-
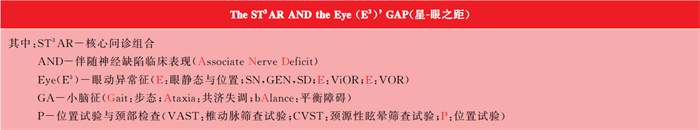
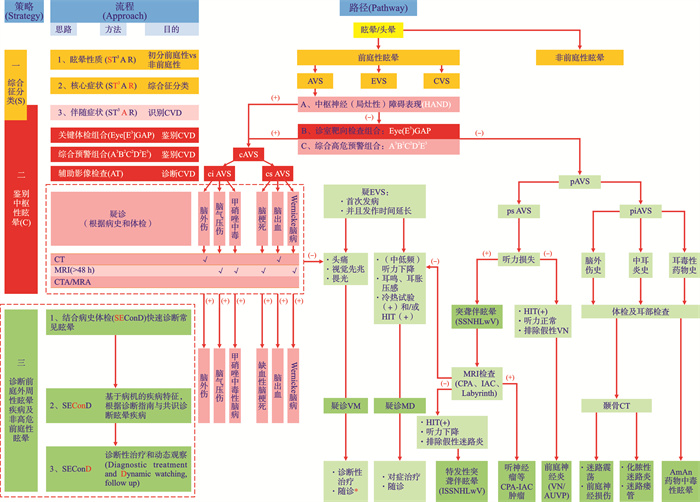
摘要: 急性前庭综合征(AVS)约占普通门诊5%,急诊神经内科20%。中枢性急性前庭综合征属于高危性眩晕疾病,或潜在“致命性”疾病。部分前庭中枢性眩晕(尤其是脑干或小脑缺血性梗死)可表现为孤立性急性眩晕综合征而易引起误诊。近十年来,眩晕疾病的临床诊断模式和诊断路径有较大的发展,Kattah等(2009)报道的HINTS组合检查法和Vanni等(2014)报道的STANDING组合检查法以及Brandt等(2017)报道的五步检查法被临床上广泛用于鉴别脑卒中。Newman-Toker和Edlow(2015)提出了眩晕疾病的TiTrATE诊断模式,Gurley和Edlow(2019)提出了急性眩晕的ATTEST诊断路径模式。但是临床上仅约50%的小脑梗死患者有自发性眼震,且方向改变性眼震对急性前庭综合征卒中的预测敏感性仅38%;而水平头脉冲检查结果正常时,对AICA卒中的预测敏感性仅62%。因此,后循环障碍引起的孤立性眩晕的鉴别检查组合以及AVS鉴别诊断流程尚需进一步完善。本文在笔者眩晕疾病SCD诊断策略及路径的基础上,提出急性前庭综合征的SCD程序式诊断模式,进一步总结了中枢性前庭性眩晕的ABC鉴别模式[A:伴发神经表现;B:Eye(E3)GAP检查组合;C:A3B2C2D2E3综合预警组合],并提出了AVS疾病的鉴别诊断路径。急性前庭综合征中枢性眩晕伴发临床表现问诊和体检核心组合模式可总结为一句非逻辑的英文短语:“HAND-Eye(E3)GAP”(“手-眼之距”)以便记忆。Abstract: Acute vestibular syndrome(AVS) accounts for about 5% of walk clinic, and 20% of neurology consultations in the emergency department. A central acute vestibular syndrome is of high-risk vertigo disorders or potentially life-threaten disorders. Some of the central vestibular vertigo, especially brainstem or cerebellar ischemic infarction, can be misdiagnosed due to the absence of focal neurological symptoms and signs. In the past decade, the diagnosis mode and diagnosis pathway of vestibular syndrome have been made great progress. The HINTS examination battery reported by Kattah et al. (2009), the STANDING examination battery reported by Vanni et al. (2014) as well as the "Big five" step examination procedure reported by Brandt et al. (2017) have been used widely to identify stroke in clinic. The TiTrATE proposed by Newman Toker and Edlow(2015) as well as the ATTEST proposed by Gurley and Edlow(2019) have promoted the accuracy for AVS diagnosis. However, only about 50% of patients with cerebellar ischemic infarction have spontaneous nystagmus. The sensitivity of direction-changing nystagmus in diagnostic predicting stroke in acute vestibular syndrome was only 38%. The diagnostic predictive sensitivity of AICA stroke was only 62% when the horizontal head pulse test were normal. Therefore, the bed-side test battery for differentiating acute isolated vertigo as well as the diagnosis approach of AVS need to be further improved. Based on the SCD diagnosis strategy and the differentiating pathway for vestibular disorders proposed by the author, I propose further in this paper the step-rised SCD strategy for the acute vestibular syndrome, and the ABC mode for differentiating central vestibular vertigo[A: Associated neurological deficit(or: with headache=HAND); B: Eye(E3) GAP examination battery; C: Combined warning battery of A3B2C2D2E3], as well as the differential diagnosis pathway of acute vestibular diseases. The history questioning of associated neurological deficit and the examining batteries for acute central vestibular disorders can be summarized as an illogical English phrase "HAND-Eye(E3) GAP" for memory.
-

-
表 1 急性前庭综合征分类分层常见及重要少见疾病
前庭综合征分类*/分层 眩晕疾病 发作类型(Type)发作时间(Time) 有无诱发(引发)因素(inducing factor) 前庭中枢疾病 前庭外周疾病 急性前庭综合征(AVS) 自发性急性前庭综合征(sAVS) ·后循环缺血性梗死
·小脑出血
·多发性硬化
·Wernicke综合征·前庭神经炎
·特发性突聋伴眩晕
·细菌性迷路炎
·小脑脑桥角肿瘤(如听神经瘤)引发性急性前庭综合征(iAVS) ·脑外伤
·药物毒副作用(如抗癫痫类)·脑外伤
·药物中毒(如AmAn类)注:1.根据文献2、4、16编制。
2. 前庭综合征按发作类型和发作持续时间分为急性前庭综合征(AVS)、急性发作性前庭综合征(EVS)和慢性前庭综合征(CVS)。本表仅列出急性前庭综合征常见及重要少见疾病。
3.AmAn:氨基糖苷类抗生素。表 2 中枢性眩晕特征性临床表现
全身性表现 局灶性神经表现(focal neurological symptoms and signs) 神志 头痛后颈部痛 肢体/头面部感觉运动障碍 霍纳综合征(Horner's Syndrome) 其他脑神经功能障碍(“五D征”) 1.认知状态改变(altered mental status)
2.短暂意识丧失(transient loss of consciousness)1.头痛(Headache)
2.颈部痛/后颈部痛(neck pain/posterior neck pain)一、肢体
1.对侧感觉障碍/感觉异常(hemianesthesia/paresthesia)
2.对侧运动障碍(hemiparalysis/weakness)
二、头面部
1.同侧面部痛或麻木(facial pain or numbness)
2.同侧面瘫/肌弱(facial paralysis)
三、共济障碍与平衡障碍
1.四肢共济障碍(limb ataxia)
2.躯体共济障碍(truncal ataxia)
3.强化Romberg(tandem Romberg)
4.步态共济障碍(gait ataxia)患侧三联征
1.上睑下垂(ptosis)
2.瞳孔缩小(miosis):即两侧瞳孔大小不一(anisocoria)
3.患侧面部无汗1.复视(diplopia,D)
2.视野缺损(visual field deficit,D)
3.辨距不良(dysmetria,D)
4.构音障碍或失声(dysarthria or dysphonia,D)
5.吞咽障碍(dysphagia,D)注:1.根据文献2、3、11、13、15、16、18、19、22、38、43、44、46编制。
2.神志变化对识别中枢源性眩晕有重要意义。
3. 头痛并不是中枢性病变特异性特征性表现。除前庭性偏头痛(特征)外,后循环障碍可引起突发持续性严重头痛,当头痛同时伴其他局灶性神经症状时,应警惕中枢神经源性眩晕。表 3 急性前庭综合征外周性与中枢性前庭反应严重程度鉴别(Proportionality of vestibular symptoms)
病变部位 前庭反应 眩晕 恶心呕吐 自主神经症状(出汗,面色苍白) 平衡障碍 自发性眼震 前庭中枢疾病 程度不定 不定,中度~ 无 较轻 严重(无扶助,几乎不可站立或行走) 不定(可有/可无) 前庭外周疾病 常严重 严重 较重 轻~ 中度(能行走) 常有 注:根据参考文献3、43~46编制。 表 4 诊室检查项目预测前庭中枢性眩晕的敏感性和特殊性
一般神经异常*(General neurologic examination) 脑神经异常**(Abnormal Cranial nerve examination) 自发性眼震*(Spontaneous Nystagmus) 眼震类型*(Nystagmus type) 眼偏斜试验*(Test of Skew) 头脉冲(HIT)* 肢体共济失调**(Limb ataxia) 躯干共济失调*(Truncal gait/ataxia) 串联步态异常**(Tandem gait) 听力下降*(Hearing loss) 敏感性 46.8%(32.3%~61.9%) 7.1%~28.6% 52.3%(29.8%~74.0%) 50.7%(41.1%~60.2%) 23.4%(15%~34.6%) 76.8%(64.4%~85.8%) 5.3%~25% 69.7%(43.3%~87.9%) 9.1%~54.6% 4.3%(1.1%~15.5%) 特殊性 92.8%(75.7%~98.1%) 95.9%~100% 42.0%(15.5%~74.1%) 98.6%(91.7%~99.7%) 97.6%(96.1%~98.6%) 89.1%(75.8%~95.6%) 99.3%~100% 83.7%(52.1%~96.0%) 84.6%~95.4% 95.0%(85.2%~98.4%) 注:1.根据Shah等[42](表 2~表 4)并参照Edlow[11](表 1)编制。
2.*:meta分析,括号外为均值,括号内为范围值。
3.**:未做meta分析之临床报道范围值。表 5 Eye(E3)GAP检查组合中枢性眩晕眼动异常征与小脑征
检查组合 部位 功能 检查项目 前庭中枢性 前庭外周性 E 眼位/眼静态检查 N 自发性眼震(Spontaneous Nystagmus)伴固视抑制(Suppression with fixation) 纯垂直/纯扭转/方向多变常无(固视增强) 纯水平/水平带扭转/垂直带扭转常有 G 凝视性眼震(Gaze evoked nystagmus) 纯垂直/纯扭转,方向改变(双向) 纯水平/水平带扭转,单向 S 眼偏斜(Skew deviation) 常有 无(仅早期存在) E 视-眼动检查(ViOR) S 扫视(Saccade) 变缓或延迟;过冲或欠冲 常无异常 P 平稳跟踪(Smooth Pursuit) 扫视性跟踪(Saccade Pursuit) 常无异常 E 前庭-眼动检查(VOR) H 摇头眼震试验(Head shaking nystagmus test) 错向眼震(Perverted HSN):纯垂直/纯扭转 纯水平/水平带扭转 I 头脉冲试验(Head Impulse test) 正常(前庭神经核病变可同右) 可有纠正性扫视 G 平衡/步态检查 G 闭目站立试验(Romberg test) 重度异常 轻~中度异常 强化Romberg试验(Tandem Romberg test) 重度异常 轻~中度异常 步态试验(Gait) 重度异常 轻~中度异常 A 共济协调检查 A 肢体共济失调试验(Limb coordination/Ataxia test):
—指-鼻试验(Finger - to - nose test)
—指-指试验(Finger - to - finger test)
—双手快速轮替运动试验(Rapid alternating movement test)
—拍膝节律实验(Rhythmic slapping of the knee test)
—(脚)跟-胫(前)试验(Heel - to - shin test)阳性 阴性 躯干共济失调(Truncal Ataxia) 重度异常 轻~中度异常 步态共济失调试验(Gait Ataxia test) 重度异常 轻~中度异常 P 位置试验 P 仰卧转头试验(Supine-roll test/Pagnini-McClure manoeuvres) 错向性眼震(与半规管平面不一致) 眼震与半规管平面一致 位置试验(Dix-Hallpike)Positional test 眼震与半规管平面不一致 眼震与半规管平面一致 注:1.根据参考文献4、11~13、16、19~22、29、38、43~47、49~52编制。
2.某些脑卒中自发性眼震(如:局限性前庭神经核梗死),可表现为外周性眼震特征。
3.HIT阴性提示前庭中枢性病变;但HIT阳性不能排除中枢性病变(假阳性)。
4. E3GAP检查组合用于急性眩晕综合征鉴别中枢源性眩晕疾病。其中:位置性试验(P)主要用于头位诱发眩晕病史的发作性前庭综合征。某些BPPV患者在发作后持续存在头晕时,需与急性前庭综合征疾病鉴别。表 6 中枢性眩晕鉴别诊断诊室检查组合项目对照
检查项目 Eye(E3) GAP HINTS HINTS+ STANDING “Big Five” 十项 三/四项 四/五项 四/五项 五项 自发性眼震(Spontaneous nystagmus)
固视抑制(Suppression with fixation)+ + + + + 凝视性眼震(Gaze evoked nystagmus) + + + + + 眼偏斜(Skew deviation) + + + - + 扫视(Saccade) + - - - - 平稳跟踪(Smooth pursuit) + - - - + 摇头眼震试验(Head shake nystagmus) + - - - - 头脉冲试验(Head impulse test) + + + + + 平衡与步态功能检查(Balance function test)
—Romberg试验(Romberg Test)
—Romberg强化试验(Tandem Romberg Test)
—行走试验(Tandem/Gait test)+ - - + - 共济协调(Ataxia) + - - - - 位置试验(Positional test) + - - + - 弹指听力检查(Finger rub hearing test) - - + - - 注:1.根据文献2、19~22、49、50编制。
2.固视抑制纳入自发性眼震检查项目。表 7 平衡障碍严重程度分级
分级 严重程度 特征(临床表现) 脑卒中阳性预测率 预测脑卒中敏感性 预测脑卒中特异性 0级 正常 正常 0 1级 轻度~中度平衡障碍 无扶助支撑时,可独立行走 7.0 % 7.1% 45.8% 2级 重度平衡障碍 无扶助支撑时,站立时严重平衡障碍或不能独立行走 28.0% 26.2% 61.0% 3级 极重度平衡障碍 无扶助支撑时,不能坐正或站立无扶助站立时摔倒 100.0% 66.7% 100.0% 注:1. 根据Carmonas等(2016)[51] (表 3、表 4)、文献4、51、53,Edlow等(2023)[4] (表 5)和Edlow (2024)[53]引用编制。
2.平衡障碍2或3级时,预测脑卒中的敏感性为93%,特异性为61%。表 8 高危中枢性眩晕A3B2C2D2E3系统预警组合
项目名称 指标 评分 A3 A 年龄(Age) > 50岁 1 A 头痛/颈后部痛(HeadAche/posterior neck pain) 1 A 共济失调(Ataxia) 肢体共济失调(limb ataxia)
躯干共济失调(truncal ataxia)
步态共济失调(gait ataxia)2 B2 B 高血压(Blood tension/hypertension) 1 B 严重平衡障碍(Balance disorder):强化Romberg test (tandem Romberg test) 2 C2 C 心血管疾病(Cardiovascular disease) 1 C 临床神经系统表现(Clinical neurological manifestations) 3 D2 D 糖尿病(Diabetes mellitus) 1 D 眩晕持续时间(Duration)>24 h 1 E3 E 眼位/眼静态检查(Eye position) 眼偏斜 2 自发性中枢性眼震 3 凝视性眼震 3 E 视-眼动态检查(Visual-ocular reflex, ViOR) 扫视/平稳跟踪异常 3 E 前庭眼动检查(Vestibulo-ocular reflex,VOR) 中枢性眼震 3 注:1.根据文献2、3、4、11、12、13、15、16、18、19、22、34、38、42、43、44、46、47、49~52、53总结编制。
2.评分值仍根据文献报道该指标在预测前庭中枢性眩晕的特殊性而设定,尚未经临床验证。
3.评分(score):=5:警惕高危中枢性眩晕(警惕风险);
≥6:高危中枢性眩晕(危险预警)。表 9 急性前庭综合征常见/部分少见眩晕疾病基于病机和受累部位的关键临床特征、诊断指征及鉴别要领
AVS
分层眩晕疾病 病因病机 主要受累部位 临床特征 诊断指征 鉴别要领 急性前庭中枢性眩晕 脑缺血性梗死 椎基底动脉小血管狭窄闭塞脑组织缺血性坏死:心脑血管危险因素 脑干,小脑 1.自发性
2.起病稍缓,常在安静状态发病,症状逐步出现
3.急性前庭综合征
4.部分患者有局灶性神经功能缺损表现(Wallenberg综合征全部或部分表现)
5.严重者发展为小脑水肿,出现脑干受压、小脑疝相应表现一、临床表现
1.急性前庭综合征
2.局灶神经受累症状
3.眼动异常征
4.小脑征(共济障碍和严重平衡障碍)
5.严重者意识障碍,昏迷甚至死亡
二、诊断
1.脑梗死:影像检查(MRI、MRA、CTA)确诊
2.脑出血:CT/MRI常呈孤立性眩晕表现
1.PICA供血区梗死:可模拟前庭神经病变(假性前庭神经炎)。
鉴别要领:除同左特征外,自发性眼震无固视抑制、且vHIT检查阴性,可鉴别。
2.AICA供血区梗死:可出现感音神经性听力下降,且vHIT检查阳性,模拟迷路炎(突发性感音神经听力下降),鉴别要领:同左
小脑和脑干出血常伴多脑神经受损症状,进展迅速,甚至昏迷或死亡小脑/脑干出血 脑血管破裂出血,脑组织受压,
缺血、坏死;
高血压
动脉硬化
凝血机制异常等心脏血管危险因素脑干,小脑 1.自发性
2.起病急骤
3.突发急性前庭综合征常伴头痛,颈部痛。和其他神经症状
4.小范围出血常类似脑缺血性梗死综合征(同上)
5.小脑出血常表现为眩晕,呕吐,头痛和不能站立和行走
6.脑桥大出血可出现肢体瘫痪,去大脑强直,针尖样瞳孔,意识障碍多发性硬化 病因不明
中枢神经脱髓鞘病变个体差异大:
前庭神经根
听神经
前庭神经核
小脑柄
小脑
脑干
椎体束等1.流行病学特征:中青年15~50岁(或30~50岁);女性大于男性
2. 临床特征:
(1)自发性
(2)个体差异大,取决于病变部位及病因:
1)眩晕:持续数小时、数天~数周;伴呕吐,平衡障碍
2)可伴突聋(突聋伴眩晕)
3)眼震;常出现。可呈外周性或中枢性需结合病史,临床表现和MRI检查综合诊断
一、临床表现
1.常有视神经炎病史
2.眩晕和/或小脑征
3.异常眼征
4.听觉、视觉或体感神经诱发电位潜伏期延长
二、诊断
1.MRI检查诊断
(造影可评估炎症活动进程)
2. 脑脊液生化,分子生物学或免疫学检查1.常呈孤立性眩晕,伴/不伴自发性眼震
(1)选择性前庭神经核受累时,可模拟前庭神经炎,但自发性眼震无固视抑制
(2)累及听神经时可模拟突发性感音神经性耳聋
2.常见异常眼征:
(1)核间性眼肌麻痹(INO):内侧纵束受损,出现单眼外展受限,另一侧眼分离性凝视性眼震;
(2)获得性钟摆样眼震(Acquired pendular nystagmus)Wernicke综合征 硫胺素缺乏
诱因:
酗酒
减肥手术
妊娠呕吐
长期饥饿
吸收障碍综合征/长期肠外营养(喂养)。化疗,甲亢,尿毒症,糖尿病,胰岛素缺乏(硫胺素经小肠转运减少而易感)丘脑内侧
乳头体(mammillary bodies)
前庭神经核1.自发性
2.常对称性双侧VOR异常
3.常呈外周性和中枢性混合性前庭损伤
4.眩晕不常见,早期常平衡失调和跌倒一、临床表现
1. 急性或亚急性“三联征”或“四联征”
(1)眼肌麻痹
(2)共济失调:躯干共济失调比肢体共济失调更严重
(3)脑病
(4)认知改变(90%)
2.眼动异常征
二、诊断
1.MRI(FLAIR和T2权重影像)
2.诊断性治疗1.前庭内侧核病变
常表现为中枢性和双侧外周前庭疾病(假性双侧前庭神经炎:双侧vHIT阳性)
鉴别:GEN阳性
2.脑桥网状结构损伤:Saccade异常
外侧脑桥核:Smooth Pursuit异常
3.共济失调和健忘症是长期表现小脑脑桥角肿瘤
后颅窝肿瘤前庭神经鞘膜瘤
脑膜瘤
转移瘤
其他良恶性肿瘤/非肿瘤占位病变前庭神经
听神经
小脑
脑干1.自发性
2.单侧渐进性听力损失、耳鸣和共济失调
3.约10% 以突发性听力下降为首发症状,有时伴眩晕
4.肿瘤压迫出现小脑与脑干症状一、临床表现:
1.单侧渐进性听力下降、耳鸣、共济失调
2.约10%以突发性听力下降为首发症状,有时伴眩晕
3.Brun's眼震(前庭外周性眼震伴凝视麻痹性眼震),vHIT阳性,半规管轻瘫,VEMP异常
4.局部神经受累症状
5.可伴头痛
二、诊断
小脑脑桥角MRI钆造影根据肿瘤部位和大小,表现复杂:
1.可表现为外周性前庭功能损害,伴/不伴中枢性前庭功能障碍
2.可出现双侧前庭功能障碍
3.可出现小脑和脑干功能障碍脑外伤 脑、颈部外伤(钝击伤) 颅脑
颈部1.诱(引)发性
2.孤立性眩晕
3.伴或不伴听力损害及其他神经症状一、脑外伤史
二、临床表现
1.孤立性眩晕
2.伴或不伴听力损害及其他神经症状
三、颅脑影像学检查
1.颅脑CT
2.MRI1.前庭中枢或前庭外周损伤
2.前庭中枢和前庭外周混合性损伤甲硝唑中毒性脑病 药物中毒
机制不清,可能与硫胺素通路障碍有关小脑/脑干诱(引)发性损伤(类似Wernicke综合征) 双侧VOR异常及GEN(类似Wernicke综合征) 一、用药史
二、临床表现
1.双侧半规管轻瘫
2.双侧HIT异常
3.凝视性眼震(GEN)
三、颅脑影像学检查:MRI1.前庭中枢损伤
或:
2.前庭中枢和前庭外周混合性损伤急性前庭外周性眩晕 前庭神经炎 病毒感染 前庭神经(急性单侧前庭病) 1.急性眩晕发作,持续数日
2.常伴急性前庭综合征其他症状:恶心呕吐,振动幻视,平衡障碍(尚可站立或行走)
3.无听力下降1.急性前庭综合征
2.无听力下降
3.前庭外周性眼震特征
4.vHIT阳性
5.排除其他前庭疾病1.急性发作眩晕,数小时内眩晕症状达到高峰,持续数日
2.需鉴别孤立性中枢性眩晕,尤其是假性前庭神经炎(PICA梗死)鉴别:后者①有中枢眼动征及小脑征(无扶助,不可站立或行走);②vHIT阴性
3.影像诊断鉴别MRI检查特发性突聋伴眩晕
(ISSNHLwV或ISHLwV)原因不明:
1.病毒感染学
2.微循环障碍学说(迷路卒中)内耳迷路 1.急性眩晕发作
2.伴突发性听力下降、耳鸣
3.可伴前庭综合征其他症状(尚可站立或行走)
4.前庭外周性眼震特征1.72 h内感音神经性听力下降,3个相连频率下降≥30 dB
2.伴眩晕及其他前庭神经症状
3.前庭外周性眼震特征
4.vHIT阳性
5.排除其他前庭、耳蜗及中枢疾病1.与中枢性假性迷路炎(AICA梗死)鉴别(两者常有vHIT阳性):AICA梗死可出现中枢性眼动特征及小脑征(无扶助,不可站立或行走)
2.需排除小脑脑桥角-内听道占位性病变后方可确诊:MRI增强前庭神经鞘膜瘤(听神经瘤) 肿瘤 前庭神经及听神经 1.多呈渐进性发展,早期主要表现为耳鸣,隐匿性平衡功能障碍
2.约10%以突发性感音神经性聋为首发症状
3.根据肿瘤大小可伴有轻度到中重度平衡障碍1.感音神经性听力下降
2.HIT/VEMP检查阳性
3.影像检查:MRI增强检查小脑脑桥角-内听道突发性感音神经性聋约1%为听神经瘤,需注意鉴别 细菌性迷路炎 细菌感染 内耳迷路 1.常有慢性化脓性中耳炎急性发作史
2.眩晕伴听力下降
3.严重者可伴其他颞骨内外并发症1.中耳炎病史
2.耳部检查:
慢性化脓性中耳炎(活动期)体征:鼓膜穿孔,中耳鼓室脓性分泌物
3.瘘管征(静止期):鼓室鼓气耳镜加压可引起眩晕
4.颞骨CT:中耳乳突阴影、骨质破坏等(常可见外半规管骨质破坏)1.中耳胆脂瘤伴中耳感染时,可发生其他颞骨并发症(如面瘫)
2.严重者可伴颅内外并发症(如乙状窦血栓性静脉炎、脑脓肿等)耳毒性药物(氨基糖苷类)中毒 药物中毒 内耳毛细胞(前庭、耳蜗)及第Ⅷ对脑神经(前庭神经-耳蜗神经) 前庭外周性病变:
1.渐进性/急性眩晕发作,持续数日至数周
2.常伴听力下降1.耳毒性药物(氨基糖苷类)用药史(全身或者耳局部)
2.眩晕伴不同程度听力下降
3.前庭功能检查异常
4.排除其他前庭性疾病1.前庭外周性病变特征:
HIT阳性,半规管轻瘫,VEMP异常等
2.常有感音神经性听力损失迷路震荡 颅脑闭合伤致内耳膜迷路结构受损 内耳迷路(耳蜗和前庭结构) 1.脑外伤病史或航空或深潜水史
2.突然发生的眩晕伴耳聋、耳鸣、平衡障碍
3.听力学及前庭功能检查异常1.脑外伤病史或航空或深潜水史
2.前庭外周和/或前庭中枢损伤临床表现
3.前庭功能和听力学检查异常
4.影像学检查可有异常头部钝击伤可引起前庭中枢和前庭外周孤立损伤或复合损伤 头部钝击伤,航空或深潜水等惯性或压力损伤 脑震荡常伴迷路震荡 内耳迷路(耳蜗和前庭结构)、第Ⅷ脑神经、脑干等 注:根据文献4、11、12、19~22、32、34、42~44、46、47、49、50、54~61、63~71编制。 -
[1] Bisdorff AR, Staab JP, Newman-Toker DE. Overview of the international classification of vestibular disorders[J]. Neurol Clin, 2015, 33(3): 541-550, vii.
[2] 孔维佳. 眩晕疾病的SCD程序式诊断策略及诊断路径[J]. 临床耳鼻咽喉头颈外科杂志, 2024, 38(11): 985-1000. https://lceh.whuhzzs.com/article/doi/10.13201/j.issn.2096-7993.2024.11.001
[3] Tarnutzer AA, Berkowitz AL, Robinson KA, et al. Does my dizzy patient have a stroke? A systematic review of bedside diagnosis in acute vestibular syndrome[J]. CMAJ, 2011, 183(9): E571-592. doi: 10.1503/cmaj.100174
[4] Edlow JA, Carpenter C, Akhter M, et al. Guidelines for reasonable and appropriate care in the emergency department 3(GRACE-3): Acute dizziness and Vertigo in the emergency department[J]. Acad Emerg Med, 2023, 30(5): 442-486.
[5] Hotson JR, Baloh RW. Acute vestibular syndrome[J]. N Engl J Med, 1998, 339(10): 680-685.
[6] Newman-Toker DE, Hsieh YH, Camargo CA, et al. Spectrum of dizziness visits to US emergency departments: cross-sectional analysis from a nationally representative sample[J]. Mayo Clin Proc, 2008, 83(7): 765-775. doi: 10.4065/83.7.765
[7] Neuhauser HK, von Brevern M, Radtke A, et al. Epidemiology of vestibular Vertigo: a neurotologic survey of the general population[J]. Neurology, 2005, 65(6): 898-904. doi: 10.1212/01.wnl.0000175987.59991.3d
[8] Royl G, Ploner CJ, Leithner C. Dizziness in the emergency room: diagnoses and misdiagnoses[J]. Eur Neurol, 2011, 66(5): 256-263. doi: 10.1159/000331046
[9] Kerber KA, Meurer WJ, Brown DL, et al. Stroke risk stratification in acute dizziness presentations: a prospective imaging-based study[J]. Neurology, 2015, 85(21): 1869-1878.
[10] Comolli L, Korda A, Zamaro E, et al. Vestibular syndromes, diagnosis and diagnostic errors in patients with dizziness presenting to the emergency department: a cross-sectional study[J]. BMJ Open, 2023, 13(3): e064057.
[11] Edlow JA. Diagnosing patients with acute-onset persistent dizziness[J]. Ann Emerg Med, 2018, 71(5): 625-631.
[12] Choi KD, Lee H, Kim JS. Ischemic syndromes causing dizziness and Vertigo[J]. Handb Clin Neurol, 2016, 137: 317-340.
[13] Steenerson KK. Acute Vestibular Syndrome[J]. Continuum(Minneap Minn), 2021, 27(2): 402-419.
[14] Kerber KA, Brown DL, Lisabeth LD, et al. Stroke among patients with dizziness, vertigo, and imbalance in the emergency department: a population-based study[J]. Stroke, 2006, 37(10): 2484-2487.
[15] Newman-Toker DE, Edlow JA. TiTrATE: A Novel, Evidence-Based Approach to Diagnosing Acute Dizziness and Vertigo[J]. Neurol Clin, 2015, 33(3): 577-599. doi: 10.1016/j.ncl.2015.04.011
[16] Gurley KL, Edlow JA. Acute dizziness[J]. Semin Neurol, 2019, 39(1): 27-40. doi: 10.1055/s-0038-1676857
[17] Navi BB, Kamel H, Shah MP, et al. Application of the ABCD2 score to identify cerebrovascular causes of dizziness in the emergency department[J]. Stroke, 2012, 43(6): 1484-1489. doi: 10.1161/STROKEAHA.111.646414
[18] Kuroda R, Nakada T, Ojima T, et al. The TriAGe+ Score for Vertigo or Dizziness: A Diagnostic Model for Stroke in the Emergency Department[J]. J Stroke Cerebrovasc Dis, 2017, 26(5): 1144-1153. doi: 10.1016/j.jstrokecerebrovasdis.2017.01.009
[19] Kattah JC, Talkad AV, Wang DZ, et al. HINTS to diagnose stroke in the acute vestibular syndrome: three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging[J]. Stroke, 2009, 40(11): 3504-3510. doi: 10.1161/STROKEAHA.109.551234
[20] Newman-Toker DE, Kerber KA, Hsieh YH, et al. HINTS outperforms ABCD2 to screen for stroke in acute continuous Vertigo and dizziness[J]. Acad Emerg Med, 2013, 20(10): 986-996. doi: 10.1111/acem.12223
[21] Vanni S, Pecci R, Casati C, et al. STANDING, a four-step bedside algorithm for differential diagnosis of acute vertigo in the Emergency Department[J]. Acta Otorhinolaryngol Ital, 2014, 34(6): 419-426.
[22] Vanni S, Pecci R, Edlow JA, et al. Differential Diagnosis of Vertigo in the Emergency Department: A Prospective Validation Study of the STANDING Algorithm[J]. Front Neurol, 2017, 8: 590. doi: 10.3389/fneur.2017.00590
[23] Lee H, Sohn SI, Cho YW, et al. Cerebellar infarction presenting isolated Vertigo: frequency and vascular topographical patterns[J]. Neurology, 2006, 67(7): 1178-1183.
[24] Choi SY, Kim HJ, Kim JS. Chasing dizzy Chimera: Diagnosis of combined peripheral and central vestibulopathy[J]. J Neurol Sci, 2016, 371: 69-78.
[25] Huh YE, Koo JW, Lee H, et al. Head-shaking aids in the diagnosis of acute audiovestibular loss due to anterior inferior cerebellar artery infarction[J]. Audiol Neurootol, 2013, 18(2): 114-124. doi: 10.1159/000345643
[26] Chalela JA, Kidwell CS, Nentwich LM, et al. Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison[J]. Lancet, 2007, 369(9558): 293-298. doi: 10.1016/S0140-6736(07)60151-2
[27] Saber Tehrani AS, Kattah JC, Kerber KA, et al. Diagnosing stroke in acute dizziness and Vertigo: pitfalls and pearls[J]. Stroke, 2018, 49(3): 788-795. doi: 10.1161/STROKEAHA.117.016979
[28] Choi KD, Kim JS. Vascular Vertigo: updates[J]. J Neurol, 2019, 266(8): 1835-1843. doi: 10.1007/s00415-018-9040-3
[29] Voetsch B, Sehgal S. Acute dizziness, Vertigo, and unsteadiness[J]. Neurol Clin, 2021, 39(2): 373-389.
[30] Saber Tehrani AS, Coughlan D, Hsieh YH, et al. Rising annual costs of dizziness presentations to U.S. emergency departments[J]. Acad Emerg Med, 2013, 20(7): 689-696.
[31] Newman-Toker DE. Missed stroke in acute Vertigo and dizziness: It is time for action, not debate[J]. Ann Neurol, 2016, 79(1): 27-31.
[32] Zwergal A, Dieterich M. Vertigo and dizziness in the emergency room[J]. Curr Opin Neurol, 2020, 33(1): 117-125.
[33] Bisdorff A, Von Brevern M, Lempert T, et al. Classification of vestibular symptoms: towards an international classification of vestibular disorders[J]. J Vestib Res, 2009, 19(1-2): 1-13. doi: 10.3233/VES-2009-0343
[34] Bennett M. The vertigo case history[M]//Jocobson GP, Shepard NT. Balance function assessment and management. Plural Publishing, 2008: 45-62.
[35] Hanley K, O'Dowd T. Symptoms of Vertigo in general practice: a prospective study of diagnosis[J]. Br J Gen Pract, 2002, 52(483): 809-812.
[36] Chan Y. Differential diagnosis of dizziness[J]. Curr Opin Otolaryngol Head Neck Surg, 2009, 17(3): 200-203. doi: 10.1097/MOO.0b013e32832b2594
[37] Post RE, Dickerson LM. Dizziness: a diagnostic approach[J]. Am Fam Physician, 2010, 82(4): 361-369.
[38] Wu V, Beyea MM, Simpson MT, et al. Standardizing your approach to dizziness and Vertigo[J]. J Fam Pract, 2018, 67(8): 490-498.
[39] Rosengren SM, Young AS, Taylor RL, et al. Vestibular function testing in the 21st century: video head impulse test, vestibular evoked myogenic potential, video nystagmography; which tests will provide answers?[J]. Curr Opin Neurol, 2022, 35(1): 64-74. doi: 10.1097/WCO.0000000000001023
[40] Zwergal A, Feil K, Schniepp R, et al. Cerebellar dizziness and Vertigo: etiologies, diagnostic assessment, and treatment[J]. Semin Neurol, 2020, 40(1): 87-96.
[41] Newman-Toker DE, Kattah JC, Alvernia JE, et al. Normal head impulse test differentiates acute cerebellar strokes from vestibular neuritis[J]. Neurology, 2008, 70(24 Pt 2): 2378-2385.
[42] Shah VP, Oliveira J E Silva L, Farah W, et al. Diagnostic accuracy of the physical examination in emergency department patients with acute Vertigo or dizziness: a systematic review and meta-analysis for GRACE-3[J]. Acad Emerg Med, 2023, 30(5): 552-578.
[43] Ishiyama G and Ishiyama A. Central vestibular disorders[M]//Johnson JT and Rosen CA eds. Bailey's Head & Neck Surgery-Otolaryngology. 5th ed. Pniladelphia, 2014, Vol. 2: 2717-2732.
[44] Eggers SD. Z, Zee DS. Central vestibular disorders[M]//Cummings CW, Flint PW, Harker LA, et al eds. Cummings Otolaryngology-Head and Neck Surgery. 4th ed. Elsevier Mosby, 2015, Vol4: 3254-3289.
[45] Goebel JA, White, JA, Heidenreich, KD. Evaluation of the Vestibular System[M]//Wackym PA, Snow JB, JR. Ballenger's Otorhinolaryngology head and neck surgery. People's Medical Publishing House-USA, 2016: 137-151.
[46] Karatas M. Central Vertigo and dizziness: epidemiology, differential diagnosis, and common causes[J]. Neurologist, 2008, 14(6): 355-364.
[47] Choi JY, Kim JS. Nystagmus and central vestibular disorders[J]. Curr Opin Neurol, 2017, 30(1): 98-106.
[48] Cnyrim CD, Newman-Toker D, Karch C, et al. Bedside differentiation of vestibular neuritis from central"vestibular pseudoneuritis"[J]. J Neurol Neurosurg Psychiatry, 2008, 79(4): 458-460.
[49] Brandt T, Strupp M, Dieterich M. Five keys for diagnosing most Vertigo, dizziness, and imbalance syndromes: an expert opinion[J]. J Neurol, 2014, 261(1): 229-231.
[50] Walther LE. Current diagnostic procedures for diagnosing Vertigo and dizziness[J]. GMS Curr Top Otorhinolaryngol Head Neck Surg, 2017, 16: Doc02.
[51] Carmona S, Martínez C, Zalazar G, et al. The diagnostic accuracy of truncal Ataxia and HINTS as cardinal signs for acute vestibular syndrome[J]. Front Neurol, 2016, 7: 125.
[52] Gerlier C, Hoarau M, Fels A, et al. Differentiating central from peripheral causes of acute Vertigo in an emergency setting with the HINTS, STANDING, and ABCD2 tests: a diagnostic cohort study[J]. Acad Emerg Med, 2021, 28(12): 1368-1378.
[53] Edlow JA. Distinguishing peripheral from central causes of dizziness and Vertigo without using HINTS or STANDING[J]. J Emerg Med, 2024, 67(6): e622-e633.
[54] Strupp M, Bisdorff A, Furman J, et al. Acute unilateral vestibulopathy/vestibular neuritis: Diagnostic criteria[J]. J Vestib Res, 2022, 32(5): 389-406.
[55] Lempert T, Olesen J, Furman J, et al. Vestibular migraine: diagnostic criteria1[J]. J Vestib Res, 2022, 32(1): 1-6.
[56] Chandrasekhar SS, Tsai Do BS, Schwartz SR, et al. Clinical Practice Guideline: Sudden Hearing Loss(Update)[J]. Otolaryngol Head Neck Surg, 2019, 161(1_suppl): S1-S45.
[57] Kitoh R, Nishio SY, Sato H, et al. Clinical practice guidelines for the diagnosis and management of acute sensorineural hearing loss[J]. Auris Nasus Larynx, 2024, 51(4): 811-821.
[58] Strupp M, Dieterich M, Brandt T. The treatment and natural course of peripheral and central vertigo[J]. Dtsch Arztebl Int, 2013, 110(29-30): 505-516.
[59] Brandt T, Dieterich M. The dizzy patient: don't forget disorders of the central vestibular system[J]. Nat Rev Neurol, 2017, 13(6): 352-362.
[60] Strupp M, Dlugaiczyk J, Ertl-Wagner BB, et al. Vestibular disorders[J]. Dtsch Arztebl Int, 2020, 117(17): 300-310.
[61] Kim HJ, Lee JO, Choi JY, et al. Etiologic distribution of dizziness and Vertigo in a referral-based dizziness clinic in South Korea[J]. J Neurol, 2020, 267(8): 2252-2259.
[62] 孔维佳, 周梁. 耳鼻咽喉头颈外科学[M]. 3版. 北京: 人民卫生出版社, 2015: 190-202.
[63] Kim SH, Kim HJ, Kim JS. Isolated vestibular syndromes due to brainstem and cerebellar lesions[J]. J Neurol, 2017, 264(Suppl 1): 63-69.
[64] Choi JY, Lee SH, Kim JS. Central Vertigo[J]. Curr Opin Neurol, 2018, 31(1): 81-89.
[65] Pellegrino N, Di Stefano V, Rotondo E, et al. Neurological Vertigo in the emergency room in pediatric and adult age: systematic literature review and proposal for a diagnostic algorithm[J]. Ital J Pediatr, 2022, 48(1): 125.
[66] Kattah JC, Dhanani SS, Pula JH, et al. Vestibular signs of thiamine deficiency during the early phase of suspected Wernicke encephalopathy[J]. Neurol Clin Pract, 2013, 3(6): 460-468.
[67] Akdal G, MacDougall HG, Chen L, et al. Selective impairment of horizontal vestibulo-ocular reflexes in acute Wernicke's encephalopathy[J]. J Neurol Sci, 2016, 365: 167-168.
[68] Kim E, Na DG, Kim EY, et al. MR imaging of metronidazole-induced encephalopathy: lesion distribution and diffusion-weighted imaging findings[J]. AJNR Am J Neuroradiol, 2007, 28(9): 1652-1658.
[69] Lee SU, Jung IE, Kim HJ, et al. Metronidazole-induced combined peripheral and central vestibulopathy[J]. J Neurol Sci, 2016, 365: 31-33.
[70] Kim HJ, Park SH, Kim JS, et al. Bilaterally abnormal head impulse tests indicate a large cerebellopontine angle tumor[J]. J Clin Neurol, 2016, 12(1): 65-74.
[71] Lee H. Audiovestibular loss in anterior inferior cerebellar artery territory infarction: a window to early detection?[J]. J Neurol Sci, 2012, 313(1-2): 153-159.
[72] Muncie HL, Sirmans SM, James E. Dizziness: approach to evaluation and management[J]. Am Fam Physician, 2017, 95(3): 154-162.
[73] Machner B, Choi JH, Trillenberg P, et al. Risk of acute brain lesions in dizzy patients presenting to the emergency room: who needs imaging and who does not?[J]. J Neurol, 2020, 267(Suppl 1): 126-135.
[74] 中华医学会, 中华医学会杂志社, 中华医学会全科医学分会, 等. 头晕/眩晕基层诊疗指南(2019年)[J]. 中华全科医师杂志, 2020, 19(3): 201-216.
[75] Filippopulos FM, Strobl R, Belanovic B, et al. Validation of a comprehensive diagnostic algorithm for patients with acute Vertigo and dizziness[J]. Eur J Neurol, 2022, 29(10): 3092-3101.
-

计量
- 文章访问数: 340
- 施引文献: 0



 下载:
下载: