Analysis of the incidence and influencing factors of collateral circulation in high-risk patients with sleep apnea complicated with stroke treated by continuous positive pressure ventilation
-
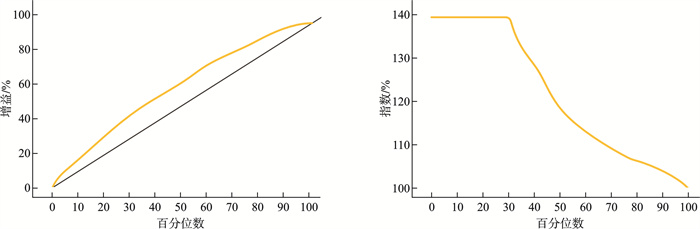
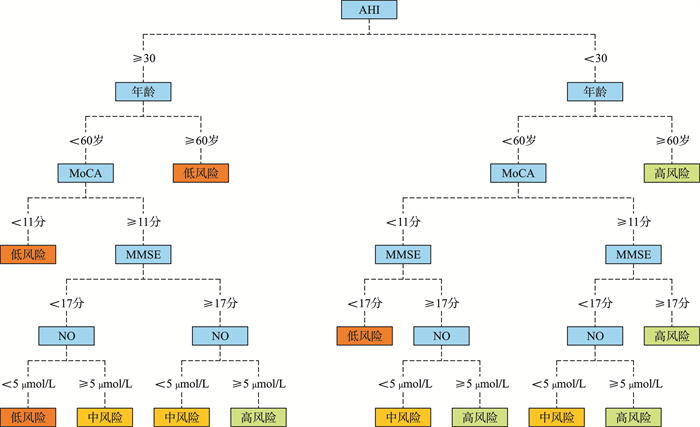
摘要: 目的 探讨睡眠呼吸暂停合并卒中高危人群经持续正压通气治疗侧支循环发生情况及影响因素分析。 方法 选取2020年1月-2022年6月郑州人民医院收治的阻塞性睡眠呼吸暂停低通气综合征(OSAHS)合并脑卒中患者152例作为研究对象,根据患者睡眠呼吸暂停低通气指数(AHI)将患者分为轻度组(n=44),中度组(n=72)和重度组(n=36),治疗后根据患者是否发生侧支循环将患者分为无侧支循环组(n=30)和有侧支循环组(n=122),根据侧支循环程度分为侧支循环较差(n=26)、侧支循环中等(n=69)、侧支循环良好(n=27),比较不同组患者临床资料,多因素分析影响患者发生侧支循环的因素。 结果 重度组患者AHI和IL-6水平显著高于轻度组和中度组,NO和PO2水平则显著低于轻度组和中度组,3组患者之间的差异有统计学意义(P<0.05),治疗后,各组患者均有所好转,轻度组、中度组和重度组发生侧支循环的人数占比分别为84.09%,81.94%和72.22%。有侧支循环组和无侧支循环组在年龄、AHI、NIHSS、NO、MoCA、MMSE方面的差异有统计学意义(P<0.05)。有侧支循环组中,侧支循环良好组年龄、AHI、NIHSS评分显著低于侧支循环较差和侧支循环中等组,NO水平、MoCA评分、MMSE评分显著高于侧支循环较差和侧支循环中等组。多因素分析结果显示,年龄、AHI、NIHSS是侧支循环发生的独立危险因素,NO、MoCA、MMSE是侧支循环发生的保护因素,与侧支循环发生呈负相关。分类树模型结果显示,以上5个影响因素中,AHI对患者发生侧支循环的影响最大。经检验,该模型的预测效果良好。 结论 睡眠呼吸暂停合并卒中高危人群经持续正压通气治疗后大部分患者会发生侧支循环,年龄、AHI、NIHSS、NO、MoCA、MMSE是影响侧支循环发生的重要因素。
-
关键词:
- 阻塞性睡眠呼吸暂停低通气综合征 /
- 急性缺血性脑卒中 /
- 持续气道正压 /
- 侧支循环
Abstract: Objective To investigate the incidence of collateral circulation in high-risk patients with sleep apnea and stroke treated by continuous positive airway pressure (CPAP) ventilation and to analyze the influencing factors. Methods A total of 152 patients diagnosed with obstructive sleep apnea-hypopnea syndrome (OSAHS) combined with acute ischemic stroke (AIS) who were admitted to our hospital from January 2020 to June 2022 were selected for this study. Based on the apnea-hypopnea index (AHI), the patients were divided into three groups: mild (n=44), moderate (n=72), and severe (n=36). After treatment, the patients were further classified into a group without collateral circulation (n=30) and a group with collateral circulation (n=26), which included those with moderate collateral circulation (n=69) and good collateral circulation (n=27). Clinical data across the different groups were compared, and multiple factor analysis was performed to identify factors affecting the occurrence of collateral circulation. Results The AHI and IL-6 levels in the severe group were significantly higher than those in the mild and moderate groups, while the levels of NO and PO2 were significantly lower in the severe group compared to the mild and moderate groups, with statistically significant differences among the three groups (P < 0.05). After treatment, all groups showed improvement, and the proportion of patients with collateral circulation was 84.09% in the mild group, 81.94% in the moderate group, and 72.22% in the severe group. Significant differences in age, AHI, NIHSS, NO, MoCA, and MMSE scores were observed between the groups with and without collateral circulation (P < 0.05). In the group with collateral circulation, the scores for age, AHI, and NIHSS in the good collateral circulation subgroup were significantly lower than those in the poor collateral circulation and moderate collateral circulation subgroups, while the scores for NO, MoCA, and MMSE were significantly higher in the good collateral circulation subgroup. Multi-factor analysis revealed that age, AHI, and NIHSS were independent risk factors for collateral circulation, whereas NO, MoCA, and MMSE served as protective factors that were negatively correlated with collateral circulation. Classification tree model results indicated that AHI had the greatest influence on the occurrence of collateral circulation among the five influencing factors, demonstrating good predictive capability. Conclusion Most high-risk patients with sleep apnea and stroke are likely to develop collateral circulation following continuous positive airway pressure ventilation. Factors such as age, AHI, NIHSS, NO, MoCA, and MMSE are important determinants affecting the occurrence of collateral circulation. -

-
表 1 不同程度OSAHS合并脑卒中患者的临床资料比较
X±S 项目 轻度(n=44) 中度(n=72) 重度(n=36) F/χ2 P 性别/例(%) 1.298 0.523 男 26(59.09) 38(52.78) 23(63.89) 女 18(40.91) 34(47.22) 13(36.11) 2.770 0.066 年龄/岁 56.68±3.52 58.16±4.11 60.58±4.20 1.954 0.053 BMI/kg/m2 24.28±0.45 25.61±0.52 26.37±0.57 吸烟史/例(%) 30(68.18) 52(72.22) 25(69.44) 0.234 0.889 饮酒史/例(%) 28(63.64) 50(69.44) 24(66.67) 0.422 0.810 高血压/例(%) 19(43.18) 22(30.56) 16(44.44) 2.828 0.243 糖尿病/例(%) 15(34.09) 20(27.78) 17(47.22) 4.032 0.133 心率/次/min 79.85±8.17 80.28±8.02 81.54±9.10 0.874 0.385 收缩压/mmHg 130.44±20.81 128.23±20.92 127.78±21.80 0.557 0.579 舒张压/mmHg 74.41±10.03 75.22±9.06 75.38±9.74 0.885 0.379 TC/mmol/L 3.90±0.66 4.15±0.52 4.80±0.60 1.755 0.083 TG/mmol/L 1.58±0.07 1.61±0.11 1.63±0.10 1.574 0.119 LDL-C/mmol/L 2.36±0.13 2.41±0.10 2.44±0.12 1.050 0.297 HDL-C/mmol/L 1.25±0.08 1.30±0.15 1.37±0.13 1.745 0.084 FPG/mmol/L 5.80±0.35 5.86±0.40 5.95±0.44 1.699 0.093 AHI/次/h 12.98±1.73 23.54±4.26 41.29±8.50 14.490 <0.001 NO/μmol/L 6.03±1.10 5.62±0.73 4.98±0.94 9.264 <0.001 IL-6/pg/mL 164.28±15.67 170.42±12.73 175.33±16.72 3.045 0.003 CRP/mg/L 5.37±1.33 5.85±1.42 6.08±1.40 1.809 0.073 PO2/mmHg 91.55±17.60 88.41±19.96 84.07±15.35 2.002 0.049 1 mmHg=0.133 kPa 表 2 不同程度患者治疗效果分析
X±S 项目 轻度(n=44) 中度(n=72) 重度(n=36) F P SL/min 治疗前 18.29±1.76 20.57±4.20 21.65±4.47 1.428 0.156 治疗后 12.33±2.031) 12.68±3.251) 13.14±2.661) 1.544 0.126 REM-SL/min 治疗前 142.26±16.18 149.30±15.29 153.65±17.69 1.288 0.200 治疗后 110.48±12.351) 126.82±13.471) 132.22±14.361) 1.921 0.057 SE/% 治疗前 78.08±11.54 73.56±13.23 70.82±10.93 1.210 0.229 治疗后 90.65±12.401) 87.68±10.551) 85.49±9.661) 1.565 0.120 N1期睡眠比率/% 治疗前 15.48±2.26 18.35±2.06 21.29±1.52 6.370 <0.001 治疗后 6.36±2.041) 8.22±3.141) 9.54±1.681) 1.836 0.070 N2期睡眠比率/% 治疗前 50.64±10.45 44.56±10.58 38.59±9.62 15.076 <0.001 治疗后 58.19±8.671) 50.40±11.321) 43.05±13.661) 8.275 <0.001 N3期睡眠比率/% 治疗前 8.39±1.86 6.28±1.37 4.14±2.03 6.008 <0.001 治疗后 17.57±3.051) 13.09±2.341) 10.18±1.661) 3.741 <0.001 REM期比率/% 治疗前 12.50±4.31 10.87±2.64 10.96±3.28 1.765 0.081 治疗后 18.49±3.551) 17.25±3.061) 16.92±2.151) 0.859 0.393 LSaO2/% 治疗前 82.17±12.60 74.52±8.67 69.48±11.42 8.267 <0.001 治疗后 93.56±10.221) 85.06±10.151) 78.24±9.571) 6.785 <0.001 AHI/次/h 治疗前 12.98±1.73 23.54±4.26 41.29±8.50 9.748 <0.001 治疗后 6.35±1.551) 15.09±2.301) 23.16±3.351) 5.304 <0.001 NIHSS评分/分 治疗前 18.50±2.04 20.37±2.35 22.78±1.96 3.585 <0.001 治疗后 8.86±1.211) 12.45±1.661) 16.20±2.011) 4.178 <0.001 PSQI评分/分 治疗前 10.08±1.37 13.69±2.04 16.15±1.42 2.696 0.009 治疗后 7.11±1.051) 8.28±1.671) 10.79±2.111) 4.978 <0.001 ESS评分/分 治疗前 9.80±1.16 11.58±1.44 13.26±2.04 1.681 0.096 治疗后 7.13±2.011) 8.67±1.061) 10.05±1.531) 1.879 0.063 MoCA/分 治疗前 15.69±2.10 13.01±1.85 11.47±3.04 1.571 0.120 治疗后 22.14±1.531) 19.67±2.091) 18.24±1.681) 1.516 0.133 MMSE/分 治疗前 21.20±1.53 20.86±1.60 19.59±2.16 1.476 0.144 治疗后 25.06±2.451) 24.50±1.431) 23.42±1.681) 1.331 0.187 与治疗前比较,1)P<0.05。 表 3 不同程度患者治疗后侧支循环发生情况
例(%) 项目 轻度(n=44) 中度(n=72) 重度(n=36) χ2 P 无侧支循环 7(15.91) 13(18.06) 10(27.78) 2.005 0.367 有侧支循环 37(84.09) 59(81.94) 26(72.22) 侧支循环发生程度 20.621 <0.001 循环较差 4(10.81) 9(15.25) 13(50.00) 循环中等 20(54.05) 40(67.80) 9(34.62) 循环良好 13(35.14) 10(16.95) 4(15.38) 表 4 侧支循环发生的临床资料比较
X±S 项目 无侧支循环(n=30) 有侧支循环(n=122) t/χ12 P1 F/χ22 P2 较差(n=26) 中等(n=69) 良好(n=27) 性别/例(%) 0.783 0.376 1.219 0.544 男 17(56.67) 15(57.69) 47(68.12) 16(59.26) 女 13(43.33) 11(42.31) 22(31.88) 11(40.74) 年龄/岁 61.10±4.10 60.10±4.10 58.43±5.15 56.48±4.02 5.275 <0.001 3.245 0.002 BMI/kg/m2 24.09±1.47 24.09±1.47 23.55±1.59 23.07±0.98 吸烟史/例(%) 20(66.67) 16(61.54) 51(73.91) 18(66.67) 0.134 0.714 1.517 0.468 饮酒史/例(%) 18(60.00) 17(65.38) 49(71.01) 15(55.56) 0.606 0.436 2.094 0.351 高血压/例(%) 9(30.00) 11(42.31) 20(28.99) 10(37.04) 0.193 0.661 1.685 0.431 糖尿病/例(%) 8(26.67) 10(38.46) 22(31.88) 15(55.56) 2.085 0.149 4.592 0.101 心率/次/min 81.64±9.00 81.25±8.05 80.37±7.73 79.08±7.27 1.462 0.146 0.853 0.395 收缩压/mmHg 129.01±19.08 130.01±19.22 129.55±20.14 131.27±18.80 0.579 0.563 0.325 0.745 舒张压/mmHg 75.68±9.83 73.91±9.31 74.25±10.26 73.58±9.03 0.700 0.485 0.442 0.658 TC/mmol/L 4.83±0.62 3.95±0.43 4.12±0.51 3.84±0.56 1.212 0.227 0.956 0.341 TG/mmol/L 1.65±0.09 1.57±0.07 1.60±0.10 1.53±0.05 0.666 0.506 0.466 0.642 LDL-C/mmol/L 2.45±0.12 2.34±0.09 2.42±0.11 2.30±0.10 0.866 0.388 0.333 0.740 HDL-C/mmol/L 1.38±0.14 1.26±0.07 1.32±0.12 1.23±0.05 1.066 0.288 0.932 0.353 FPG/mmol/L 5.97±0.28 5.80±0.34 5.86±0.38 5.78±0.23 1.448 0.150 0.905 0.367 NO(μmol/L) 4.74±0.44 5.50±0.23 6.10±1.12 6.14±1.06 1.991 0.048 2.353 0.020 IL-6/pg/mL 175.89±15.92 172.09±14.50 164.79±14.16 162.85±13.67 1.267 0.207 1.636 0.104 CRP/mg/L 7.05±1.31 6.11±1.12 5.25±1.24 5.10±1.03 1.086 0.279 1.432 0.154 PO2/mmHg 88.86±17.55 89.40±15.06 90.35±18.23 92.59±15.60 1.405 0.162 0.181 0.857 SL/min 21.78±3.49 20.77±3.24 18.17±2.60 17.05±1.02 1.368 0.173 1.334 0.184 REM-SL/min 150.64±16.83 143.27±20.09 141.67±19.05 140.11±18.14 0.965 0.336 0.996 0.321 SE/% 72.40±8.91 76.39±9.43 78.12±12.07 79.33±10.22 1.304 0.194 1.402 0.163 N1/% 21.93±2.54 19.46±1.87 16.05±2.16 15.81±1.08 1.179 0.240 1.327 0.187 N2/% 37.38±10.02 45.03±9.46 48.62±10.12 50.84±9.68 1.941 0.054 1.450 0.149 N3/% 5.11±2.18 6.20±1.15 8.44±1.08 8.50±1.29 1.695 0.092 1.425 0.156 REM/% 10.40±3.00 10.64±2.72 11.13±2.35 12.72±3.20 1.081 0.281 0.688 0.493 LSaO2/% 65.89±10.30 82.49±12.74 76.32±10.67 83.34±13.36 1.916 0.057 1.671 0.097 AHI/次/h 43.25±4.61 25.64±3.16 14.08±2.03 10.57±1.84 8.747 <0.001 7.731 <0.001 NIHSS/分 23.29±3.26 21.47±2.52 19.13±1.84 17.42±2.15 3.078 0.002 2.716 0.007 PSQI/分 16.85±1.92 13.96±2.11 12.34±1.55 10.01±1.08 1.297 0.197 1.204 0.231 ESS/分 13.76±1.48 11.44±1.54 10.82±2.06 9.52±1.14 0.958 0.339 0.958 0.340 MoCA/分 10.58±1.05 12.15±1.76 14.29±2.12 16.76±1.65 3.802 <0.001 2.534 0.012 MMSE/分 16.37±2.14 18.83±1.55 20.68±1.73 22.15±1.42 2.353 0.020 3.668 <0.001 注:P1表示无侧支循环组和有侧支循环组的差异,P2表示有侧支循环组中,侧支循环较差、中等、良好组之间的差异,P<0.05表示差异有统计学意义。 表 5 多因素分析各指标对侧支循环发生的影响
因素 β SE Wald OR(95%CI) P 年龄 0.579 0.224 6.691 1.785(1.101~1.930) <0.001 NO -0.403 0.311 1.683 0.852(0.502~0.988) 0.007 AHI 0.455 0.505 0.811 1.576(1.214~1.847) <0.001 NIHSS 0.326 0.216 2.274 1.385(1.230~1.971) 0.001 MoCA -0.248 0.216 1.323 0.780(0.495~0.969) <0.001 MMSE -0.160 0.157 1.041 0.668(0.525~0.956) <0.001 -
[1] 龚琴, 王海燕, 谢晓玮, 等. 中重度阻塞性睡眠呼吸暂停低通气综合征的危险因素分析及风险预测模型的构建[J]. 现代生物医学进展, 2023, 23(17): 3268-3272, 3262.
[2] Li SY, Zheng W, Wang X, et al. The impact of obstructive sleep apnea and comorbidity status on cardiovascular outcomes in patients with acute coronary syndrome[J]. Nutr Metab Cardiovasc Dis, 2023, 33(12): 2372-2383.
[3] 王连辉, 元小冬, 徐斌, 等. 阻塞性睡眠呼吸暂停低通气综合征与卒中[J]. 实用心脑肺血管病杂志, 2023, 31(6)122-126.
[4] Scanning. Retracted: Effects of Obstructive Sleep Apnea-Hypopnea Syndrome and Cognitive Function in Ischemic Stroke Based on Linear Regression Equation[J]. Scanning, 2023, 2023: 9763714.
[5] Ji P, Kou Q, Qu X, et al. Effects of Obstructive Sleep Apnea-Hypopnea Syndrome and Cognitive Function in Ischemic Stroke Based on Linear Regression Equation[J]. Scanning, 2022, 2022: 4105169.
[6] 张新静, 王迪琼, 陆小威, 等. CPAP治疗OSAHS合并脑卒中的临床研究[J]. 临床肺科杂志, 2021, 26(8): 1143-1147.
[7] Wang B, Hao W, Fan JY, et al. Clinical significance of obstructive sleep apnea in patients with acute coronary syndrome with or without prior stroke: a prospective cohort study[J]. Eur J Med Res, 2023, 28(1): 107.
[8] 李少宁, 秦娜, 高影, 等. 脑梗死合并OSAHS患者血清MCP-1、HSP70、AOPP的表达水平及临床意义[J]. 海南医学, 2023, 34(5): 680-683.
[9] Condoleo V, Bonfrate L, Armentaro G, et al. Effects of continuous positive airway pressure on comprehensive geriatric assessment and cognitive function in elderly patients with obstructive sleep apnea syndrome[J]. Intern Emerg Med, 2023, 18(3): 769-779.
[10] 陶景山, 臧晓进, 戴益盛, 等. 四维CT血管造影评估的急性缺血性脑卒中患者脑侧支循环与预后的相关性[J]. 中华老年多器官疾病杂志, 2022, 21(6): 443-448.
[11] 刘跃男, 许华俊, 钱颖君, 等. 阻塞性睡眠呼吸暂停低通气综合征和代谢综合征关系的最新研究进展[J]. 中国眼耳鼻喉科杂志, 2021, 21(4): 305-308.
[12] 阻塞性睡眠呼吸暂停低通气综合征诊治指南(基层版)写作组. 阻塞性睡眠呼吸暂停低通气综合征诊治指南(基层版)[J]. 中华全科医师杂志, 2015, 14(7): 509-515.
[13] 钟迪, 张舒婷, 吴波. 《中国急性缺血性脑卒中诊治指南2018》解读[J]. 中国现代神经疾病杂志, 2019, 19(11): 897-901.
[14] 许金回, 岳红梅, 刘苗苗, 等. 腰臀比对阻塞性睡眠呼吸暂停低通气综合征的筛查价值[J]. 临床肺科杂志, 2023, 28(10): 1554-1558.
[15] Yuan K, Xie MD, Hou HJ, et al. Association of glycemic gap with stroke recurrence in patients with ischemic stroke[J]. J Diabetes, 2023, 15(9): 714-723.
[16] Hoang-Anh T, Duong-Minh Q, Nguyen-Thi-Y N, et al. Study of the obstructive sleep apnea syndrome in cerebral infarction patients[J]. Front Neurol, 2023, 14: 1132014.
[17] Sunnetcioglu A, Cilingir BM, Gunbatar H, et al. Factors determining the therapeutic level of positive airway pressure in patients with obstructive sleep apnea syndrome[J]. Lung India, 2023, 40(2): 112-116.
[18] Vaioli G, Tagini S, Scarpina F, et al. Short-term benefits of continuous positive airway pressure treatment on cognition in the obstructive sleep apnea syndrome: a retrospective study[J]. Brain Sci, 2023, 13(1): 124.
[19] 张士玉, 姚柳, 姜亦伦. 全脑CTP及动态CTA评估单侧大脑中动脉狭窄或闭塞患者侧支循环状态及预后的价值[J]. 医学影像学杂志, 2023, 33(7): 1137-1140.
[20] Cipolla MJ. Therapeutic induction of collateral flow[J]. Transl Stroke Res, 2023, 14(1): 53-65.
[21] Scavasine VC, Stoliar GA, de Almeida Teixeira BC, et al. Automated evaluation of collateral circulation for outcome prediction in acute ischemic stroke[J]. J Stroke Cerebrovasc Dis, 2024, 33(4): 107584.
[22] Chen W, Wang MH, Yang L, et al. White matter hyperintensity burden and collateral circulation in acute ischemic stroke with large artery occlusion[J]. BMC Neurol, 2024, 24(1): 6.
[23] Hao W, Wang B, Fan JY, et al. Obstructive sleep apnea is associated with the long-term prognosis of patients in acute coronary syndromes with prior myocardial infarction: Insights from OSA-ACS study[J]. Sleep Med, 2023, 112: 141-148.
-

计量
- 文章访问数: 122
- 施引文献: 0



 下载:
下载: