Diagnostic value of IT-MAIS scores by logistic regression and ROC curve in predicting the degree of hearing loss in infants and toddlers aged 0-36 months
-
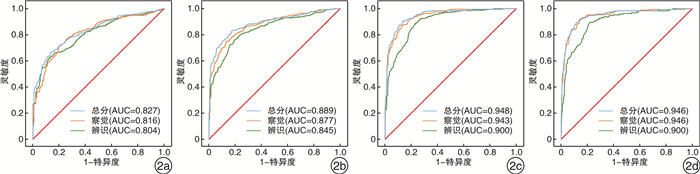
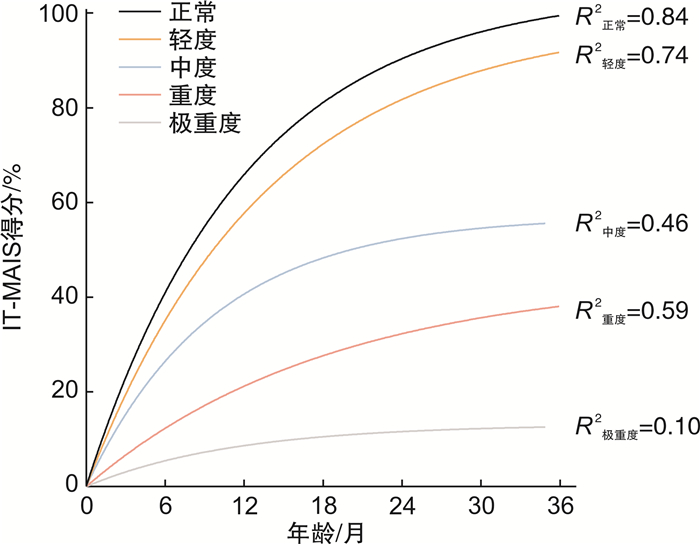
摘要: 目的 比较正常听力和不同程度听力损失婴幼儿的早期语前听能发展轨迹,并探讨婴幼儿有意义听觉整合量表(IT-MAIS)得分在0~36月龄婴幼儿听力损失程度中的诊断价值。方法 收集2009年3月-2021年3月231名听力正常和611名不同程度听力损失患儿的临床资料。对不同程度听力损失患儿IT-MAIS得分随年龄的变化进行非线性回归拟合。分别构建IT-MAIS总得分、察觉得分和辨识得分与评估年龄联合的三种logistic回归模型,绘制ROC曲线,评价诊断效能。结果 轻、中、重、极重度患儿IT-MAIS得分随年龄的变化规律和正常听力婴幼儿的发育规律相似,均随年龄的增长而增长,且听力损失程度越严重,增长速率越缓慢,能达到的峰值越低。联合IT-MAIS总得分和评估年龄构建的logistic模型区分轻度及以上、中度及以上、重度及以上和极重度的AUC最佳,分别为0.827,0.889,0.948,0.946。对于极重度听力损失患儿的诊断效能最优,敏感度为89.6%,特异度为88.4%。听力损失程度越重,IT-MAIS的区分准确性越高,诊断效能越佳。结论 基于IT-MAIS量表构建的logistic模型联合ROC曲线法在鉴别0~36月龄婴幼儿听力损失程度诊断中有良好的诊断效能。当婴幼儿无法配合小儿行为测听、小儿测听结果不可靠、没有电生理条件时,IT-MAIS量表有望用于辅助预估婴幼儿听力损失程度,更加全面地了解患儿的听功能状态,为后续制定康复干预策略提供依据,具有一定的临床应用价值。Abstract: Objective This study is inorder to compare the early prelingual auditory development trajectory of infants and toddlers with normal hearing and different degrees of hearing loss, and to explore the value of the Infant-Toddler Meaningful Auditory Integration Scale (IT-MAIS) scores in the diagnosis of hearing loss severity in infants and toddlers aged 0-36 months.Methods Eight hundred and forty-two cases of infant-toddler from March 2009 to March 2021 were selected as participants, including 231 cases with normal hearing and 611 cases with hearing loss. The IT-MAIS scores of participants with different degrees of hearing loss were fitted with nonlinear regression with age. By respectively constructing three logistic regression models of IT-MAIS total scores, perception scores, discrimination scores and evaluation age, the ROC curve was drawn to evaluate the diagnostic efficacy.Results The IT-MAIS scores of children with mild, moderate, severe, and profound hearing loss participants changes with age are similar to the development of infants with normal hearing, and they all increase with age. And the more severe the hearing loss, the slower the growth rate, and the lower the peak value that can be reached. The logistic model constructed by combining IT-MAIS total score and evaluation age is the best to distinguish mild and above, moderate and above, severe and above, and profound hearing loss, whose AUC are 0.827, 0.889, 0.948, 0.946. The diagnostic efficiency is the best for infant-toddlers with profound hearing loss, with a sensitivity of 89.6% and a specificity of 88.4%. The more severe the hearing loss, the higher the discrimination accuracy of IT-MAIS and the better the diagnostic efficiency.Conclusion The logistic model based on the IT-MAIS scale and the ROC curve method have a good efficiency in the diagnosis of hearing loss severity in infants and toddlers aged 0-36 months. When the child cannot cooperate with behavioral audiometry, the results of behavioral audiometry are unreliable, and there is no electrophysiological condition, the IT-MAIS scale is expected to evaluate the degree of infants' hearing loss as an auxiliary tool. It can understand the children's auditory function state more and provides a basis for the subsequent formulation of rehabilitation intervention strategies with certain clinical application value.
-
Key words:
- infant-toddler /
- hearing loss /
- scale /
- ROC curve
-

-
表 1 不同听力损失程度患儿的基线特征
变量 听力损失程度 P值 正常 轻度 中度 重度 极重度 样本量 231 194 135 89 192 性别/例(%) 0.207 女 103(44.59) 66(34.02) 59(43.70) 39(43.82) 77(40.10) 男 128(55.41) 128(65.98) 76(56.30) 50(56.18) 115(59.90) 评估年龄/月 11.26±10.63 7.19±6.08 8.77±6.81) 11.08±10.70 13.64±10.13 < 0.001 双侧听力基本对称/例(%) < 0.001 否 119(51.52) 37(19.07) 41(30.37) 38(42.70) 3(1.56) 是 112(48.48) 157(80.93) 94(69.63) 51(57.30) 189(98.44) IT-MAIS总分 50.71±30.77 35.44±22.81 29.32±19.27 17.22±13.36 7.94±10.95 < 0.001 察觉得分 65.81±26.25 52.30±23.74 43.52±21.19 25.45±13.32 11.33±13.46 < 0.001 辨识得分 40.35±36.18 23.15±25.50 20.15±22.48 10.42±17.69 3.49±10.77 < 0.001 表 2 三种logistic模型区分婴幼儿不同程度听力损失的曲线下面积AUC
听力损失程度 年龄+总得分 年龄+察觉得分 年龄+辨别得分 AUC SE 95%CI AUC SE 95%CI AUC SE 95%CI 轻度及以上 0.827 0.015 0.798,0.855 0.816 0.015 0.786,0.846 0.804 0.015 0.774,0.835 中度及以上 0.889 0.012 0.867,0.912 0.877 0.012 0.854,0.901 0.845 0.013 0.819,0.872 重度及以上 0.948 0.008 0.933,0.963 0.943 0.008 0.927,0.958 0.900 0.011 0.880,0.921 极重度 0.946 0.009 0.928,0.965 0.946 0.009 0.928,0.964 0.900 0.012 0.876,0.925 表 3 IT-MAIS得分区分婴幼儿不同程度听力损失的诊断效能
听力损失程度 准确性 灵敏度 特异度 截断值 约登指数 回归方程 轻度及以上 0.779 0.667 0.861 >0.790 0.529 Y=2.13+0.11×月龄-0.06×总分 中度及以上 0.829 0.834 0.824 >0.499 0.658 Y=0.83+0.24×月龄-0.10×总分 重度及以上 0.886 0.904 0.864 >0.354 0.768 Y=0.39+0.29×月龄-0.18×总分 极重度 0.910 0.896 0.884 >0.299 0.780 Y=-0.12+0.20×月龄-0.19×总分 -
[1] 聂文英, 吴汉荣, 戚以胜. 新生儿及婴幼儿听力损失[J]. 中国妇幼保健, 2004, 19(22): 124-126. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFYB200416087.htm
[2] 韩冰, 历建强, 兰兰, 等. 中国内地新生儿听力筛查情况的回顾性分析[J]. 听力学及言语疾病杂志, 2012, 20(1): 6-11. doi: 10.3969/j.issn.1006-7299.2012.01.003
[3] 曾镇罡, 张燕梅, 尚美霞, 等. 新生儿听力筛查与诊断质控量表的信度和效度分析[J]. 听力学及言语疾病杂志, 2021, 29(2): 158-161. doi: 10.3969/j.issn.1006-7299.2021.02.010
[4] Delaroche M, Thiébaut R, Dauman R. Behavioral audiometry: validity of audiometric measurements obtained using the 《Delaroche protocol》 in babies aged 4--18 months suffering from bilateral sensorineural hearing loss[J]. Int J Pediatr Otorhinolaryngol, 2006, 70(6): 993-1002. doi: 10.1016/j.ijporl.2005.10.010
[5] Probst R. [Subjective and objective audiometry][J]. Ther Umsch Rev Ther, 2004, 61(1): 7-14. doi: 10.1024/0040-5930.61.1.7
[6] Singleton A J, Waltzman S B. Audiometric Evaluation of Children with Hearing Loss[J]. Otolaryngol Clin North Am, 2015, 48(6): 891-901. doi: 10.1016/j.otc.2015.06.002
[7] 李刚, 郑芸, 张圆. 探讨IT-MAIS在儿童听力评估中的临床价值[J]. 中国听力语言康复科学杂志, 2016, 14(4): 275-277. doi: 10.3969/j.issn.1672-4933.2016.04.010
[8] Barker BA, Donovan NJ, Schubert AD, et al. Using Rasch Analysis to Examine the Item-Level Psychometrics of the Infant-Toddler Meaningful Auditory Integration Scales[J]. Speech Lang Hear Lond Engl, 2017, 20(3): 130-143. doi: 10.1080/2050571X.2016.1243747
[9] 郑芸, 孟照莉, 胥科, 等. ITMAIS在听障婴幼儿早期干预中的临床应用[J]. 中国听力语言康复科学杂志, 2011, 9(4): 26-31. doi: 10.3969/j.issn.1672-4933.2011.04.006
[10] Liang S, Soli S D, Zheng Y, et al. Initial classification of pediatric hearing impairment using behavioral measures of early prelingual auditory development[J]. Int J Audiol, 2016, 55(4): 224-231. doi: 10.3109/14992027.2015.1120891
[11] 陈建勇. 婴幼儿听力损失评估国际共识[J]. 临床耳鼻咽喉头颈外科杂志, 2018, 32(12): 886-890. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201812003.htm
[12] 杨奉玲. 常用的婴幼儿听觉功能评估工具[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(11): 1045-1048. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202011023.htm
[13] 李刚, 陶勇, 孟照莉, 等. 同龄接受助听器或人工耳蜗干预的极重度聋患儿早期语前听能发育规律的对比研究[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(1): 41-44. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202001010.htm
[14] Lu X, Qin Z. Auditory and language development in Mandarin-speaking children after cochlear implantation[J]. Int J Pediatr Otorhinolaryngol, 2018, 107: 183-189. doi: 10.1016/j.ijporl.2018.02.006
[15] Zheng Y, Soli S D, Wang K, et al. A normative study of early prelingual auditory development[J]. Audiol Neurootol, 2009, 14(4): 214-222.
[16] Cavicchiolo S, Mozzanica F, Guerzoni L, et al. Early prelingual auditory development in Italian infants and toddlers analysed through the Italian version of the Infant-Toddler Meaningful Auditory Integration Scale(IT-MAIS)[J]. Eur Arch Otorhinolaryngol, 2018, 275(2): 615-622. doi: 10.1007/s00405-017-4847-6
[17] Kishon-Rabin L, Taitelbaum-Swead R, Ezrati-Vinacour R, et al. Prelexical vocalization in normal hearing and hearing-impaired infants before and after cochlear implantation and its relation to early auditory skills[J]. Ear Hear, 2005, 26(4 Suppl): 17S-29S.
[18] Yang F, Zheng Y, Li G. Early Prelingual Auditory Development of Infants and Toddlers With Unilateral Hearing Loss[J]. Otol Neurotol, 2020, 41(5): 654-650. doi: 10.1097/MAO.0000000000002584
[19] Wiseman K, Sapp C, Walker E, et al. Comprehensive Audiological Management of Hearing Loss in Children, Including Mild and Unilateral Hearing Loss[J]. Otolaryngol Clin North Am, 2021, 54(6): 1171-1179. doi: 10.1016/j.otc.2021.08.006
[20] Xu TQ, Chen XQ, Wang H. A normative study of auditory development in Mandarin-speaking infants[J]. Chin J Otorhinolaryngol Head Neck Surg, 2013, 48(11): 908-912.
[21] Zheng Y, Soli SD, Tao Y, et al. Early prelingual auditory development and speech perception at 1-year follow-up in Mandarin-speaking children after cochlear implantation[J]. Int J Pediatr Otorhinolaryngol, 2011, 75(11): 1418-1426.
-




 下载:
下载: