Gerontol Geriatr, 2003, 37(2) : 139-145. doi: 10.1016/S0167-4943(03)00028-1
[26] Hébert S, Fullum S, Carrier J. Polysomnographic and quantitative electroencephalographic correlates of subjective sleep complaints in chronic tinnitus[J]. J Sleep Res, 2011, 20(1 Pt1) : 38-44.
[27] Nofzinger EA, Buysse DJ, Germain A, et al. Functional neuroimaging evidence for hyperarousal in sinsomnia [J]. Am J Psychiatry, 2004, 161(11) : 2126-2128. doi: 10.1176/appi.ajp.161.11.2126
[28] Altena E, Van Der Werf YD, Sanz-Arigita EJ, et al. Prefrontal hypoactivation and recovery in insomnia [J]. Sleep, 2008, 31(9) : 1271-1276.
[29] Wallhäusser-Franke E, Schredl M, Delb W. Tinnitus and insomnia: is hyperarousal the common denominator?[J]. Sleep Med Rev, 2013, 17(1) : 65-74. doi: 10.1016/j.smrv.2012.04.003
[30] Kalmbach DA, Cuamatzi-Castelan AS, Tonnu CV, et al. Hyperarousal and sleep reactivity in insomnia: current insights[J]. Nat Sci Sleep, 2018, 10: 193-201. doi: 10.2147/NSS.S138823
[31] Stobik C, Weber RK, Münte TF, et al. Evidence of psychosomatic influences in compensated and decompensated tinnitus[J]. IntJ Audiol, 2005, 44(6) : 370-378. doi: 10.1080/14992020500147557
[32] Wallhäusser-Franke E, Brade J, Balkenhol T, et al. Tinnitus: distinguishing between subjectively perceived loudness and tinnitus-related distress[J]. PLoS One, 2012, 7(4) : e34583. doi: 10.1371/journal.pone.0034583
[33] Richter K, Zimni M, Tomova I, et al. Insomnia Associated with Tinnitus and Gender Differences[J]. Int J Environ Res Public Health, 2021, 18(6) : 3209. doi: 10.3390/ijerph18063209
[34] Koo M, Hwang JH. Risk of tinnitus in patients with sleepapnea: A nationwide, population-based, case-control study[J ]. Laryngoscope, 2017, 127 (9) : 2171- 2175. doi: 10.1002/lary.26323
[35] 洪志军, 刘秀丽, 刘启贵. 1596名体检者耳鸣状况调查分析[J]. 临床耳鼻咽喉头颈外科杂志, 2016, 30 (19) : 1525-1528. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201619006.htm
[36] 刘博, 李谨, 张祎, 等. 糖尿病患者的耳鸣调查与分析[J]. 临床耳鼻咽喉头颈外科杂志, 2018, 32 (8) : 566- 569. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201808002.htm
-




 下载:
下载: