A retrospective analysis of the clinical characteristics of 63 patients with vestibular neuritis
-
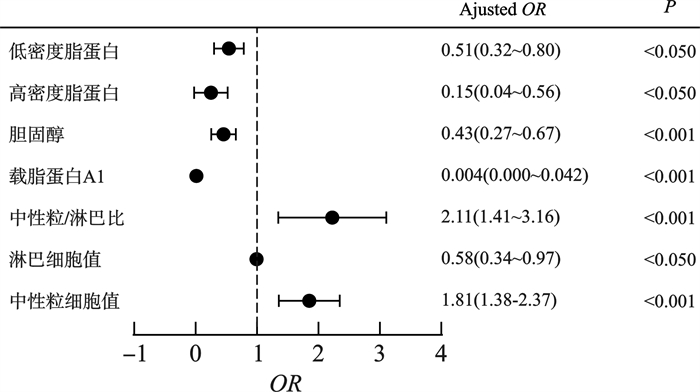
摘要: 目的 回顾性分析63例前庭神经炎患者听觉及前庭功能检查、实验室检查结果并分析其特点。方法 收集2012年10月至2022年12月在中山大学附属第三医院耳鼻咽喉头颈外科住院治疗的资料完整的前庭神经炎患者63例,均符合2022年Bárány协会前庭神经炎的诊断标准,总结纯音测听、耳蜗电图、视频眼震图、双温实验、颈肌前庭诱发肌源性电位(cVEMP)、眼肌前庭诱发肌源性电位(oVEMP)、视频头脉冲试验(vHIT)完成比及异常比。选取年龄性别匹配的体检中心健康体检者63例为对照组,比较2组间血炎症指标及脂代谢指标是否存在差异。结果 前庭神经炎患者纯音测听双耳听力正常50例,双侧高频感音神经性听力下降8例,单侧轻度高频感音神经性听力下降5例。耳蜗电图完成56例,其中双耳-SP/AP幅值比≥0.4为3例,单耳幅值比≥0.4为5例。双温试验完成为55例,且55例CP值均大于30%。vHIT完成30例。cVEMP完成46例,oVEMP完成22例。4项前庭功能检查全部完成17例。可判断损伤范围的患者49例,其中单侧前庭上神经损伤27例,单侧前庭上、下神经损伤21例,单侧前庭下神经损伤1例。前庭神经炎患者血中性粒细胞值(P < 0.001)、淋巴细胞值(P < 0.005)、中性粒/淋巴细胞比值(P < 0.001)、载脂蛋白A1(P < 0.001)、胆固醇(P < 0.001)、高密度脂蛋白(P < 0.01)、低密度脂蛋白(P < 0.01)与对照组比较差异有统计学意义。炎症指标是前庭神经炎患者的危险性因素,OR值分别为中性粒细胞值1.81(1.38~2.37,P < 0.001)、血中性粒/淋巴细胞比值2.11(1.41~3.16,P < 0.001),载脂蛋白A1是前庭神经炎患者的保护性因素,OR值为0.004(0.001~0.042,P < 0.001)。结论 部分前庭神经炎患者耳蜗电图结果异常,可能提示患者存在隐性听力损失。中性粒细胞值、淋巴细胞值、血中性粒/淋巴细胞比值、载脂蛋白A1、与前庭神经炎发病相关。其中中性粒细胞值、血中性粒/淋巴细胞比值是发病的危险因素。Abstract: Objective To retrospectively analyze the results of auditory examination, vestibular function examination and laboratory examination of 63 patients diagnosed as vestibular neuritis.Methods A total of 63 patients diagnosed with vestibular neuritis hospitalized in the Department of Otolaryngology, Head and Neck Surgery of the Third Affiliated Hospital of Sun Yat-sen University, from October 2012 to December 2022 were recruited. All patients met the diagnostic criteria for the 2022 Bárány association vestibular neuritis. Clinical data and the results of pure tone audiometry, electrocochleogram, video electronystagmogram, caloric test, cervical vestibuloevoked myogenic potential(cVEMP), ocular vestibuloevoked myogenic potential(oVEMP), video head impulse test(vHIT) was collected.A total of 63 age-and sex-matched healthy subjects in the physical examination center were randomly selected as the control group. The differences of blood indexs and lipid metabolism indexes between the two groups were compared.Results In patients with vestibular neuritis, 50 out of 63 patients presented normal threshold in pure tone audiometry, 8 out of 63 patients had bilateral high-frequency sensorineural hearing loss and 5 out of 63 patients had unilateral mild high-frequency sensorineural hearing loss, 56 out of 63 cases completed the electrocochleogram, of which 3 cases had a binaural-SP/AP amplitude ratio≥0.4, 5 cases had monaural amplitude ratio ≥0.4. Fifty-five out of 63 patients completed the caloric test with CP values greater than 30% in all. The ratio of patients completed cVEMP, oVEMP and vHIT were 46 cases, 22 cases and 30 cases, respectively. 17 out of 63 cases completed all the four vestibular function tests. According to these tests, 49 patients could determine the extent of injury, including 27 cases with unilateral superior vestibular nerve injury, 21 cases with unilateral superior and inferior vestibular nerve injury and 1 case with unilateral inferior vestibular nerve injury. There were significant differences in neutrophil value(P < 0.001), lymphocyte value(P < 0.005), neutrophil/lymphocyte ratio(P < 0.001) and apolipoprotein A1(P < 0.001) between patient group and control group. Inflammatory markers were risk factors for patients with vestibular neuritis. The OR values of neutrophil value and blood neutrophil/lymphocyte ratio were 1.81(1.38-2.37, P < 0.001) and 2.11(1.41-3.16, P < 0.001), respectively. Apolipoprotein A1 was a protective factor for patients with vestibular neuritis, and the OR value was 0.004(0.001-0.042, P < 0.001).Conclusion Electrocochleogram could be used in vestibular neuritis patients with normal pure tone threshold to test whether there is hidden hearing loss in these patients. Neutrophil value, lymphocyte value, neutrophil/lymphocyte ratio and apolipoprotein A1 were correlated with vestibular neuritis. The Neutrophil value and neutrophil/lymphocyte ratio were risk factors for morbidity.
-

-
表 1 病例组和对照组基线资料
项目 病例组(n=63) 对照组(n=63) P 年龄/X±S 40.21±15.01 40.08±14.94 0.96 年龄(中位数)/岁 38(25) 38(24) 性别/例(%) 男 35(55.6) 35(55.6) 1.00 女 28(44.4) 28(44.4) 1.00 高血压/例(%) 7(11.1) 5(7.9) 糖尿病/例(%) 3(4.8) 1(1.6) 表 2 外周血炎症指标及脂代谢指标在2组中的分布
各项指标 病例组(n=63) 对照组(n=63) OR(95%CI) P 中性粒细胞 6.16±3.40 3.59±1.31 1.810(1.380~2.370) < 0.001 淋巴细胞 1.83±0.81 2.11±0.61 0.580(0.340~0.970) 0.039 血小板 239.74±56.20 257.56±51.49 0.994(0.987~1.000) 0.069 中性/淋巴比值 4.70±5.15 1.85±0.77 2.110(1.410~3.160) < 0.001 血小板/淋巴比值 160.26±98.00 132.78±47.22 1.005(1.000~1.011) 0.065 同型半胱氨酸 16.09±8.28 14.85±7.14 1.020(0.970~1.070) 0.400 载脂蛋白A1 1.23±0.22 1.51±0.22 0.004(0.000~0.042) < 0.001 甘油三脂TAG 1.47±0.76 1.28±0.70 1.440(0.850~2.440) 0.180 胆固醇TCHO 4.66±1.15 5.58±1.11 0.430(0.270~0.670) < 0.001 高密度脂蛋白 1.22±0.41 1.43±0.32 0.150(0.040~0.560) 0.004 低密度脂蛋白 2.88±1.07 3.50±0.98 0.510(0.320~0.800) 0.003 25-VitD 57.84±16.10 56.41±18.56 1.010(0.980~-1.030) 0.680 -
[1] Adamec I, Krbot Skorić M, Handžić J, et al. Incidence, seasonality and comorbidity in vestibular neuritis[J]. Neurol Sci, 2015, 36(1): 91-95. doi: 10.1007/s10072-014-1912-4
[2] Nylen CO. Some cases of ocular nystagmus due to certain positions of the head[J]. Acta oto-laryngologica, 1924, 6(1): 106-137. doi: 10.3109/00016482409123851
[3] Gacek RR, Gacek MR. Viral neuropathies in the temporal bone[M]. Introduction. Adv Otorhinolaryngol. 2002: Ⅶ-Ⅸ.
[4] Hallpike CS. The pathology and differential diagnosis of aural vertigo, Proc 4th Intern Congress Otolaryngol[C]. London: Br Med Ass, 1949.
[5] Fetter M, Dichgans J. Vestibular neuritis spares the inferior division of the vestibular nerve[J]. Brain, 1996, 119(Pt 3): 755-763.
[6] Strupp M, Bisdorff A, Furman J, et al. Acute unilateral vestibulopathy/vestibular neuritis: Diagnostic criteria[J]. J Vestib Res, 2022, 32(5): 389-406. doi: 10.3233/VES-220201
[7] Le TN, Westerberg BD, Lea J. Vestibular neuritis: recent advances in etiology, diagnostic evaluation, and treatment[J]. Adv Otorhinolaryngol, 2019, 82: 87-92.
[8] Greco A, Macri GF, Gallo A, et al. Is vestibular neuritis an immune related vestibular neuropathy inducing Vertigo?[J]. J Immunol Res, 2014, 2014: 459048
[9] Vnel S, Yilmaz M, Albayram S, et al. Anastomoses of the vestibular, cochlear, and facial nerves[J]. J Craniofac Surg, 2012, 23(5): 1358-1361. doi: 10.1097/SCS.0b013e31824e63fe
[10] Arbusow V, Schulz P, Strupp M, et al. Distribution of herpes simplex virus type 1 in human geniculate and vestibular Ganglia: implications for vestibular neuritis[J]. Ann Neurol, 1999, 46(3): 416-419. doi: 10.1002/1531-8249(199909)46:3<416::AID-ANA20>3.0.CO;2-W
[11] Büki B, Ward BK. Length of the narrow bony channels may not be the sole cause of differential involvement of the nerves in vestibular neuritis[J]. Otol Neurotol, 2021, 42(7): e918-e924. doi: 10.1097/MAO.0000000000003161
[12] Büki B, Mair A, Pogson JM, et al. Three-dimensional high-resolution temporal bone histopathology identifies areas of vascular vulnerability in the inner ear[J]. Audiol Neurootol, 2022, 27(3): 249-259. doi: 10.1159/000521397
[13] Goudakos JK, Markou KD, Psillas G, et al. Corticosteroids and vestibular exercises in vestibular neuritis. Single-blind randomized clinical trial[J]. JAMA Otolaryngol Head Neck Surg, 2014, 140(5): 434-440. doi: 10.1001/jamaoto.2014.48
[14] 李洁, 时海波. 前庭代偿与治疗机制研究进展[J]. 临床耳鼻咽喉头颈外科杂志, 2024, 38(3): 256-260. https://lceh.whuhzzs.com/article/doi/10.13201/j.issn.2096-7993.2024.03.015
[15] Legatt AD. Electrophysiology of cranial nerve testing: auditory nerve[J]. J Clin Neurophysiol, 2018, 35(1): 25-38. doi: 10.1097/WNP.0000000000000421
[16] Lu Y, Zhang Q, Wen Y, et al. The SP-AP compound wave in patients with auditory neuropathy[J]. Acta Otolaryngol, 2008, 128(8): 896-900. doi: 10.1080/00016480701762482
[17] Liberman MC. HIDDEN HEARING LOSS[J]. Sci Am, 2015, 313(2): 48-53. doi: 10.1038/scientificamerican0815-48
[18] Hornibrook J. Electrocochleography(EcochG)for the diagnosis of cochlear endolymphatic hydrops[J]. J Neurol, 2023, 270(5): 2789. doi: 10.1007/s00415-023-11571-y
[19] 黄丽辉. 隐性听力损失及早期识别[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(7): 668-671. https://lceh.whuhzzs.com/article/doi/10.13201/j.issn.2096-7993.2020.07.023
[20] Vnel S, Yilmaz M, Albayram S, et al. Anastomoses of the vestibular, cochlear, and facial nerves[J]. J Craniofac Surg, 2012, 23(5): 1358-1361. doi: 10.1097/SCS.0b013e31824e63fe
[21] Büki B, Mair A, Pogson JM, et al. Three-dimensional high-resolution temporal bone histopathology identifies areas of vascular vulnerability in the inner ear[J]. Audiol Neurootol, 2022, 27(3): 249-259. doi: 10.1159/000521397
[22] Baloh RW, Lopez I, Ishiyama A, et al. Vestibular neuritis: clinical-pathologic correlation[J]. Otolaryngol Head Neck Surg, 1996, 114(4): 586-592.
[23] Rahko T, Karma P. New clinical finding in vestibular neuritis: high-frequency audiometry hearing loss in the affected ear[J]. Laryngoscope, 1986, 96(2): 198-199.
[24] Milionis HJ, Mittari V, Exarchakos G, et al. Lipoprotein(a)and acute-phase response in patients with vestibular neuronitis[J]. Eur J Clin Invest, 2003, 33(12): 1045-1050.
[25] Şahin Mİ, Kökoğlu K, Gülmez E. Mean platelet volume, neutrophil-and platelet to lymphocyte ratios are elevated in vestibular neuritis[J]. J Clin Neurosci, 2019, 67: 134-138.
[26] Koçak HE, Elbistanlı MS, Acıpayam H, et al. Are neutrophil/lymphocyte and platelet/lymphocyte ratios related with formation of sudden hearing loss and its prognosis?[J]. Eur Ann Otorhinolaryngol Head Neck Dis, 2017, 134(6): 383-386.
[27] Şahin Mİ, Kökoğlu K, Gülmez E. Mean platelet volume, neutrophil-and platelet to lymphocyte ratios are elevated in vestibular neuritis[J]. J Clin Neurosci, 2019, 67: 134-138.
[28] Özler GS, Günak G. Neutrophil-lymphocyte ratio: a new predictive and prognostic factor in patients with Bell palsy[J]. J Craniofac Surg, 2014, 25(3): 944-945.
[29] Han W, Wang D, Wu Y, et al. Correlation between vestibular neuritis and cerebrovascular risk factors[J]. Am J Otolaryngol, 2018, 39(6): 751-753.
[30] Pâris P, Charpiot A, Veillon F, et al. Prevalence of cardiovascular risk factors in superior vestibular neuritis: a cross-sectional study following STROBE guidelines[J]. Eur Ann Otorhinolaryngol Head Neck Dis, 2022, 139(4): 194-197.
[31] Lee JS, Kim DH, Lee HJ, et al. Lipid profiles and obesity as potential risk factors of sudden sensorineural hearing loss[J]. PLoS One, 2015, 10(4): e0122496.
[32] Weng T, Devine EE, Xu H, et al. A clinical study of serum lipid disturbance in Chinese patients with sudden deafness[J]. Lipids Health Dis, 2013, 12: 95.
-

计量
- 文章访问数: 166
- 施引文献: 0




 下载:
下载: