-
摘要: 目的 分析咽旁间隙肿瘤的影像学特点,并指导治疗方式的选择。方法 回顾性分析75例咽旁间隙肿瘤患者的临床资料。所有患者均行增强CT和(或)增强MRI检查,与血管关系密切或脉管性肿瘤行CTA或MRA检查,与周围神经关系密切肿瘤行MRN检查。评估肿瘤与颈动脉鞘、腮腺、颅底、硬腭的关系,根据肿瘤的影像学特点选择治疗方式。结果 影像学提示良性肿瘤69例,恶性肿瘤6例。8例良性肿瘤选择随访,61例良性肿瘤和6例恶性肿瘤患者进行手术。其中,鼻内镜辅助下经口径路17例,肿瘤位于颈动脉鞘内侧,主体凸向口咽,位于硬腭平面以下,距颅底≥5 mm;经颈径路31例,肿瘤主体凸向颈部(颈动脉鞘外侧15例、内侧16例);经腮腺径路16例,肿瘤与腮腺广基附着;其他径路3例(经鼻径路1例,经鼻和颈联合径路1例,耳颈径路1例)。25例患者出现术后并发症,其中面瘫9例(Ⅱ级6例,Ⅲ级2例,Ⅳ级1例),面部麻木1例,Hornor综合征5例,伸舌偏斜3例,饮水呛咳2例,术后血肿形成1例,口内渗血1例,听力丧失1例,耸肩、抬手无力1例,涎瘘1例,术后口咽部肿胀行气管切开1例,吞咽梗阻1例,味觉出汗综合征1例,因血栓脱落出现急性脑梗死1例。结论 影像学检查结果是咽旁间隙肿瘤治疗方式选择的重要依据。手术径路选择应充分依赖影像学,包括与颈部大血管、腮腺、硬腭的关系,以及距颅底的距离,并结合肿瘤性质。Abstract: Objective To analyze the imaging features of parapharyngeal space tumors, and to guide the choice of treatment.Method A retrospective analysis of 75 cases' clinical data of parapharyngeal space tumor was carried out. All patients underwent enhanced CT and/or enhanced MRI, those tumors closely related to blood vessels and vascular tumors were examined by CTA or MRA, those closely related to peripheral nerves were examined by MRN. We evaluated the relationship between tumor and carotid sheath, parotid gland, skull base and hard palate. We choose the treatment according to the imaging features.Result Imaging revealed 69 benign tumors and 6 malignant tumors. 8 benign tumors chose to follow up, 61 benign tumors and 6 malignant tumors underwent surgery. Among them, 17 cases of tumors were operated by the transoral approach assisted by endoscope, which were located in the medial of carotid sheath, with the main body protruding toward the oropharynx, below the level of the hard palate, and more than 5 mm away from the skull base; 31 cases were resected by the transcervical approach, and the tumor body protruded toward the neck(15 cases were lateral of the carotid sheath, and 16 cases were medial); 16 cases were resected by the transparotid approach, and the tumor harbored a broad interconnecting margin with the parotid gland; there were 3 cases of other approaches(1 case of transnasal approach, 1 case of combined transnasal and transcervical approach, and 1 case of combined transauricular-cervical approach). Postoperative complications occurred in 25 patients, including 9 cases of facial paralysis(6 cases of grade Ⅱ, 2 cases of grade Ⅲ, 1 case of grade Ⅳ), 1 case of facial numbness, 5 cases of Hornor's syndrome; tongue extension deflection in 3 cases, 2 cases cough while drinking water, 1 case of postoperative hematoma formation, 1 case of oral errhysis, hearing loss in 1 case, shoulder shrugging and hand lifting weakness in 1 case, salivary fistula in 1 case, tracheotomy was performed in 1 case because of postoperative oropharyngeal swelling, swallowing obstruction in 1 case, gustatory sweating syndrome in 1 case and acute cerebral infarction was caused by thrombus detachment in 1 case.Conclusion Imaging results are important basis for the treatment of parapharyngeal space tumors. The choice of surgical approach should be made based on imaging, including the relationship with the big vessels of the neck, the parotid gland, the hard palate, and the distance from the skull base, combined with the nature of the tumor.
-
Key words:
- parapharyngeal space tumor /
- imaging /
- surgical approach
-

-
表 1 咽旁间隙肿瘤影像学特点与手术径路
手术径路 颈内动脉 距离颅底距离≥5 mm 与硬腭关系 与腮腺关系 外侧 内侧 是 否 上 下 窄蒂/无关 广基 经口 1 16 17 0 2 15 17 0 经颈 15 16 21 10 7 24 31 0 经腮腺 13 3 14 2 6 10 0 16 其他 1 2 2 1 3 0 3 0 合计 30 37 54 13 18 49 51 16 表 2 经口径路与经颈径路围手术期比较
观察指标 手术径路经口 经颈 P 切口深度/mm 3.93±2.13 19.00±10.25 < 0.05 手术时间/min 154.00±65.43 135.77±57.86 >0.05 术中出血量/mL 76.92±68.36 50.00(120) >0.05 恢复时间/d 7.33±2.69 8.00(3) >0.05 并发症/例(%) 2(11.76) 13(41.94) < 0.05 -
[1] Casani AP, Cerchiai N, Dallan I, et al. Benign tumours affecting the deep lobe of the parotidgland: how to select the optimal surgical approach[J]. Acta Otorhinolaryngol Ital, 2015, 35(2): 80-87.
[2] Kuet ML, Kasbekar AV, Masterson L, et al. Management of tumors arising from the parapharyngeal space: a systematic review of 1, 293 cases reported over 25 years[J]. Laryngoscope, 2015, 125(6): 1372-1381. doi: 10.1002/lary.25077
[3] Dan P, Eran A. Imaging of the parapharyngeal space[J]. Oper Tech Otolayngol Head Neck Surg, 2014, 25(3): 220-226. doi: 10.1016/j.otot.2014.04.002
[4] Stambuk HE, Patel SG. Imaging of the parapharyngeal space[J]. Otolaryngol Clin North Am, 2008, 41(1): 77-101. doi: 10.1016/j.otc.2007.10.012
[5] 丁忠祥, 袁建华, 沈君, 等. 咽旁间隙在头颈部肿瘤MRI诊断中的价值. [J]. 实用放射学杂志, 2007, 23(4): 455-457. doi: 10.3969/j.issn.1002-1671.2007.04.007
[6] Gupta A, Chazen JL, Phillips CD. Imaging evaluation of the parapharyngeal space[J]. Otolaryngol Clin North Am, 2012, 45(6): 1223-1232. doi: 10.1016/j.otc.2012.08.002
[7] Bradley PJ, Bradley PT, Olsen KD. Update on the management of parapharyngeal tumours[J]. Curr Opin Otolaryngol Head Neck Surg, 2010, 19(2): 92-98.
[8] Isobe K, Shimizu T, Akahane T, et al. Imaging of ancient schwannoma[J]. AJR Am J Roentgenol, 2004, 183(2): 331-336. doi: 10.2214/ajr.183.2.1830331
[9] 李平栋, 陈晓红, 房居高, 等. 改良颈-腮腺入路高位咽旁间隙肿瘤切除术探讨[J]. 中国耳鼻咽喉头颈外科, 2013, 20(7): 337-340. https://www.cnki.com.cn/Article/CJFDTOTAL-EBYT201307001.htm
[10] Horowitz G, Ben-Ari O, Wasserzug O, et al. The transcervical approach for parapharyngeal space pleomorphic adenomas: indications and technique[J]. PLoS One, 2014, 9(2): e90210. doi: 10.1371/journal.pone.0090210
-

| 引用本文: | 侯佳欣, 王玲, 曾泉, 等. 咽旁间隙肿瘤影像学与治疗方式选择[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(10): 937-941. doi: 10.13201/j.issn.2096-7993.2020.10.016 |
| Citation: | HOU Jiaxin, WANG Ling, ZENG Quan, et al. Imaging of the parapharyngeal space tumors and selection of the treatment[J]. J Clin Otorhinolaryngol Head Neck Surg, 2020, 34(10): 937-941. doi: 10.13201/j.issn.2096-7993.2020.10.016 |
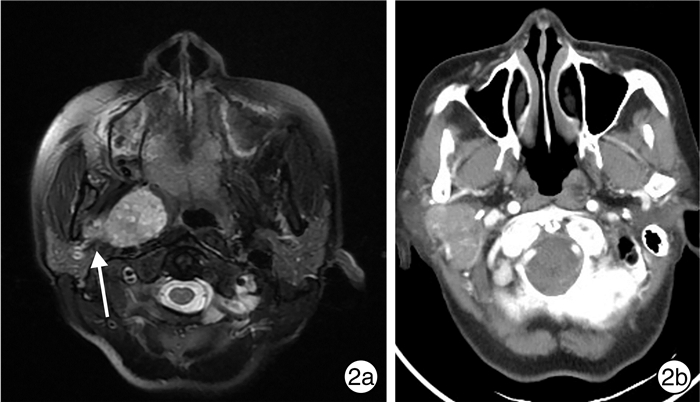
- Figure 1.
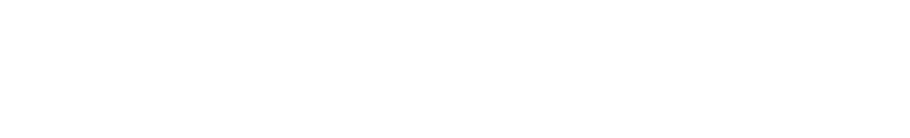
- Figure 2.


 下载:
下载: