Evaluation of the effectiveness of immersive virtual reality-based exercise system for vestibular rehabilitation
-
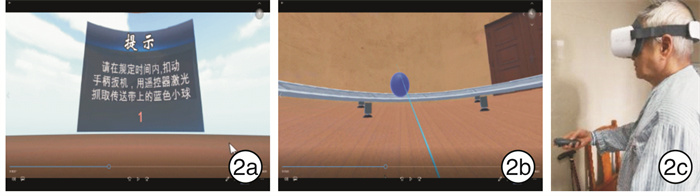
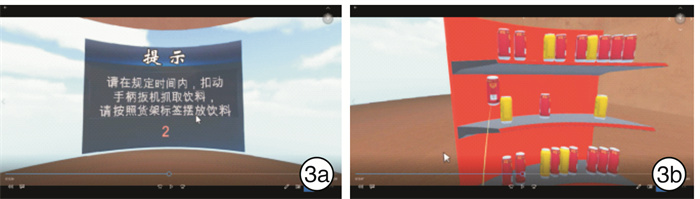
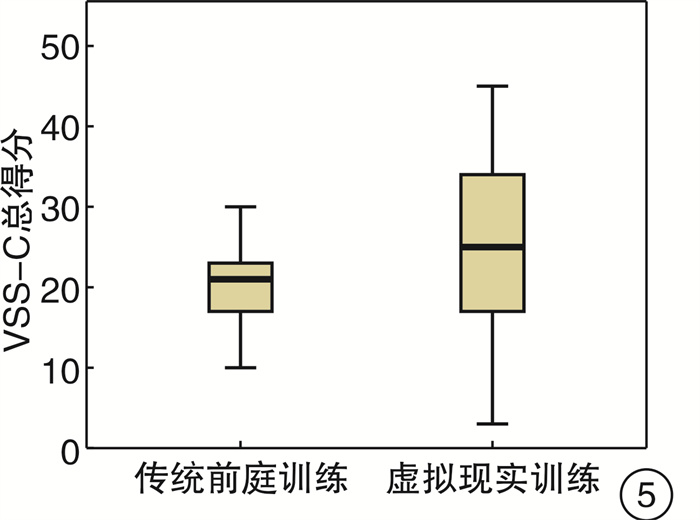
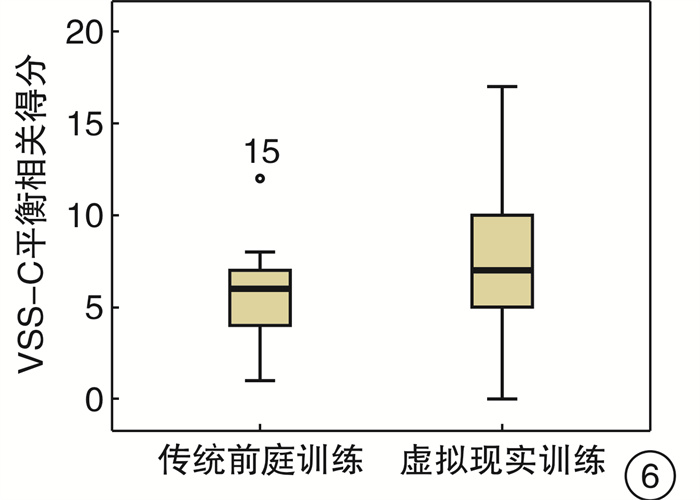
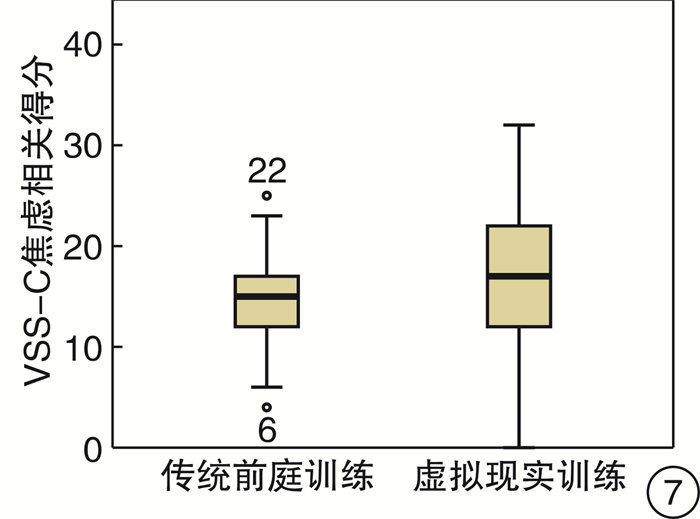
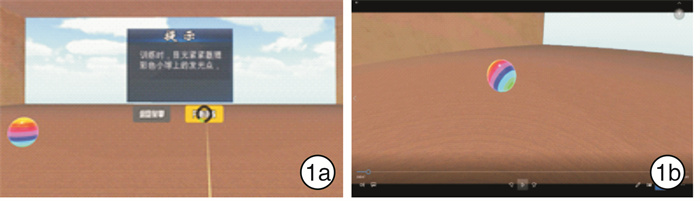
摘要: 目的 探讨虚拟现实(VR)技术辅助前庭康复训练(VRT)治疗慢性前庭功能低下的作用和价值。方法 按机械抽样方法将98例慢性前庭功能低下患者分为实验组(VR组)73例和控制组25例,VR组采取沉浸式VR辅助VRT方法治疗,控制组采取常规VRT治疗。治疗前和治疗后第12周,采用汉化眩晕症状量表(VSS-C)进行评分,评估患者治疗前后眩晕症状变化。平衡功能评估采用平衡仪测定人体中心压力(COP)、最大摆动长度(MOL)及COP摆动包络面积(EA)数据,数字越小表示平衡能力越好。采用SPSS 20.0统计软件进行数据分析。结果 ① VR组治疗后12周较治疗前VSS-C量表总分、平衡相关得分差异有统计学意义(P < 0.01)。治疗后2组VSS-C量表总分(P < 0.01)、平衡相关得分(P < 0.05)差异有统计学意义。②平衡仪COP测定,2种训练方法治疗12周前后,MOL、EA睁眼状态下差异均有统计学意义(P < 0.01)。结论 VRT引入VR技术能够在训练中为患者提供有趣的互动,鼓励患者更积极主动地参与康复锻炼,达到良好效果。VR技术在患者无视力障碍的前提下对主观平衡康复的疗效优于常规VRT训练方法。Abstract: Objective To evaluate the efficacy of virtual reality technology assisted vestibular rehabilitation training(VRT) in treating chronic vestibular dysfunction patients.Method Ninety-eight vestibular dysfunction patients were assigned into the experimental group(n=73) and the control group(n=25) using mechanical sampling. The experimental group received immersive virtual reality assisted VRT treatment, while the control group received conventional VRT treatment. Chinese vertigo symptom scale(VSS-C) was used to measure vertigo symptoms before treatment and 12 weeks post-treatment. Balance feedback instrument was used to measure the center of pressure(COP), maximum oscillation length(MOL) and COP envelope area(EA) which smaller numbers indicating better balance functions. Analysis of variance and Fisher's exact test were performed using SPSS 20.0 software to compare mean values and frequencies, respectively.Result ① Before treatment as baseline, there were no statistically significant differences in the total score of VSS-C scale, balance correlation and anxiety correlation score between the two groups. Total score and balance related score of experimental group were significantly different between before and after treatment(P < 0.01), while no statistically significant difference in anxiety related scores. After treatment, there were statistically significant differences in total VSS-C score(P < 0.01) and balance correlation score(P < 0.05) between the two groups, while no statistically significant difference in anxiety correlation score. ②After 12 weeks of treatment, there were statistically significant differences between MOL and EA in open-eye state(P < 0.01), but no statistically significant difference in close-eye state between two groups.Conclusion The introduction of VR technology by VRT can provide interesting interactions for patients in training and encourage patients to actively participate in various repetitive rehabilitation exercises that are boring, achieving good effect. The effect of VR on subjective balance rehabilitation without visual impairment is better than that of conventional.
-
Key words:
- vertigo /
- virtual reality /
- vestibular rehabilitation training
-

-
表 1 2组患者的资料
例 项目 VR组 控制组 性别 男 42 14 女 31 11 年龄/岁 46.97±15.32 35.00±20.71 诊断 前庭神经炎 11 5 梅尼埃病 9 4 持续性姿势-知觉性头晕 8 4 闭合性颅脑外伤 7 2 难治性BBPV 31 6 前庭性偏头痛 3 2 放射性脑病 4 2 前庭功能减退 左 21 6 右 22 8 双 30 11 视觉障碍 2 0 表 2 2组患者治疗前VSS-C量表得分比较
x±s VR组 控制组 F P 平衡相关 16.47±6.86 16.44±5.69 9.12 0.48 焦虑相关 21.42±7.20 29.68±10.51 8.87 0.28 总分 41.36±13.02 33.68±13.50 17.30 0.66 表 3 VR组治疗前后VSS-C得分比较
x±s 治疗前 治疗后 F P 平衡相关 16.47±6.86 7.99±4.40 9.21 <0.01 焦虑相关 21.42±7.20 21.19±8.33 8.87 0.58 总分 41.36±13.02 24.59±10.77 17.30 <0.01 表 4 2种训练方法治疗前后睁眼状态COP
mm, x±s 组别 治疗前 治疗后 P MOL EA MOL EA VR组 271.65±134.56 1091.91±438.27 98.01±78.63 487.28±167.38 <0.01 控制组 229.65±138.54 970.19±343.57 130.78±107.25 674.76±251.57 <0.01 表 5 2种训练方法治疗前后闭眼状态COP
mm, x±s 组别 治疗前 治疗后 P MOL EA MOL EA VR组 387.95±320.80 1426.30±479.87 271.74±148.80 1233.21±313.28 >0.05 控制组 343.59±205.42 1400.78±521.88 276.48±148.27 1140.06±766.47 >0.05 -
[1] 孙勍, 戴静, 彭新, 等. 美国外周前庭功能低下前庭康复训练临床指南简要解读[J]. 中华全科医师杂志, 2019, 18(3): 228-231. doi: 10.3760/cma.j.issn.1671-7368.2019.03.004
[2] 杨军, 郑贵亮. 进一步重视前庭康复[J]. 临床耳鼻咽喉头颈外科杂志, 2019, 33(3): 204-206. http://lceh.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=339ae9b4-aeb6-4210-b5da-d681d871f8c0
[3] 姜树军, 彭新, 单希征, 等. 巴拉尼协会双侧前庭病诊断标准解读[J]. 北京医学, 2018, 40(8): 789-791. https://www.cnki.com.cn/Article/CJFDTOTAL-BJYX201808022.htm
[4] 邓真, 元唯安, 王辉昊, 等. 眩晕症状量表的汉化及信效度和反应度检验[J]. 浙江大学学报(医学版), 2015, 3(4): 138-144. https://www.cnki.com.cn/Article/CJFDTOTAL-ZJYB201502005.htm
[5] 焦粤农, 于锋, 钟胜长, 等. 中文译本耳鸣致残量表的临床应用研究[J]. 临床耳鼻咽喉头颈外科杂志, 2016, 30(11): 907-910. http://lceh.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=6057791c-d387-40b7-83de-924b646ca44a
[6] van Kerckhoven G, Mert A, De Ru JA. Treatment of vertigo and postural instability usingvisual illusions[J]. J Laryngol Otol, 2014, 128(11): 1005-1007. doi: 10.1017/S0022215114002254
[7] 王瑞丹, 黄佩玲, 公维军. 虚拟现实技术在帕金森病冻结步态康复中的应用进展研究[J]. 中国康复理论与实践, 2018, 24(7): 791-794. doi: 10.3969/j.issn.1006-9771.2018.07.006
[8] 赵一瑾, 余彬, 何龙龙. 虚拟现实技术结合作业治疗训练对脑卒中偏瘫患者上肢功能影响的临床研究[J]. 中国康复医学杂志, 2019, 34(6): 661-666. doi: 10.3969/j.issn.1001-1242.2019.06.007
[9] de Rooij IJM, van de Port IGL, Visser-Meily JMA, et al. Virtual reality gait training versus non-virtual reality gait training for improving participation in subacute stroke survivors: study protocol of the ViRTAS randomized controlled trial[J]. Trials, 2019, 20(1): 89. doi: 10.1186/s13063-018-3165-7
[10] Gonçalves MG, Piva MFL, Marques CLS, et al. Effects of virtual reality therapy on upper limb function after stroke and the role of neuroimagingas a predictor of a better response[J]. Arq Neuropsiquiatr, 2018, 76(10): 654-662. doi: 10.1590/0004-282x20180104
[11] 刘婷婷, 刘箴, 钱平安, 等. 虚拟现实在特殊人群康复中的应用研究[J]. 系统仿真学报, 2018, 30(9): 3229-3237. https://www.cnki.com.cn/Article/CJFDTOTAL-XTFZ201809001.htm
[12] Donath L, Rössler R, Faude O. Effects of Virtual Reality Training(Exergaming)Compared to Alternative Exercise Training and Passive Control on Standing Balance and Functional Mobility in Healthy Community-Dwelling Seniors: A Meta-Analytical Review[J]. Sports Med, 2016, 46(9): 1293-1309. doi: 10.1007/s40279-016-0485-1
[13] Micarelli A, Viziano A, Augimeri I, et al. Three-dimensional head-mounted gaming taskprocedure maximizes effects of vestibular rehabilitation in unilateral vestibular hypofunction: a randomized controlledpilot trial[J]. Int J Rehabil Res, 2017, 40(4): 325-332. doi: 10.1097/MRR.0000000000000244
[14] Rosiaka O, Krajewski K, Woszczak M, et al. Evaluation of the effectiveness of a Virtual Reality-based exerciseprogram for Unilateral Peripheral Vestibular Deficit[J]. J Vestib Res, 2018, 28(5-6): 409-415.
[15] Sato G, Matsuda K, Matsuoka M. Comparative study of anti-vertiginous and anti-anxious drugs for the treatment of chronic vestibularpatients with secondary anxiety[J]. J Acta Otolaryngol, 2019, 139(7): 593-597. doi: 10.1080/00016489.2019.1612531
[16] Staab JP. Psychiatric Considerations in the Management of Dizzy Patients[J]. J Adv Otorhinolaryngol, 2019, 82: 170-179.
[17] Jahn K. The Aging Vestibular System: Dizziness and Imbalance in the Elderly[J]. J Adv Otorhinolaryngol, 2019, 82: 143-149.
[18] 吴子明. 前庭康复[M]. 4版. 郑州: 河南科学技术出版社, 2018: 313-322
-




 下载:
下载: