A prospective comparative study on the short-term effect of endoscopic myringoplasty in dry and wet ears
-
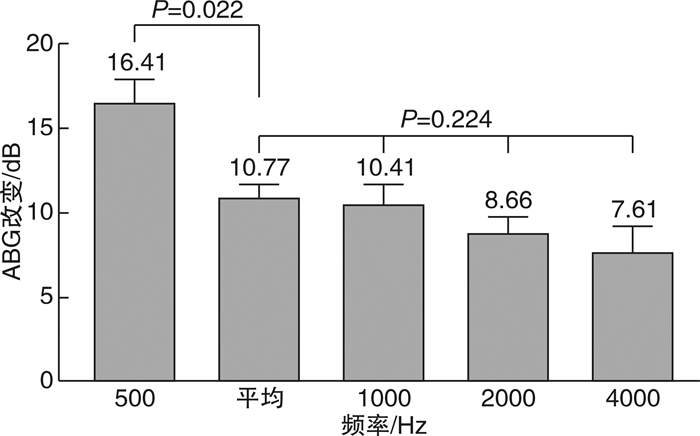
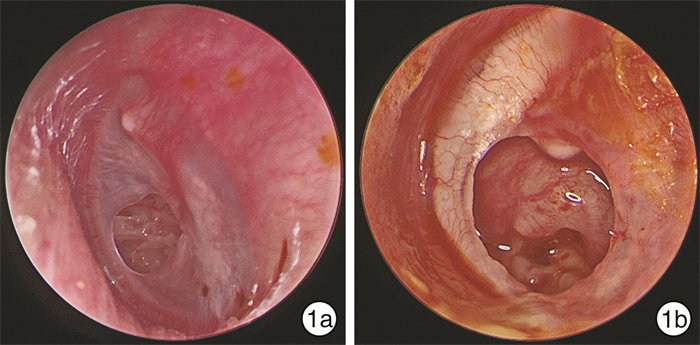
摘要: 目的 探讨干、湿耳条件下, 慢性化脓性中耳炎患者鼓膜修补术后穿孔愈合率、干耳时间及听力改善情况。方法 前瞻性纳入2018-01-2019-10于四川大学华西医院耳鼻咽喉头颈外科经耳内镜行Ⅰ型鼓室成形术的慢性化脓性中耳炎患者。术前完善耳部高分辨薄层CT扫描、耳内镜及纯音听阈测试等检查, 并根据是否有中耳黏、脓性分泌物及鼓室黏膜水肿分为湿耳组(32例)和干耳组(69例)。术后半个月、1个月及3个月随访行耳内镜检查及纯音听阈测试。利用SPSS 19.0统计软件分析鼓膜修补术对不同条件下的慢性化脓性中耳炎和鼓膜穿孔患者的治疗效果。结果 干耳组术后3个月穿孔愈合率为97.1%, 高于湿耳组(90.6%), 但两组差异无统计学意义(P=0.367)。干、湿耳组术后3个月内干耳率分别为98.6%、93.7%, 其中干耳组术后半个月、1个月及3个月干耳率分别为14.5%、52.2%、31.9%, 湿耳组分别为28.1%、40.6%、25.0%。两组患者术后达到干耳的时间无明显差异(P=0.172)。干、湿耳组术后3个月较术前气骨导差(ABG)改变分别为(9.87±1.08) dB、(12.74±1.77) dB, 两组差异无统计学意义(P=0.154)。对纳入干、湿耳患者进行整体分析, 发现术后3个月较术后1个月ABG(P < 0.01)、术后1个月较术前ABG(P < 0.01)明显减小。气导听阈由术前(42.09±1.74) dB HL改善至术后3个月的(29.41±1.61) dB HL(P < 0.01), 而术后3个月骨导听阈较术前无明显变化(P=0.338)。结论 鼓膜修补术在慢性化脓性中耳炎的干耳及湿耳状态下术后疗效无明显差异。湿耳直接行Ⅰ型鼓室成形术对预后没有显著影响。Abstract: Objective To investigate the success rate, dry ear time and hearing improvement of myringoplasty on chronic suppurative otitis media(CSOM) patients under dry and wet ear conditions.Method Patients with CSOM who underwent endoscopic type Ⅰ tympanoplasty between January 2018 and October 2019 in West China Hospital were prospectively enrolled. Before the operation, Ear HRCT, oto-endoscope and pure tone audiometry were completed. According to whether there was mucus and purulent secretion of middle ear accompanied with edema of tympanic mucosa, patients were divided into wet ear group(32 cases) and dry ear group(69 cases). All patients were followed up at half-month, 1 month and 3 months after surgery, with assessment of endoscopy and pure tone audiometry. SPSS 19.0 was used to compare the therapeutic effect of myringoplasty on different condition CSOM patients.Result Compared with wet ear group, a higher level of perforation healing rate was found in dry ear group, but there was no significant difference between them(97.1% vs. 90.6%, P=0.367). The rate of dry ear was 98.6% and 93.7% in dry ear group and wet ear group respectively within three months after surgery, among which the rate of dry ear was 14.5%, 52.2% and 31.9% in dry ear group in half month, 1 month and 3 months after surgery, while that in wet ear group was 28.1%, 40.6% and 25.0% respectively. There was no significant difference in the time to dry ear after surgery between the two groups(P=0.172). Meanwhile, changes of air bone gap(ABG) between pre-operation and 3 months after operation in dry and wet ear groups was similar [(9.87±1.08) dB vs. (12.74±1.77) dB, P=0.154]. When included patients were analyzed as a whole, the ABG at 3 months was significantly lower than 1 month after operation(P < 0.01), similar result was also found when compared the ABG at 1 month after operation with pre-operation(P < 0.01). The air conduction threshold was improved from (42.09±1.74) dB HL before operation to (29.41±1.61) dB HL at 3 months after operation(P < 0.01), however, there was no significant change in bone conduction threshold(P=0.338).Conclusion There is no significant difference in the therapeutic effect of myringoplasty on CSOM patients under dry and wet ear conditions. Direct type Ⅰ tympanoplasty on wet ear patients has no adverse effect on the prognosis.
-
Key words:
- otitis media, suppurative /
- dry ear /
- wet ear /
- myringoplasty /
- treatment effectiveness
-

-
表 1 干耳组和湿耳组患者的临床资料
例(%) 变量 干耳组 湿耳组 P CT软组织影分布a) 0.465 无 23(41.8) 6(25.0) 鼓室 6(10.9) 5(20.8) 乳突 13(23.6) 7(29.2) 鼓室及乳突 13(23.6) 6(25.0) 乳突气化a) 1.000 良好 36(65.5) 15(62.5) 不良 19(34.5) 9(37.5) 鼓膜穿孔部位 0.304 次全 17(24.6) 8(25.0) 后方 5(7.2) 3(9.4) 前下 42(60.9) 15(46.9) 下部 5(7.2) 6(18.8) 鼓膜穿孔大小/mm 0.108 >6 34(49.3) 17(53.1) 3~6 23(33.3) 5(15.6) < 3 12(17.4) 10(31.2) 注:a)22例患者无术前耳部HRCT检查资料,其中干耳组14例,湿耳组8例。 表 2 干耳组和湿耳组患者术后听力改善情况
dB,x±s 变量 干耳组 湿耳组 P值 ABG 术前 22.18±1.16 25.53±1.72 0.107 术后1个月 16.01±0.86 18.60±1.15 0.094 术后3个月 12.09±0.69 13.06±1.21 0.459 术后3个月较术
前ABG改变平均 9.87±1.08 12.74±1.77 0.154 500 Hz 14.52±1.94 20.52±2.25 0.067 1000 Hz 9.29±1.60 12.86±2.16 0.202 2000 Hz 8.05±1.27 10.00±2.25 0.421 4000 Hz 7.62±1.80 7.59±2.79 0.992 -
[1] Mittal R, Lisi CV, Gerring R, et al. Current concepts in the pathogenesis and treatment of chronic suppurative otitis media[J]. J Med Microbiol, 2015, 64(10): 1103-1116. doi: 10.1099/jmm.0.000155
[2] 黄选兆, 汪吉宝, 孔维佳. 实用耳鼻咽喉头颈外科学[M]. 2版. 北京: 人民卫生出版社, 2008: 888-894.
[3] 柴永川, 杨洁, 汪照炎, 等. 耳内镜下Ⅰ型鼓室成形干湿耳手术疗效分析[J]. 中国耳鼻咽喉颅底外科杂志, 2018, 24(1): 24-28. https://www.cnki.com.cn/Article/CJFDTOTAL-ZEBY201801007.htm
[4] Webb BD, Chang CY. Efficacy of tympanoplasty without mastoidectomy for chronic suppurative otitis media[J]. Arch Otolaryngol Head Neck Surg, 2008, 134(11): 1155-1158. doi: 10.1001/archotol.134.11.1155
[5] McGrew BM, Jackson CG, Glasscock ME, et al. Impact of mastoidectomy on simple tympanic membrane perforation repair[J]. Laryngoscope, 2004, 114(3): 506-511. doi: 10.1097/00005537-200403000-00023
[6] Albu S, Trabalzini F, Amadori M, et al. Usefulness of cortical mastoidectomy in myringoplasty[J]. Otol Neurotol, 2012, 33(4): 604-609. doi: 10.1097/MAO.0b013e31825368f2
[7] Trinidade A, Page JC, Dornhoffer JL, et al. Therapeutic Mastoidectomy in the Management of Noncholesteatomatous Chronic Otitis Media: Literature Review and Cost Analysis[J]. Otolaryngol Head Neck Surg, 2016, 155(6): 914-922. doi: 10.1177/0194599816662438
[8] Pignataro L, Grillo Della Berta L, Capaccio P, et al. Myringoplasty in children: anatomical and functional results[J]. J Laryngol Otol, 2001, 115(5): 369-373. doi: 10.1258/0022215011907893
[9] Denoyelle F, Roger G, Chauvin P, et al. Myringoplasty in Children: Predictive Factors of Outcome[J]. Laryngoscope, 1999, 109(1): 47-51. doi: 10.1097/00005537-199901000-00010
[10] Mills R, Thiel G, Mills N. Results of myringoplasty operations in active and inactive ears in adults[J]. Laryngoscope, 2013, 123(9): 2245-2249. doi: 10.1002/lary.23772
-




 下载:
下载: