Study on simulated airflow dynamics of children with obstructive sleep apnea treated by different surgical methods
-
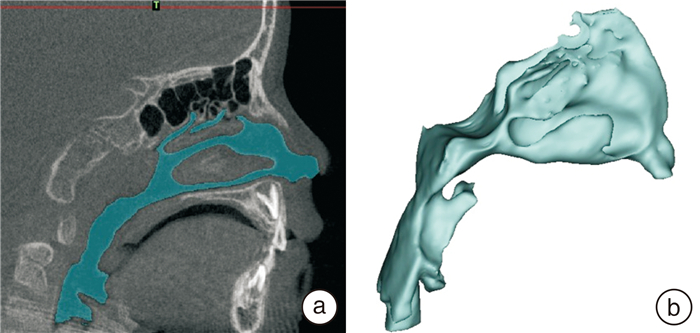
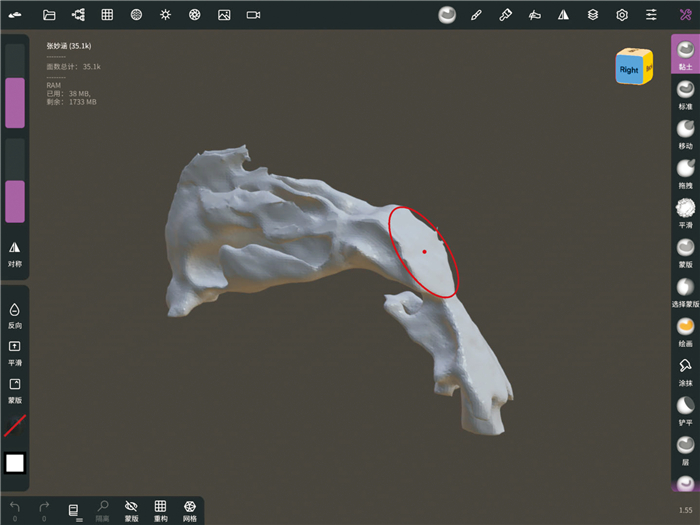
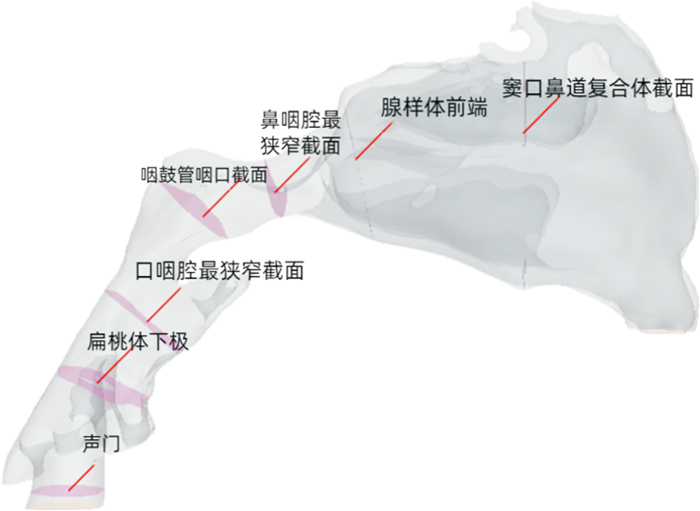
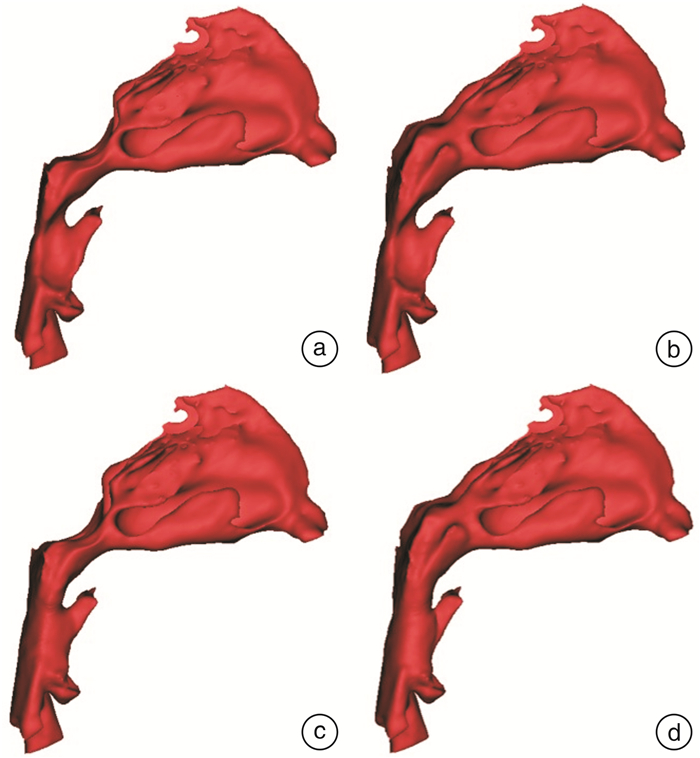
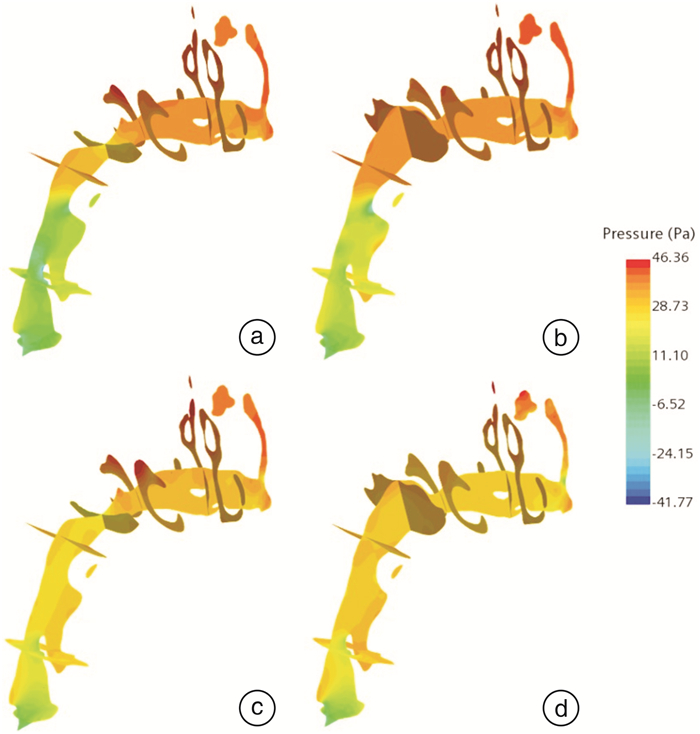
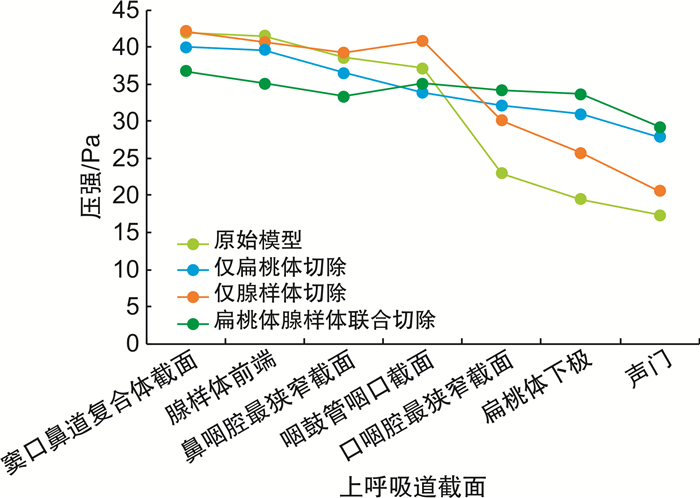
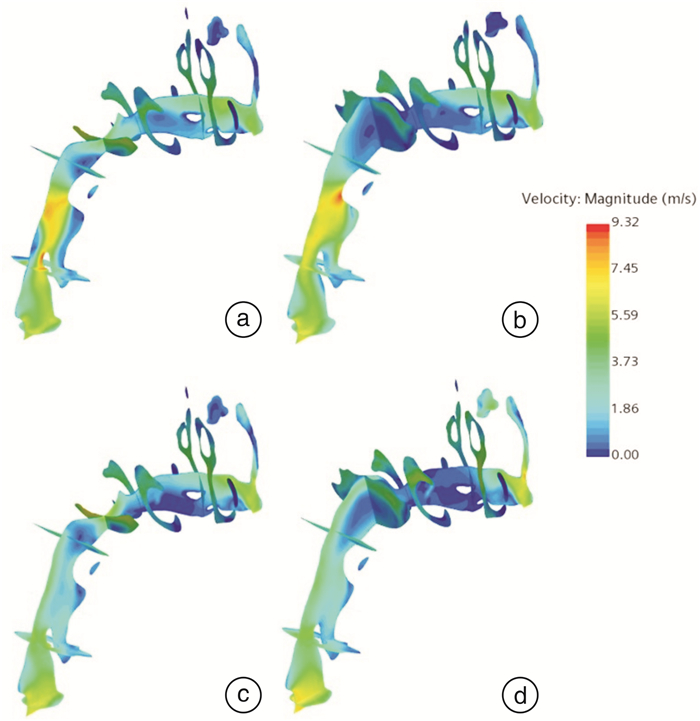
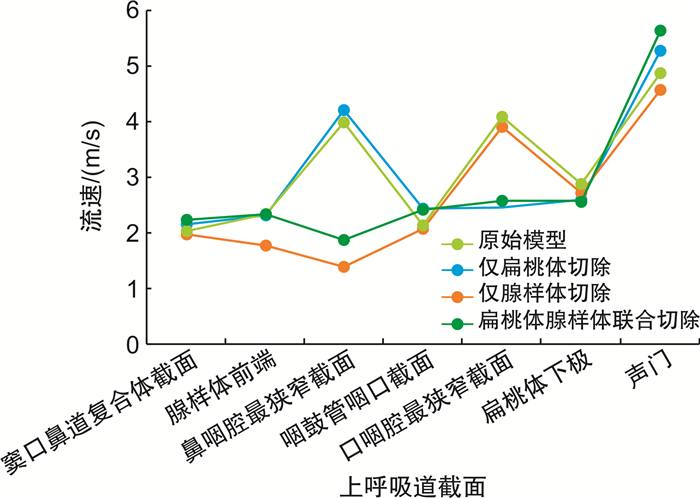
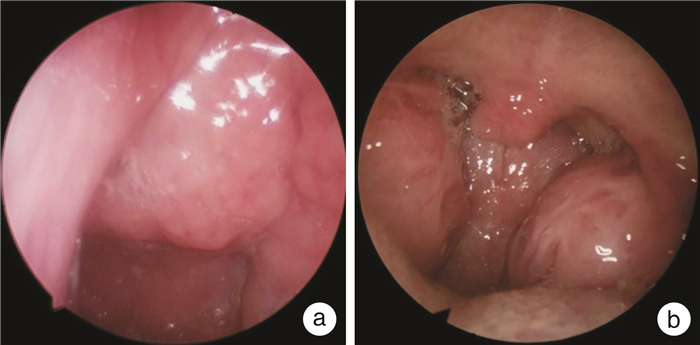
摘要: 目的 利用计算流体力学数值模拟,分析腺样体切除、扁桃体切除及扁桃体腺样体联合切除对阻塞性睡眠呼吸暂停(OSA)患儿的影响。方法 选取典型扁桃体伴腺样体肥大患儿1例。使用Mimics 21.0软件,分别建立术前原始模型、腺样体切除、扁桃体切除及扁桃体腺样体联合切除的虚拟手术模型并采用ANSYS 2019 R1软件建立上气道计算流体力学(CFD)模型,接着对CFD模型内部流场的压强和流速进行数值模拟。选取窦口鼻道复合体截面、腺样体前端、鼻咽腔最狭窄截面、咽鼓管咽口截面、口咽腔最狭窄截面、扁桃体下极和声门截面共计7个与气流迹线垂直的平面作为观测平面,对比指标包括压强、气流流速及气流分布。结果 与术前原始模型相比,仅切除腺样体后,窦口鼻道复合体截面至咽鼓管咽口截面之间的压降减缓、腺样体前端的高流速峰消失、且通过中鼻道的气流迹线增加;仅切除双侧扁桃体后,咽鼓管咽口截面至声门之间的压降减缓、咽鼓管咽口截面至声门之间的流速变得缓慢;扁桃体腺样体联合切除术使得上气道压强分布最为均匀、压强变化和流速最为平缓,通过中鼻道的气流迹线在3种术式中增加最显著。结论 腺样体切除术、扁桃体切除术及扁桃体腺样体联合切除术可在不同程度上使上呼吸道的气流流速和压强变得均匀,但在具体的解剖部位和程度上有明显差别。应用CFD可直观地预测不同手术方式对OSA患儿上气道流场的改善情况,帮助临床医生进行手术方案的决策。Abstract: Objective To analyze the effects of adenoidectomy, tonsillectomy and tonsillectomy combined with adenoidectomy on obstructive sleep apnea children by computational fluid dynamics numerical simulation.Methods A case of typical tonsil with adenoid hypertrophy was selected. Mimics 21.0 software was used to establish the original preoperative model, adenoidectomy, tonsillectomy and virtual surgical models of tonsillectomy combined adenoidectomy, and the computational fluid dynamics model of the upper airway was established by ANSYS 2019 R1 software, and then the pressure and velocity of the internal flow field of the CFD model were numerically simulated. Seven planes perpendicular to the flow trace were selected as the observation planes, including the cross section of the sinusostoma complex, the anterior end of the adenoid body, the narrowest cross section of the nasopharyngeal cavity, the pharyngostoma tube, the narrowest cross section of the oropharyngeal cavity, the lower pole of the tonsil and the glottis section. The comparison indexes included pressure, flow velocity and flow distribution.Results Compared with the original model before operation, after the adenoids were removed only, the pressure drop between the section of the ostiomeatal complex and the section of the eustachian tube decreased, the high velocity peak at the anterior end of the adenoids disappeared, and the flow trace through the middle nasal canal increased. When only bilateral tonsils were removed, the pressure drop between the eustachian tube and the glottis slowed down and the flow velocity between the eustachian tube and the glottis slowed down. Combined tonsillar-adenoidectomy resulted in the most uniform pressure distribution, the most gentle pressure change and flow rate in the upper airway, and the most ignificant increase in airflow trace through the middle nasal canal among the three operations.Conclusion Adenoidectomy, tonsillectomy and combined tonsillar adenoidectomy can make the airflow velocity and pressure of upper respiratory tract uniform to different degrees, but there are obvious differences in the specific anatomical location and degree. The application of CFD can intuitively predict the improvement of upper airway flow field in OSA children by different surgical methods, which helps clinicians to make surgical decision.
-

-
表 1 原始模型及不同虚拟手术后上气道CFD模型各观测平面压强的比较
pa 项目 窦口鼻道复合体截面 腺样体前端 鼻咽腔最狭窄截面 咽鼓管咽口截面 口咽腔最狭窄截面 扁桃体下极 声门 原始模型 41.91 41.50 38.55 37.14 22.97 19.48 17.33 仅腺样体切除 42.12 40.63 39.23 40.83 30.09 25.74 20.60 仅扁桃体切除 39.94 39.60 36.50 33.85 32.12 30.96 27.86 扁桃体腺样体联合切除 36.74 35.07 33.34 35.08 34.16 33.61 29.18 表 2 原始模型及不同虚拟手术后上气道CFD模型各观测平面流速的比较
m/s 项目 窦口鼻道复合体截面 腺样体前端 鼻咽腔最狭窄截面 咽鼓管咽口截面 口咽腔最狭窄截面 扁桃体下极 声门 原始模型 2.03 2.33 3.98 2.13 4.09 2.88 4.87 仅腺样体切除 1.97 1.78 1.38 2.07 3.91 2.72 4.56 仅扁桃体切除 2.16 2.32 4.21 2.43 2.46 2.60 5.26 扁桃体腺样体联合切除 2.24 2.33 1.87 2.42 2.57 2.55 5.64 -
[1] 倪鑫. 中国儿童阻塞性睡眠呼吸暂停诊断与治疗指南(2020)[J]. 中国循证医学杂志, 2020, 20(8): 883-900.
[2] Burgos MA, Rosique L, Piqueras F, et al. Reducing variability in nasal surgery outcomes through computational fluid dynamics and advanced 3D virtual surgery techniques[J]. Heliyon, 2024, 10(5): e26855. doi: 10.1016/j.heliyon.2024.e26855
[3] 张亚, 马瑞萍, 王玉升, 等. 鼻膨胀体对鼻腔气流及艾蒿颗粒沉积的影响[J]. 临床耳鼻咽喉头颈外科杂志, 2023, 37(7): 535-541. https://lceh.whuhzzs.com/article/doi/10.13201/j.issn.2096-7993.2023.07.006
[4] 刘小涵, 雷齐鸣, 张小兵. 计算流体力学在鼻腔疾病临床应用中的进展[J]. 中华耳鼻咽喉头颈外科杂志, 2021, 56(5): 528-531. doi: 10.3760/cma.j.cn115330-20200519-00423
[5] Faizal WM, Ghazali NNN, Khor CY, et al. Computational fluid dynamics modelling of human upper airway: A review[J]. Comput MethodsPrograms Biomed, 2020, 196: 105627.
[6] Hu Z, Dong J, Lou M, et al. Effect of different degrees of adenoid hypertrophy on pediatric upper airway aerodynamics: a computational fluid dynamics study[J]. Biomech Model Mechanobiol, 2023, 22(4): 1163-1175. doi: 10.1007/s10237-023-01707-4
[7] Sun Q, Dong J, Zhang Y, et al. Numerical modelling of micron particle inhalation in a realistic nasal airway with pediatric adenoid hypertrophy: A virtual comparison between pre-and postoperative models[J]. Front Pediatr, 2023, 11: 1083699. doi: 10.3389/fped.2023.1083699
[8] 郭宇峰, 苏丽君, 蔡惠坤, 等. 基于计算流体力学的阻塞性睡眠呼吸暂停儿童与正常儿童上气道流场对比分析[J]. 临床耳鼻咽喉头颈外科杂志, 2021, 35(2): 141-146. doi: 10.13201/j.issn.2096-7993.2021.02.011
[9] Parmar A, Baker A, Narang I. Positive airway pressure in pediatric obstructive sleep apnea[J]. Paediatr Respir Rev, 2019, 31: 43-51.
[10] Weese J, Lungu A, Peters J, et al. CFD-and Bernoulli-based pressure drop estimates: A comparison using patient anatomies from heart and aortic valve segmentation of CT images[J]. Med Phys, 2017, 44(6): 2281-2292. doi: 10.1002/mp.12203
[11] Guo C, Pan L, Chen L, et al. Investigating the epidemiological relevance of secretory otitis media and neighboring organ diseases through an Internet search[J]. PeerJ, 2024, 12: e16981. doi: 10.7717/peerj.16981
[12] Vanneste P, Page C. Otitis media with effusion in children: Pathophysiology, diagnosis, and treatment. A review[J]. J Otol, 2019, 14(2): 33-39. doi: 10.1016/j.joto.2019.01.005
-




 下载:
下载: