-
摘要: 目的探讨再次手术对接受甲状旁腺全切除加自体移植术(PTX+AT)治疗继发性甲状旁腺功能亢进(SHPT)后出现SHPT术后持续(PHPT)患者的疗效。方法回顾性分析北京大学民航临床医学院耳鼻咽喉头颈外科2012年8月—2021年12月行再手术治疗的18例接受PTX+AT术后出现PHPT患者的临床资料,术前通过联合颈部彩色多普勒超声、核素显像、增强CT、MR四种影像学检查对前次手术遗留的甲状旁腺进行定位,再次手术时参照影像学结果切除遗留原位甲状旁腺,并按照清扫式甲状旁腺切除理念扩大手术探查范围,切除遗漏的异位旁腺或额外旁腺。比较术前与术后多时段血清全段甲状旁腺激素(i-PTH)变化,观察术后临床症状改善情况及术后并发症发生情况以评价治疗效果。结果所有患者均成功手术,共切除30枚甲状旁腺,均经术后病理再次确认,其中颈部原位甲状旁腺16枚,异位甲状旁腺14枚(其中异位于上纵隔5枚、胸腺4枚、后纵隔2枚、甲状腺实质内2枚、颈鞘内1枚)。术后6 h患者骨关节痛、皮肤瘙痒明显缓解甚至消失; 术后1周血清i-PTH、钙磷指标均达标,肌无力明显改善; 16例患者术后发生低钙血症,经补钙后均缓解; 6例出现短暂性声嘶。未出现严重并发症及死亡病例。术后随访1年无复发。结论再次手术是SHPT术后持续状态的首选治疗方法,术中按照清扫式甲状旁腺切除理念扩大手术范围,成功率高、并发症少,能有效提高患者生活质量和长期生存率。
-
关键词:
- 继发性甲状旁腺功能亢进 /
- 甲状旁腺全切除 /
- 自体移植术 /
- 再手术
Abstract: ObjectiveTo evaluate the clinical effect of reoperation in persistent hyperparathyroidism (PHPT) patients after operation of parathyroidectomy combined with autotransplantation(PTX+AT) on secondary hyperparathyroidism (SHPT).Methods18 PHPT patients who treated with reoperation after PTX+AT were enrolled in this study during the period from Aug 2012 to Dec 2021 in the Department of Otolaryngology Head and Neck Surgery of Peking University Civil Aviation School of Clinical Medicine, Civil Aviation General Hospital. The remaining parathyroid glands were located by preoperative colour Doppler ultrasonography, radionuclide imaging, enhanced CT and MR imaging in the neck region. Based on the imaging findings, the remaining parathyroid glands were removed in situ, and the missed ectopic or extra parathyroid glands were resected with an extended surgical scope according to the parathyroid dissection method. The surgical effect was evaluated by the changes of clinical symptoms, the dynamic change of serum intact paramyroidhomone(i-PTH) between preoperative and postoperative periods and the surgical complications.ResultsAll the 18 patients accepted successful operation. 30 parathyroid glands were resected confirmed by postoperative pathology, including 16 in situ and 14 ectopic glands(5 in superior mediastinum, 4 in thymus, 2 in posterior mediastinum, 2 in thyroid glands, 1 in carotid sheath).Osteoarthropathy and skin itching were significantly relieved or even disappeared at 6 h after surgery. The levels of serum i-PTH, calcium and phosphorus reached the standards and muscle weakness was significantly improved 1 week after surgery. 16 patients presented hypocalcemia and returned to normal after supplement of calcium. Hoarseness due to temporary injury of laryngeal nerve was found in 6 cases. No serious complications or death occurred after the operation.There was no recurrence after 1 year follow-up.ConclusionReoperation is the first choice for SHPT patients complicated with persistent hyperparathyroidism. Multiple imaging examinations are used to locate the residual parathyroid, especially the ectopic gland. Expanded surgical scope is applied to resect all the residual parathyroid glands(ectopic, in situ and concealed parathyroid) according to the concept of dissection parathyroidectomy. The surgery is effective and safe. Patients'quality of life and long-term survival rate is improved.-
Key words:
- secondary hyperparathyroidism /
- parathyroidectomy /
- autotransplantation /
- reoperation
-

-
表 1 术后1周生化指标变化情况(n=18)
时间 血钙/(mmol·L-1) 血磷/(mmol·L-1) 钙磷乘积/(mg2·dL-2) 血红蛋白/(g·L-1) 红细胞比容/% 术前 2.41±0.28 2.18±0.52 66.78±16.94 123.78±20.69 38.76±7.57 术后 1.94±0.35 1.83±0.61 44.47±15.94 121.46±19.75 36.88±6.89 t值 6.547 2.568 4.574 1.065 1.753 P值 < 0.001 0.037 < 0.001 0.321 0.138 -
[1] Portillo MR, Rodríguez-Ortiz ME. Secondary Hyperparthyroidism: Pathogenesis, Diagnosis, Preventive and Therapeutic Strategies[J]. Rev Endocr Metab Disord, 2017, 18(1): 79-95. doi: 10.1007/s11154-017-9421-4
[2] Tominaga Y, Matsuoka S, Uno N. Surgical and medical treatment of secondary hyperparathyroidism in patients on continuous dialysis[J]. World J Surg, 2009, 33(11): 2335-2342. doi: 10.1007/s00268-009-9943-3
[3] Hindié E, Ugur O, Fuster D, et al. 2009 EANM parathyroid guidelines[J]. Eur J Nucl Med Mol Imaging, 2009, 36(7): 1201-1216. doi: 10.1007/s00259-009-1131-z
[4] Clark OH, Duh QY, Kebebew E. Textbook of Endocrine Surgery[M]. 2nd ed. Philadelphia: Elsevier Saunders, 2005: 518.
[5] Kidney Disease: Improving Global Outcomes(KDIGO)CKD-MBD Work Group. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of Chronic Kidney Disease-Mineral and Bone Disorder(CKD-MBD)[J]. Kidney Int Suppl, 2009, 113: S1-130.
[6] 孙海勇, 王田田, 徐先发, 等, 慢性肾功能衰竭患者继发性甲状旁腺功能亢进的外科治疗[J]. 肾脏病及透析肾移植杂志, 2015, 24(4): 337-341. https://www.cnki.com.cn/Article/CJFDTOTAL-SZBY201504007.htm
[7] 宁玉东, 王田田, 薄少军, 等. 磁共振成像在继发性甲状旁腺功能亢进症术前定位的诊断价值[J]. 中国耳鼻咽喉头颈外科, 2017, 24(10): 497-500. https://www.cnki.com.cn/Article/CJFDTOTAL-EBYT201710001.htm
[8] 薄少军, 徐先发, 王田田, 等. 持续性或复发性继发性甲状旁腺功能亢进症的再次手术治疗[J]. 中国血液净化, 2018, 17(1): 35-40. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGJH201801010.htm
[9] 薄少军, 徐先发, 邱传亚, 等. 甲状旁腺切除加部分自体移植术后持续继发性甲状旁腺功能亢进症的外科治疗[J]. 临床耳鼻咽喉头颈外科杂志, 2018, 32(2): 142-147. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201802018.htm
[10] 杨晓琦, 陈安举, 王田田, 等. 继发性甲状旁腺功能亢进甲状旁腺全切术的探讨[J]. 中华耳鼻咽喉头颈外科杂志, 2020, 55(2): 98-103. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGJH202008001.htm
[11] Lokey J, Pattou F, Mondragon-Sanchez A, et al. Intraoperative decay profile of intact(1-84) parathyroid hormone in surgery for secondary hyperparathyroidism in a consecutive series of 50 patients on haemodialysis[J]. Br J Surg, 2000, 87(9): 1256-1278.
[12] 周鹏, 贺青卿, 庄大勇, 等. 持续性和复发性肾性甲状旁腺功能亢进的外科治疗[J]. 中华普通外科杂志, 2019, 34(9): 766-770.
[13] Akerström G, Malmaeus J, Bergström R. Surgical anatomy of human parathyroid glands[J]. Surgery, 1984, 95(1): 14-21.
[14] Karipineni F, Sahli Z, Somervell H, et al. Are preoperative sestamibi scans useful for identifying ectopic parathyroid glands in patients with expected multigland parathyroid disease?[J]. Surgery, 2018, 163(1): 35-41.
[15] 宁玉东, 王田田, 薄少军, 等. 三种影像学检查联用在继发性甲状旁腺功能亢进症术前定位的诊断价值研究[J]. 临床耳鼻咽喉头颈外科杂志, 2017, 31(18): 1408-1411. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201718010.htm
[16] Steinl GK, Kuo JH. Surgical Management of Secondary Hyperparathyroidism[J]. Kidney Int Rep, 2021, 6(2): 254-264.
[17] Polistena A, Sanguinetti A, Lucchini R, et al. Surgical treatment of secondary hyperparathyroidism in elderly patients: an institutional experience[J]. Aging Clin Exp Res, 2017, 29(Suppl 1): 23-28.
[18] Abruzzo A, Gioviale MC, Damiano G, et al. Reoperation for persistent or recurrent secondary hyperparathyroidism[J]. Acta Biomed, 2017, 88(3): 325-328.
[19] Liew V, Gough IR, Nolan G, et al. Re-operation for hyperparathyroidism[J]. ANZ J Surg, 2004, 74(9): 732-740.
[20] Polistena A, Sanguinetti A, Lucchini R, et al. Surgical treatment of secondary hyperparathyroidism in elderly patients: an institutional experience[J]. Aging Clin Exp Res, 2017, 29(Suppl 1): 23-28.
[21] 张一鸣, 蔡相军, 李医明. 甲状腺术中甲状旁腺的识别与保护及术后低钙血症的诊断与治疗[J]. 医学综述, 2018, 24(2): 347-351. https://www.cnki.com.cn/Article/CJFDTOTAL-YXZS201802026.htm
[22] Albuquerque R, Carbonara C, Martin R, et al. Parathyroidectomy in patients with chronic kidney disease: Impacts of different techniques on the biochemical and clinical evolution of secondary hyperparathyroidism[J]. Surgery, 2018, 163(2): 381-387.
[23] Fonseca-Correa JI, Nava-Santana C, Tamez-Pedroza L, et al. Clinical factors associated with early and persistent hypocalcaemia after parathyroidectomy in patients on dialysis with severe hyperparathyroidism[J]. Nephrology(Carlton), 2021, 26(5): 408-419.
[24] Ge P, Liu S, Sheng X, et al. Serum parathyroid hormone and alkaline phosphatase as predictors of calcium requirements after total parathyroidectomy for hypocalcemia in secondary hyperparathyroidism[J]. Head Neck, 2018, 40(2): 324-329.
[25] Chou FF, Lee CH, Chen HY, et al. Persistent and recurrent hyperparathyroidism after total parathyroidectomy with autotransplantation[J]. Ann Surg, 2002, 235(1): 99-104.
-

| 引用本文: | 贾晨晖, 薄少军, 王田田, 等. 继发性甲状旁腺功能亢进术后持续状态的再手术治疗[J]. 临床耳鼻咽喉头颈外科杂志, 2022, 36(11): 822-826. doi: 10.13201/j.issn.2096-7993.2022.11.003 |
| Citation: | JIA Chenhui, BO Shaojun, WANG Tiantian, et al. Reoperation treatment of persistent postoperative secondary hyperparathyroidism[J]. J Clin Otorhinolaryngol Head Neck Surg, 2022, 36(11): 822-826. doi: 10.13201/j.issn.2096-7993.2022.11.003 |
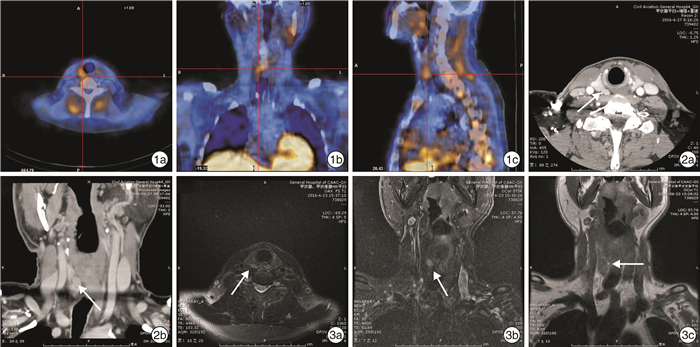
- Figure 1.



 下载:
下载: