The experimental study on the biological rhythm expression of substance P in allergic airway inflammation mice
-
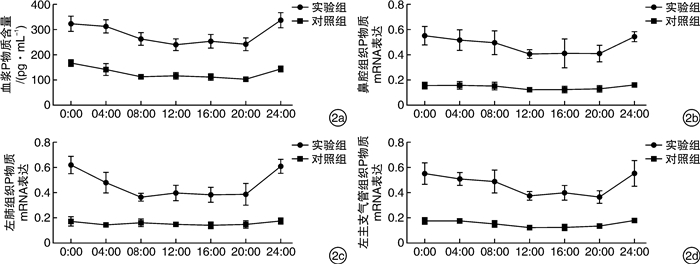
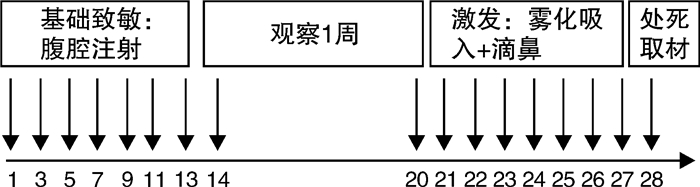
摘要: 目的 建立变应性气道炎症小鼠模型,探讨P物质在变应性气道炎症小鼠中的生物节律性表达。方法 将84只BABL/c小鼠随机分为14个组,分别为实验组7组(0:00组,04:00组,08:00组,12:00组,16:00组,20:00组,24:00组)和对照组7组(0:00组,04:00组,08:00组,12:00组,16:00组,20:00组,24:00组),每组6只。采用卵清蛋白腹腔注射+鼻腔局部激发+雾化吸入的方法制备小鼠变应性气道炎症模型。对实验动物血液进行ELISA法测量上清液P物质含量,采用RT-PCR技术检测不同时间段内P物质在鼻腔组织、肺组织及支气管组织中基因表达的分布及含量。取小鼠鼻腔组织、左肺组织及左主支气管组织行免疫组织化学染色,观察组织切片中P物质阳性细胞的表达及分布。结果 实验组各时间段内血浆中P物质含量明显高于对照组(P < 0.05),其中,实验组中0:00组(321.99±28.93) pg/mL、04:00组(310.76±25.31) pg/mL及24:00组(335.62±28.29) pg/mL的P物质含量明显高于实验组其他时间段(P < 0.05)。实验组小鼠鼻腔组织、左肺组织及左主支气管组织中P物质mRNA表达明显高于对应的对照组(P < 0.01)。实验组小鼠鼻腔组织、左肺及左主支气管免疫组织化学切片中P物质表达显著高于对照组。结论 P物质在变应性气道炎症小鼠模型中呈现高表达,且在凌晨及上午04:00~08:00表达出现峰值,这可能为治疗变应性气道炎症的给药时间提供新的依据。Abstract: Objective To establish the murine models of allergic airway inflammation, and to investigate the biological rhythm expression of substance P in it.Method Eighty-four BALB/c mice were divided into 14 groups, which were airway inflammation groups(0: 00 group, 04: 00 group, 08: 00 group, 12: 00 group, 16: 00 group, 20: 00 group, 24: 00 group) and normal control groups(0: 00 group, 04: 00 group, 08: 00 group, 12: 00 group, 16: 00 group, 20: 00 group, 24: 00 group). The allergic airway inflammation models of mice were established by intraperitoneal injection of ovalbumin(OVA), nasal challenge and aerosol inhalation with OVA. The plasma substance P levels were measured by ELISA. The expression of substance P in nasal mucosa, left lung tissue and left bronchial tissue during different time periods was obversed with RT-PCR and immunohistochemical technique.Result In allergic airway inflammation groups, the plasma substance P levels were higher than in normal control groups(P < 0.05), and 0: 00 group(321.99±28.93) pg/mL, 04: 00 group(310.76±25.31) pg/mL and 24: 00 group(335.62±28.29) pg/mL were higher than other experimental groups(P < 0.05). The expression of substance P mRNA in nasal mucosa, left lung tissue and left bronchial tissue was higher than control groups(P < 0.01). By observing immunohistochemical sections, the expression of substance P in allergic airway inflammation groups was higer than control groups.Conclusion The expression of substance P is high in allergic airway inflammation mice and the peaks are during 04: 00-08: 00 in the early morning, which may provide new basis for treating allergic airway inflammation.
-
Key words:
- allergic airway inflammation /
- substance P /
- biological rhythm
-

-
表 1 各时间点小鼠血浆P物质含量
pg/mL,x±s 时间点 只数 实验组 对照组 t P 0:00 6 321.99±28.931)2) 166.25±11.91 12.19 < 0.01 04:00 6 310.76±25.311)2) 140.33±22.74 12.27 < 0.01 08:00 6 261.17±25.281) 111.14±8.42 13.79 < 0.01 12:00 6 238.76±23.911) 114.86±12.57 11.24 < 0.01 16:00 6 251.19±26.831) 109.33±9.42 12.22 < 0.01 20:00 6 240.91±25.911) 101.30±7.37 12.69 < 0.01 24:00 6 335.62±28.291)2) 141.04±9.40 15.99 < 0.01 与对照组比较,1)P < 0.01;与08:00、12:00、16:00、20:00比较,2)P < 0.05。 表 2 各时间点小鼠鼻腔组织中P物质mRNA表达
时间点 只数 实验组 对照组 t P 0:00 6 0.553±0.073 0.160±0.021 12.718 < 0.01 04:00 6 0.519±0.082 0.164±0.029 9.964 < 0.01 08:00 6 0.498±0.094 0.158±0.029 8.495 < 0.01 12:00 6 0.410±0.033 0.128±0.019 18.347 < 0.01 16:00 6 0.414±0.113 0.129±0.026 6.023 < 0.01 20:00 6 0.413±0.063 0.134±0.029 9.782 < 0.01 24:00 6 0.544±0.038 0.165±0.015 22.877 < 0.01 表 3 各时间点小鼠左肺组织中P物质mRNA表达
时间点 只数 实验组 对照组 t P 0:00 6 0.618±0.067 0.170±0.038 14.254 < 0.01 04:00 6 0.479±0.085 0.140±0.018 9.603 < 0.01 08:00 6 0.363±0.312 0.157±0.026 12.193 < 0.01 12:00 6 0.395±0.064 0.146±0.018 9.149 < 0.01 16:00 6 0.382±0.061 0.138±0.021 9.241 < 0.01 20:00 6 0.388±0.088 0.146±0.030 6.344 < 0.01 24:00 6 0.611±0.056 0.171±0.021 18.122 < 0.01 表 4 各时间点小鼠左主支气管组织中P物质mRNA表达
时间点 只数 实验组 对照组 t P 0:00 6 0.553±0.085 0.176±0.020 10.552 < 0.01 04:00 6 0.509±0.050 0.178±0.011 15.736 < 0.01 08:00 6 0.488±0.091 0.152±0.021 8.834 < 0.01 12:00 6 0.374±0.036 0.125±0.006 16.953 < 0.01 16:00 6 0.395±0.059 0.124±0.017 10.903 < 0.01 20:00 6 0.366±0.049 0.134±0.008 11.541 < 0.01 24:00 6 0.552±0.102 0.178±0.015 8.883 < 0.01 -
[1] Grossman J. One airway, one disease[J]. Chest, 1997, 111(2 Suppl): 11S-16S.
[2] Schäper C, Gustavus B, Koch B, et al. Effect of fluticasone on neuropeptides in nasal lavage in persistent allergic rhinitis[J]. J Investig Allergol Clin Immunol, 2010, 20(3): 214-221. doi: 10.1016/j.jaci.2009.10.034
[3] Man K, Loudon A, Chawla A. Immunity around the clock[J]. Science, 2016, 354(6315): 999-1003. doi: 10.1126/science.aah4966
[4] Scheiermann C, Gibbs J, Ince L, et al. Clocking in to immunity[J]. Nat Rev Immunol, 2018, 18(7): 423-437. doi: 10.1038/s41577-018-0008-4
[5] Kitahata Y, Nunomura S, Terui T, et al. Prolonged culture of mast cells with high-glucose medium enhances the Fc epsilon RI-mediated degranulation response and leukotriene C4 production[J]. Int Arch Allergy Immunol, 2010, 152 Suppl 1: 22-31. doi: 10.1159/000312122
[6] Smolensky MH, Lemmer B, Reinberg AE. Chronobiology and chronotherapy of allergic rhinitis and bronchial asthma[J]. Adv Drug Deliv Rev, 2007, 59(9-10): 852-882. doi: 10.1016/j.addr.2007.08.016
[7] Wang X, Reece SP, Van Scott MR, et al. A circadian clock in murine bone marrow-derived mast cells modulates IgE-dependent activation in vitro[J]. Brain Behav Immun, 2011, 25(1): 127-134. doi: 10.1016/j.bbi.2010.09.007
[8] Sun YQ, Deng MX, He J, et al. Human pluripotent stem cell-derived mesenchymal stem cells prevent allergic airway inflammation in mice[J]. Stem Cells, 2012, 30(12): 2692-2699. doi: 10.1002/stem.1241
[9] 杨瑞嘉, 黄志纯. 变应性鼻炎动物模型的建立与评价[J]. 国际耳鼻咽喉头颈头颈外科杂志, 2007, 31(2): 87-89. https://www.cnki.com.cn/Article/CJFDTOTAL-SCGP201601003.htm
[10] 江满杰, 李泽卿, 吴晋蓉, 等. 变应性鼻炎豚鼠模型上下气道炎症一致性研究[J]. 中国耳鼻咽喉头颈外科, 2012, 19(10): 559-563. https://www.cnki.com.cn/Article/CJFDTOTAL-EBYT201210014.htm
[11] 徐定远, 张勇, 薛飞, 等. 变应性气道炎症动物模型的实验取材[J]. 医学研究生学报, 2009, 22(11): 1147-1149. doi: 10.3969/j.issn.1008-8199.2009.11.008
[12] 丁建明. 光照对哺乳类动物生物钟的调节机制[J]. 基础医学与临床, 2005, 25(7): 577-586. doi: 10.3969/j.issn.1001-6325.2005.07.001
[13] Nicholson PA, Bogie W. Diurnal variation in the symptoms of hay fever: implications for pharmaceutical development[J]. Curr Med Res Opin, 1973, 1(7): 395-400. doi: 10.1185/03007997309111700
[14] Pavlov VA, Tracey KJ. Neural regulation of immunity: molecular mechanisms and clinical translation[J]. Nat Neurosci, 2017, 20(2): 156-166. doi: 10.1038/nn.4477
[15] Gaber T, Strehl C, Buttgereit F. Metabolic regulation of inflammation[J]. Nat Rev Rheumatol, 2017, 13(5): 267-279.
[16] Nakao A. Clockwork allergy: How the circadian clock underpins allergic reactions[J]. J Allergy Clin Immunol, 2018, 142(4): 1021-1031. doi: 10.1016/j.jaci.2018.08.007
[17] Baumann A, Feilhauer K, Bischoff SC, et al. IgE-dependent activation of human mast cells and fMLP-mediated activation of human eosinophils is controlled by the circadian clock[J]. Mol Immunol, 2015, 64(1): 76-81. doi: 10.1016/j.molimm.2014.10.026
[18] Storms WW. Pharmacologic approaches to daytime and nighttime symptoms of allergic rhinitis[J]. J Allergy Clin Immunol, 2004, 114(5 Suppl): S146-153.
[19] 赵小寅, 樊蓥, 金芳, 等. 不同时辰给药对哮喘豚鼠血浆内皮素的影响[J]. 南京中医药大学学报(自然科学版), 2001, 17(2): 102-103. https://www.cnki.com.cn/Article/CJFDTOTAL-NJZY200102014.htm
-




 下载:
下载: