Correlation between parameters of suppression head impulse paradigm and changesin DHI score in acute vestibular neuritis
-
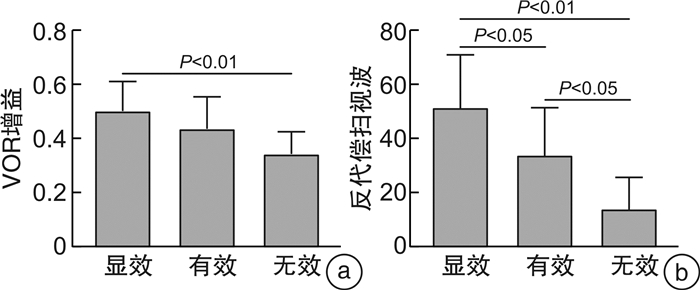
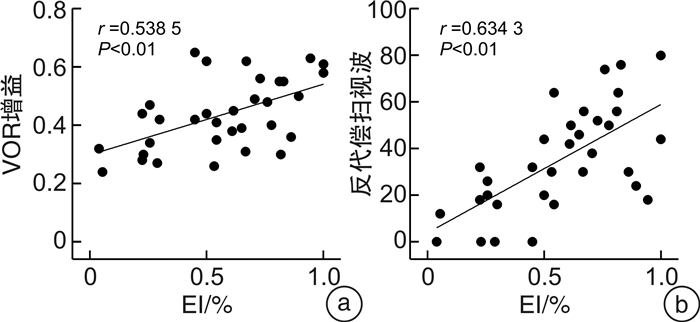
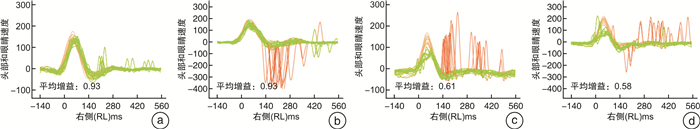
摘要: 目的 探讨视频头脉冲抑制试验(suppression head impulse paradigm,SHIMP)的参数与眩晕障碍量表(dizziness handicap inventory,DHI)评分改变的相关性,以期通过SHIMP的相关参数来评估急性前庭神经炎的眩晕程度及预后。方法 选取急性前庭神经炎患者33例,行DHI量表评估、vHIT和SHIMP检查,病程达2周且不伴自发性眼震时再次行DHI量表评估。以第二次DHI评分的下降幅度,作为疗效指标(efficacy index,EI)。将所有患者按照疗效分为显效、有效和无效3组。比较3组患者SHIMP的前庭眼反射增益值及反代偿扫视波出现率之间的差异。结果 显效组13例,有效组11例,无效组9例。①在各组水平半规管增益均值比较中,显效组增益均值为(0.50±0.11);有效组增益均值为(0.44±0.12);无效组增益均值为(0.34±0.08)。显效组与无效组增益均值差异有统计学意义(P < 0.01)。水平半规管增益值与EI呈正相关(r=0.538 5,P < 0.01);②在各组水平半规管反代偿扫视波出现率均值比较中,显效组反代偿扫视波出现率均值为(51.23±19.59);有效组反代偿扫视波出现率均值为(33.64±17.68);无效组反代偿扫视波出现率均值为(13.78±11.81)。各组间两两比较均差异有统计学意义(P < 0.05)。水平半规管反代偿扫视波出现率与EI呈正相关(r=0.658 2,P < 0.01)。结论 急性前庭神经炎患者SHIMP检查中的增益值以及反代偿扫视波出现率与DHI评分下降幅度密切相关。Abstract: Objective To explore the correlation between the parameters of suppression head impulse paradigm(SHIMP) and changes in dizziness handicap inventory(DHI) scores. Additionally, to evaluate the degree of vertigo and prognosis of patients with acute vestibular neuritis through SHIMP parameters.Methods Thirty-three patients with acute vestibular neuritis were enrolled for DHI evaluation, vHIT and SHIMP. A secondary DHI score were evaluated after after two weeks, once patients no longer exhibited spontaneous nystagmus. The decrease in the second DHI score was used as the efficacy index(EI). All patients were divided into significantly effective group, effective group and ineffective group based on EI. Differences of the VOR gain values of SHIMP and the anti-compensatory saccade were compared among the three groups.Results There were 13 cases in the significant effective group, 11 cases in the effective group, and 9 cases in the ineffective group. ①The mean gain of the horizontal semicircular canal in the significant effective group, the effective group, and the ineffective group was(0.50±0.11), (0.44±0.12), and(0.34±0.08), respectively. The difference between the significant effective group and the ineffective group was statistically significant(P < 0.01). The gain of horizontal semicircular canal was positively correlated with EI(r=0.538 5, P < 0.01)。②The occurrence rate of the anti-compensatory saccade in the significant effective group, the effective group, and the ineffective group was(51.23±19.59), (33.64±17.68), and(13.78±11.81), respectively. Pairwise comparisons between each group showed statistical significance(P < 0.05). The occurrence rate of anti-compensatory saccade was positively correlated with EI(r=0.658 2, P < 0.01).Conclusion The horizontal semicircular canal gain and the occurrence rate of the anti-compensatory saccade in SHIMP for patients with acute vestibular neuritis were closely correlated with decrease in DHI score.
-

-
[1] Tokle G, Mørkved S, Bråthen G, et al. Efficacy of vestibular rehabilitation following acute vestibular neuritis: a randomized controlled trial[J]. Otol Neurotol, 2020, 41(1): 78-85. doi: 10.1097/MAO.0000000000002443
[2] Le TN, Westerberg BD, Lea J. Vestibular neuritis: recent advances in etiology, diagnostic evaluation, and treatment[J]. Adv Otorhinolaryngol, 2019, 82: 87-92.
[3] MacDougall HG, McGarvie LA, Halmagyi GM, et al. A new saccadic indicator of peripheral vestibular function based on the video head impulse test[J]. Neurology, 2016, 87(4): 410-418. doi: 10.1212/WNL.0000000000002827
[4] Casani AP, Canelli R, Lazzerini F, et al. Prognosis after acute unilateral vestibulopathy: Usefulness of the suppression head impulse paradigm(SHIMP)[J]. J Vestib Res, 2021, 31(6): 531-540. doi: 10.3233/VES-210038
[5] Şahin M, Köko lu K, Gülmez E. Mean platelet volume, neutrophil-and platelet to lymphocyte ratios are elevated in vestibular neuritis[J]. J Clin Neurosci, 2019, 67: 134-138. doi: 10.1016/j.jocn.2019.05.062
[6] Kim TS, Lim HW, Yang CJ, et al. Changes of video head impulse test results in lateral semicircular canal plane by different peak head velocities in patients with vestibular neuritis[J]. Acta Otolaryngol, 2018, 138(9): 785-789. doi: 10.1080/00016489.2018.1481523
[7] Park JS, Lee JY, Nam W, et al. Comparing the suppression head impulse paradigm and the head impulse paradigm in vestibular neuritis[J]. and, 2020, 41(1): e76-e82.
[8] Manzari L, Tramontano M. Suppression Head Impulse Paradigm(SHIMP)in evaluating the vestibulo-saccadic interaction in patients with vestibular neuritis[J]. Eur Arch Oto Rhino Laryngol, 2020, 277(11): 3205-3212. doi: 10.1007/s00405-020-06085-6
[9] 李俊, 张云美, 时晨, 等. 前庭神经炎患者视频头脉冲试验与DHI评分的相关性分析[J]. 临床耳鼻咽喉头颈外科杂志, 2022, 36(11): 854-858. https://lceh.whuhzzs.com/article/doi/10.13201/j.issn.2096-7993.2022.11.009
[10] 中国医师协会神经内科分会眩晕专业委员会, 中国卒中学会卒中与眩晕分会. 前庭神经炎诊治多学科专家共识[J]. 中华老年医学杂志, 2020, 39(9): 985-994.
[11] 丁雷, 刘畅, 王嘉玺, 等. 眩晕残障程度评定量表(中文版)的评价[J]. 中华耳科学杂志, 2013, 11(2): 228-230. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHER201302016.htm
[12] Whitney SL, Wrisley DM, Brown KE, et al. Is perception of handicap related to functional performance in persons with vestibular dysfunction?[J]. Otol Neurotol, 2004, 25(2): 139-143. doi: 10.1097/00129492-200403000-00010
[13] Yang TH, Xirasagar S, Cheng YF, et al. Peripheral Vestibular Disorders: Nationwide Evidence From Taiwan[J]. Laryngoscope, 2021, 131(3): 639-643. doi: 10.1002/lary.28877
[14] Roehm PC, Camarena V, Nayak S, et al. Cultured vestibular ganglion neurons demonstrate latent HSV1 reactivation[J]. Laryngoscope, 2011, 121(10): 2268-2275. doi: 10.1002/lary.22035
[15] Strupp M, Brandt T. Peripheral vestibular disorders[J]. Curr Opin Neurol, 2013, 26(1): 81-89. doi: 10.1097/WCO.0b013e32835c5fd4
[16] Arbusow V, Derfuss T, Held K, et al. Latency of herpes simplex virus type-1 in human geniculate and vestibular Ganglia is associated with infiltration of CD8+T cells[J]. J Med Virol, 2010, 82(11): 1917-1920. doi: 10.1002/jmv.21904
[17] Pollak L, Book M, Smetana Z, et al. Herpes simplex virus type 1 in saliva of patients with vestibular neuronitis: a preliminary study[J]. Neurologist, 2011, 17(6): 330-332. doi: 10.1097/NRL.0b013e318235a0e7
[18] 庄建华. 前庭神经炎不同时期的临床特征和处理策略[J]. 中华内科杂志, 2023, 62(7): 743-747.
[19] Fetter M. Vestibulo-ocular reflex[J]. Dev Ophthalmol, 2007, 40: 35-51. doi: 10.1159/000100348
[20] 陈飞云, 张玉忠, 吴彩芹, 等. 头脉冲抑制试验在单侧前庭神经炎患者中的应用价值[J]. 临床耳鼻咽喉头颈外科杂志, 2018, 32(18): 1374-1377. https://lceh.whuhzzs.com/article/doi/10.13201/j.issn.1001-1781.2018.18.003
-

计量
- 文章访问数: 226
- 施引文献: 0



 下载:
下载: