Analyzing the reasons for and prevention of serious complications after general anesthesia in children with obstructive sleep apnea
-
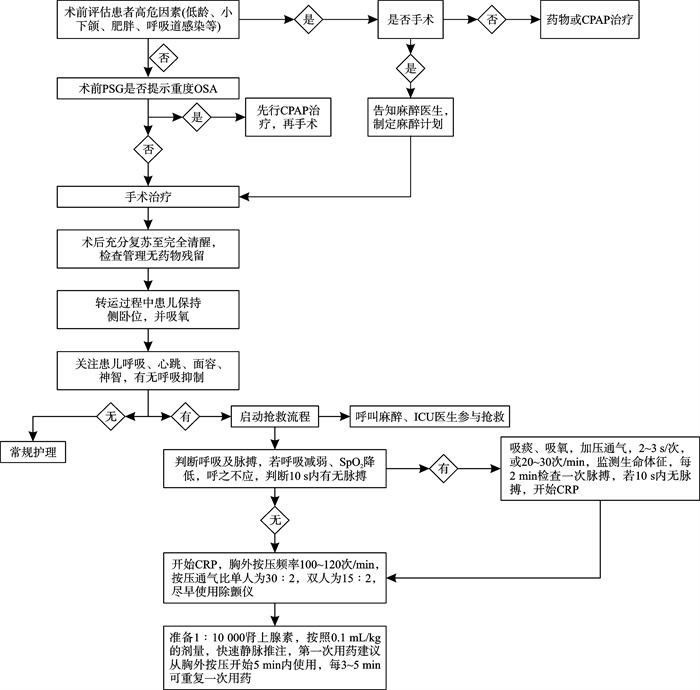
摘要: 目的 探讨儿童阻塞性睡眠呼吸暂停(obstructive sleep apnea,OSA)全身麻醉手术后呼吸暂停发生的原因及预防措施,提高OSA全身麻醉手术的安全性。方法 回顾性分析2020年3月—2022年3月南方医科大学深圳医院发生的4例OSA患儿全身麻醉手术后呼吸心搏骤停事件的临床及随访资料。结果 4例OSA患儿全身麻醉术后出现不同程度的血氧饱和度下降、发绀、意识丧失,其中1例出现呼吸心搏骤停。经过吸氧、吸痰、加压通气、唤醒及心肺复苏等措施积极抢救,4例患儿均转危为安。术后随访2~6个月,患儿均无并发症发生。术后呼吸暂停发生的主要原因可能包括麻醉药物残留、OSA疾病的特性以及儿童群体的特殊性。结论 儿童OSA全身麻醉手术后需密切关注患儿生命体征,若出现呼吸抑制,应积极抢救,避免出现严重后果。Abstract: Objective To explore the causes and preventive measures of respiratory arrest following general anesthesia in children with obstructive sleep apnea (OSA), in order to enhance the safety of OSA surgeries under general anesthesia.Methods A retrospective analysis was conducted on the clinical and follow-up data of four pediatric cases that experienced respiratory arrest after general anesthesia for OSA at Shenzhen Hospital of Southern Medical University from March 2020 to March 2022.Results All four children exhibited varying degrees of decreased blood oxygen saturation, cyanosis, and loss of consciousness after OSA surgery under general anesthesia, with one case experiencing respiratory and cardiac arrest. Through emergency rescue measures such as oxygen supplementation, suctioning, positive pressure ventilation, awakening, and cardiopulmonary resuscitation, all four children were stabilized. Follow-up after 2 to 6 months showed no complications. The main reasons for the occurrence are analyzed as: residual anesthetic drugs, characteristics of the OSA disease, and the unique aspects of the pediatric population.Conclusion Children undergoing general anesthesia for OSA should be closely monitored for vital signs after surgery. If respiratory suppression occurs, active rescue measures should be taken to avoid serious consequences.
-
Key words:
- obstructive sleep apnea /
- respiratory depression /
- cardiac arrest /
- anesthesia recovery
-

-
表 1 4例OSA术后发生呼吸心跳意外事件的患儿基本信息及抢救情况
例序 性别 年龄 体重/kg 手术名称 呕吐误吸 气管痉挛 手术时长/min 复苏时长/min 复苏结束/min 表现 抢救措施 预后 1 男 3岁
12个月15.1 扁桃体伴腺样体切除术 无 无 23 20 5 呼之不应,口唇发绀,SpO2 72% 侧卧、吸痰、高流量吸氧 良好 2 女 3岁
7个月13.6 腺样体切除术 无 无 20 28 1 口唇发绀、面色苍白、呼之不应,SpO2 84% 侧卧、吸痰、高流量吸氧 良好 3 女 8岁
2个月19.3 扁桃体伴腺样体切除术 无 无 29 46 1 嗜睡,面唇发绀,心音偏低,SpO2 87% 侧卧、吸痰、吸氧无好转,球囊面罩通气 良好 4 男 3岁
7个月14.6 扁桃体伴腺样切除术+鼓膜置管术 无 无 32 27 9 颜面青紫、意识及自主呼吸丧失,SpO2 31%,颈动脉搏动不明显 持续胸外按压、吸痰、球囊面罩通气、补液 良好 -
[1] 邓哲, 王桂香, 侯钰玮, 等. 出生体重与儿童阻塞性睡眠呼吸暂停关系的研究[J]. 临床耳鼻咽喉头颈外科杂志, 2024, 38(3): 230-234. doi: 10.13201/j.issn.2096-7993.2024.03.010
[2] Springford LR, Griffiths M, Bajaj Y. Management of paediatric sleep-disordered breathing[J]. Br J Hosp Med(Lond), 2024, 85(2): 1-6.
[3] 中国医师协会耳鼻咽喉头颈外科医师分会, 儿童扁桃体腺样体低温等离子射频消融术规范化治疗临床实践指南[J]. 临床耳鼻咽喉头颈外科杂志, 2021, 35(3): 193-199. doi: 10.13201/j.issn.2096-7993.2021.03.001
[4] 李妮吉娜, 刘雁. 麻醉复苏期患者呼吸道的管理[J]. 当代护士(中旬刊), 2016, 11: 99-101.
[5] von Ungern-Sternberg BS. Respiratory complications in the pediatric postanesthesia care unit[J]. Anesthesiol Clin, 2014, 32(1): 45-61. doi: 10.1016/j.anclin.2013.10.004
[6] Karcz M, Papadakos PJ. Respiratory complications in the postanesthesia care unit: A review of pathophysiological mechanisms[J]. Can J Respir Ther, 2013, 49(4): 21-29.
[7] Bateman JT, Saunders SE, Levitt ES. Understanding and countering opioid-induced respiratory depression[J]. Br J Pharmacol, 2023, 180(7): 813-828. doi: 10.1111/bph.15580
[8] Dahan A, Yassen A, Bijl H, et al. Comparison of the respiratory effects of intravenous buprenorphine and fentanyl in humans and rats[J]. Br J Anaesth, 2005, 94(6): 825-834. doi: 10.1093/bja/aei145
[9] Boom M, Niesters M, Sarton E, et al. Non-analgesic effects of opioids: opioid-induced respiratory depression[J]. Curr Pharm Des, 2012, 18(37): 5994-6004. doi: 10.2174/138161212803582469
[10] Chaudhry RA, Zarmer L, West K, et al. Obstructive Sleep Apnea and Risk of Postoperative Complications after Non-Cardiac Surgery[J]. J Clin Med, 2024, 13(9): 2538. doi: 10.3390/jcm13092538
[11] Thilen SR, Weigel WA, Todd MM, et al. 2023 American Society of Anesthesiologists Practice Guidelines for Monitoring and Antagonism of Neuromuscular Blockade: A Report by the American Society of Anesthesiologists Task Force on Neuromuscular Blockade[J]. Anesthesiology, 2023, 138(1): 13-41. doi: 10.1097/ALN.0000000000004379
[12] Hill CA, Litvak A, Canapari C, et al. A pilot study to identify pre-and peri-operative risk factors for airway complications following adenotonsillectomy for treatment of severe pediatric OSA[J]. Int J Pediatr Otorhinolaryngol, 2011, 75(11): 1385-1390. doi: 10.1016/j.ijporl.2011.07.034
[13] Belyea J, Chang Y, Rigby MH, et al. Post-tonsillectomy complications in children less than three years of age: a case-control study[J]. Int J Pediatr Otorhinolaryngol, 2014, 78(5): 871-874. doi: 10.1016/j.ijporl.2014.02.029
[14] 刘华平, 胡怀成, 许明华. 小儿阻塞性睡眠呼吸暂停综合征的麻醉处理体会[J]. 临床麻醉学杂志, 2007, 23(3): 253-253. doi: 10.3969/j.issn.1004-5805.2007.03.035
[15] 周益人, 姜燕, 金泉英. 琥珀胆碱致患儿呼吸恢复延迟一例[J]. 临床麻醉学杂志, 2013, 29(7): 715-715.
[16] Subramani Y, Nagappa M, Wong J, et al. Death or near-death in patients with obstructive sleep apnoea: a compendium of case reports of critical complications[J]. Br J Anaesth, 2017, 119(5): 885-899. doi: 10.1093/bja/aex341
[17] Saur JS, Brietzke SE. Polysomnography results versus clinical factors to predict post-operative respiratory complications following pediatric adenotonsillectomy[J]. Int J Pediatr Otorhinolaryngol, 2017, 98: 136-142. doi: 10.1016/j.ijporl.2017.05.004
[18] 胡巧, 蒋丽丹, 唐凤娇. 全身麻醉患儿麻醉苏醒期呼吸抑制影响因素分析及预防护理[J]. 齐鲁护理杂志, 2021, 27(14): 38-40.
[19] 张恩琴, 张鑫, 樊荣. 静脉注射硫酸镁预防儿童腺样体扁桃体切术后喉痉挛及咳嗽的临床效果分析[J]. 儿科药学杂志, 2017, 23(8): 18-20.
[20] Topjian AA, Raymond TT, Atkins D, et al. Pediatric Basic and Advanced Life Support Collaborators. Part 4: Pediatric Basic and Advanced Life Support 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care[J]. Pediatrics, 2021, 147(Suppl 1): e2020038505D.
-




 下载:
下载: