Hearing care network for early identification of delayed hearing loss in preschool children
-
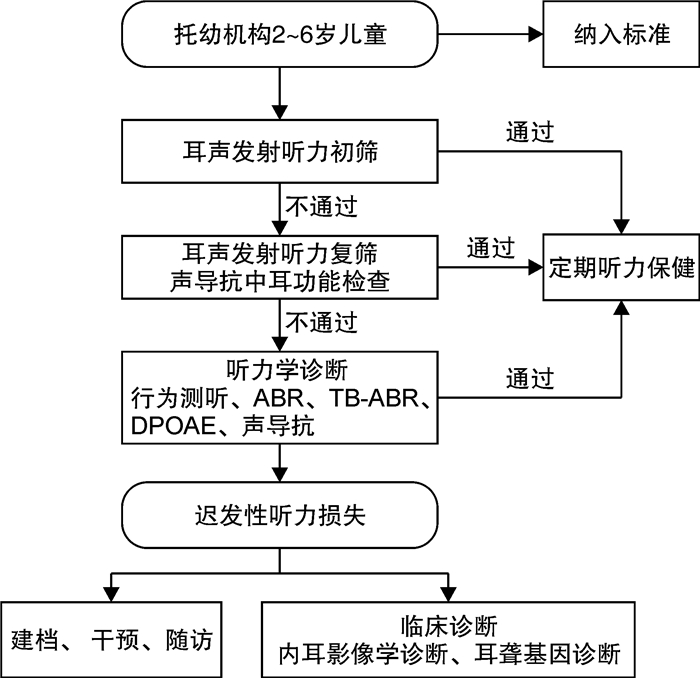
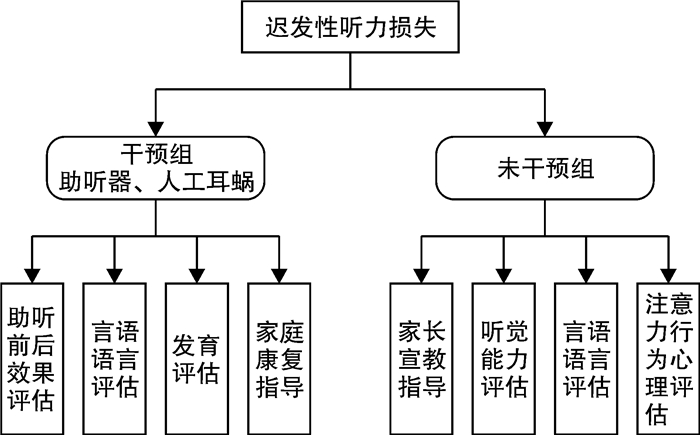
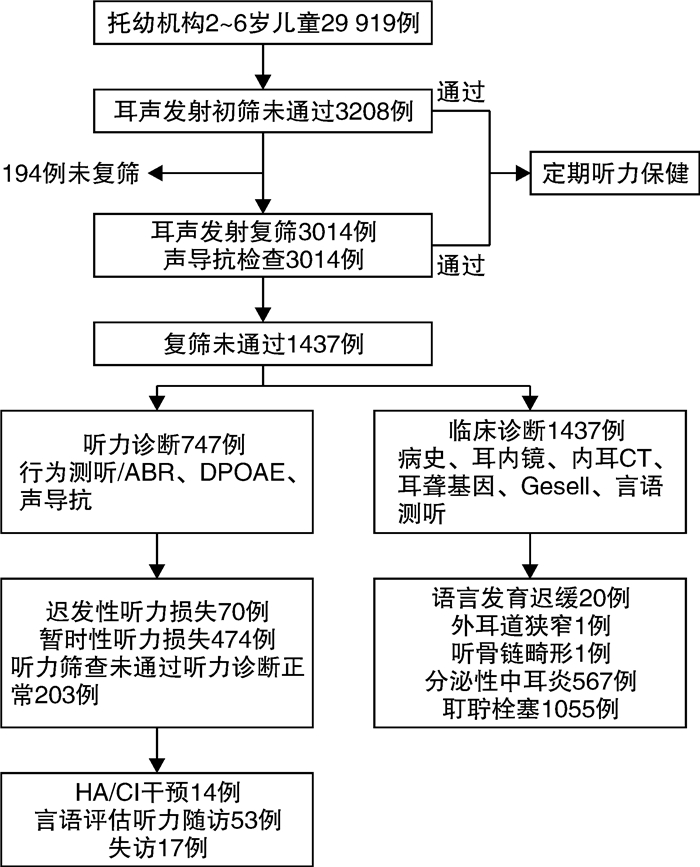
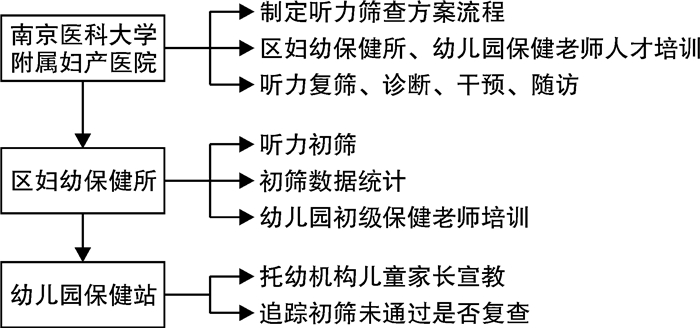
摘要: 目的 建立南京市托幼机构听力保健网络,对迟发性听力损失进行早期识别和干预,并评价听力保健网络的应用效果。方法 通过建立听力保健网络对南京地区托幼机构儿童进行听力筛查、诊断和随访。听力初筛应用畸变产物耳声发射(DPOAE),初筛未通过的儿童半个月内进行复筛,听力复筛采用DPOAE和声导抗检查,复筛未通过的儿童进行临床诊断和听力学评估,确诊为迟发性听力损失的儿童同时行言语评估、助听干预和听力言语的随访。结果 2019年5月—2022年9月共有29 919例托幼机构儿童完成听力筛查,其中3208例(10.7%)初筛未通过,1437例(47.7%)复筛未通过,747例完成听力学诊断,70例(0.23%)儿童诊断为迟发性听力损失,其中,20例伴有语言发育迟缓,12例验配了助听器,2例行人工耳蜗植入,此外还完成了53例儿童的言语评估和听力学随访。结论 托幼机构听力筛查有助于早期发现迟发性听力损失和语言发育迟缓的儿童,建立托幼机构听力保健网络有利于儿童听力损失的早期识别和干预。Abstract: Objective To establish a hearing care network for preschool children in Nanjing, to perform early identification and intervention for delayed hearing loss, and to evaluate the application effect of the hearing care network.Methods Through the establishment of a hearing care network, hearing screening, diagnosis and follow-up of preschool children were conducted. Distortion product otoacoustic emissions(DPOAE) was adopted for primary hearing screening. Children who failed in the primary screening were re-screened within half a month. DPOAE and acoustic impedance test were used for hearing re-screening. Clinical diagnosis and audiological evaluation were performed for children who failed in the re-screening. Speech assessment, hearing aid intervention, and audio-speech follow-up were conducted for children diagnosed with delayed hearing loss.Results Among 29 919 preschool children completing the hearing screening from May 2019 to September 2022, 3208 cases(10.7%) failed the primary screening and 1437 cases(47.7%) failed the re-screening. Total 747 children completed the hearing diagnosis, and 70 children were diagnosed with delayed hearing loss, with a detection rate of 0.23%. Among them, 20 cases were accompanied by language development delay, in which 12 cases received hearing aids and 2 cases received cochlear implantation. In addition, speech assessment and audiological follow-up were completed for 53 children.Conclusion The hearing screening for preschool children is beneficial for early detection of children with delayed hearing loss and language development delay. Besides, the establishment of hearing care network is conducive to early identification and intervention of children with hearing loss.
-
Key words:
- hearing care network /
- preschool children /
- hearing screening /
- delayed hearing loss
-

-
表 1 托幼机构听力初筛与复筛结果
例(%) 时间/年 初筛 初筛未通过 复筛 复筛未通过 2019 7578(25.3) 1314(17.3) 1268(96.5) 787(62.1) 2020 6027(20.1) 554(9.2) 478(86.3) 145(30.3) 2021 9893(33.1) 801(8.1) 772(96.4) 347(44.9) 2022 6421(21.5) 539(8.4) 496(92.0) 158(31.9) 合计 29 919(100.0) 3208(10.7) 3014(94.0) 1437(47.7) 表 2 70例迟发性听力损失分布(双耳损失程度按较好耳算)
例 组别 例数 单耳听力损失 双耳听力损失 合计 轻度 中度 重度 极重度 轻度 中度 重度 极重度 2岁组 1977 7 2 0 0 7 0 0 2 18 3岁组 8499 7 3 0 0 9 4 1 0 24 4岁组 7841 2 0 1 0 8 0 1 1 13 5岁组 7713 3 2 0 0 5 0 0 0 10 6岁组 3889 1 0 0 0 3 0 1 0 5 合计 29 919 20 7 1 0 32 4 3 3 70 表 3 迟发性听力损失病因学结果
确诊月龄 听力损失程度 耳聋基因诊断 影像学
(内耳MRI/CT)听力损失高危因素 左耳 右耳 30 正常 轻度 TMC1c.1622T>C/-
ALMS1c.11557A>T/-(-) 30 轻度 正常 GJB2c.109G>A/c.109G>A 右乳突炎 37 正常 轻度 GJB2c.235delC/-
SLC26A4c.1975G>C/-(-) 44 正常 轻度 未测 未测 耳聋家族史(母亲先天性聋) 25 轻度 轻度 (—) (—) 早产,低体重,新生儿窒息,新生儿脑病 26 轻度 轻度 USH2Ac.9815C>T/c.10011C>A (—) 27 轻度 轻度 GJB2c.235delC/- (-) 早产,低体重 37 轻度 轻度 未测 右前半规管局部显示欠清 37 轻度 轻度 GJB2c.109G>A/c.109G>A 右后半规管不连续 60 轻度 轻度 GJB2c.109G>A/c.598G>A (—) 早产,低体重,NICU住院5 d 60 轻度 轻度 GJB2c.109G>A/c.109G>A (—) 耳聋家族史(祖父的叔叔耳聋) 66 轻度 轻度 GJB2c.109G>A/c.109G>A 左前半规管局部未显示 72 轻度 轻度 GJB2c.109G>A/c.235delC (—) 耳聋家族史(姑姑迟发性聋) 73 轻度 轻度 MYO1Ac.2270G>A/-
MYO3Ac.2794-1G>A/-右前半规管发育不良 43 轻度 中度 GATA3c.65_68dup/- 双侧耳蜗顶圈与中圈融合 42 中度 中度 未测 双锤骨异常、锤砧关节融合 高胆红素血症,耳聋家族史(母亲迟发性聋) 37 正常 中度 未测 右外耳道狭窄 48 正常 重度 未测 右蜗神经发育不良 36 重度 重度 TECTAc.4977-1G>A/- (—) 耳聋家族史(母亲、外祖母迟发性聋) 30 极重度 极重度 GJB2c.109G>A/c.109G>A (—) -
[1] 吴皓, 黄治物. 婴幼儿听力损失诊断与干预指南[J]. 中华耳鼻咽喉头颈外科杂志, 2018, 53(3): 181-188. doi: 10.3760/cma.j.issn.1673-0860.2018.03.004
[2] 李兴启, 王秋菊. 听觉诱发反应及应用[M]. 北京: 人民军医出版社, 2015: 312-313.
[3] 顾海玲, 孔维丽, 尹晓玲, 等. logistic回归联合ROC曲线评价IT-MAIS得分在预测0~36月龄婴幼儿听力损失程度中的诊断价值[J]. 临床耳鼻咽喉头颈外科杂志, 2022, 36(2): 109-114. https://lceh.whuhzzs.com/article/doi/10.13201/j.issn.2096-7993.2022.02.007
[4] 吴艳, 李刚, 马莹, 等. 1~3岁植入人工耳蜗患儿韵母辨识能力的发育规律研究[J]. 临床耳鼻咽喉头颈外科杂志, 2019, 33(10): 918-922. doi: 10.13201/j.issn.1001-1781.2019.10.005
[5] 张颖, 王俊峰, 丁艳华. 儿童语言发育迟缓的临床特征和影响因素研究[J]. 中国儿童保健杂志, 2022, 30(8): 912-915. https://www.cnki.com.cn/Article/CJFDTOTAL-ERTO202208021.htm
[6] 刘建菊, 张芳, 孙喜斌. 听障儿童言语识别能力评估标准的修订[J]. 中国听力语言康复科学杂志, 2014, 12(5): 357-361. doi: 10.3969/j.issn.1672-4933.2014.05.011
[7] 谢静, 贺璐, 龚树生. WHO世界听力报告的解读与思考[J]. 中华耳鼻咽喉头颈外科杂志, 2021, 56(10): 1131-1135. doi: 10.3760/cma.j.cn115330-20210430-00241
[8] 曲成毅, 王艳平, 韩睿, 等. 中国听障儿童助听器验配康复服务成本的经济学分析[J]. 中国听力语言康复科学杂志, 2009, 7(5): 16-21. doi: 10.3969/j.issn.1672-4933.2009.05.003
[9] Kraft CT, Malhotra S, Boerst A, et al. Risk indicators for congenital and delayed-onset hearing loss[J]. Otol Neurotol, 2014, 35(10): 1839-1843. doi: 10.1097/MAO.0000000000000615
[10] Joint Committee on Infant Hearing. Year 2019 Position Statement: Principles and Guidelines for Early Hearing Detection and Intervention Programs[J]. J Early hear Detect Interv, 2019, 4(2): 1-44.
[11] Shen J, Oza AM, Del Castillo I, et al. Consensus interpretation of the p. Met34Thr and p. Val37Ile variants in GJB2 by the ClinGen Hearing Loss Expert Panel[J]. Genet Med, 2019, 21(11): 2442-2452. doi: 10.1038/s41436-019-0535-9
[12] 牛文侠, 许慧娟, 秦利涛, 等. 42例迟发性非综合征性耳聋患者基因型与临床表型分析[J]. 临床耳鼻咽喉头颈外科杂志, 2021, 35(2): 131-136. https://lceh.whuhzzs.com/article/doi/10.13201/j.issn.2096-7993.2021.02.009
[13] 崔庆佳, 黄丽辉, 韩任杰, 等. 3~6岁儿童不同听力筛查方法比较[J]. 听力学及言语疾病杂志, 2020, 28(2): 128-132. doi: 10.3969/j.issn.1006-7299.2020.02.003
[14] Lu TM, Wu FW, Chang H, et al. Using click-evoked auditory brainstem response thresholds in infants to estimate the corresponding pure-tone audiometry thresholds in children referred from UNHS[J]. Int J Pediatr Otorhinolaryngol, 2017, 95: 57-62. doi: 10.1016/j.ijporl.2017.02.004
[15] 谢雯, 刘月辉, 段茂利. 小儿行为测听现状及研究进展[J]. 中华耳科学杂志, 2020, 18(5): 947-952. doi: 10.3969/j.issn.1672-2922.2020.05.027
[16] Ricalde RR, Chiong CM, Labra P. Current assessment of newborn hearing screening protocols[J]. Curr Opin Otolaryngol Head Neck Surg, 2017, 25(5): 370-377.
[17] Zussino J, Zupan B, Preston R. Speech, language, and literacy outcomes for children with mild to moderate hearing loss: A systematic review[J]. J Commun Disord, 2022, 99: 106248.
[18] 孙敬涛, 刘海红, 王雪瑶, 等. 听性脑干反应对于婴幼儿不同性质听力损失的应用性分析[J]. 临床耳鼻咽喉头颈外科杂志, 2022, 36(2): 120-125. https://lceh.whuhzzs.com/article/doi/10.13201/j.issn.2096-7993.2022.02.009
-




 下载:
下载: