Predictive value of strobovideolaryngoscopy, acoustic and aerodynamic measures in the prognosis of temporally unilateral vocal fold paralysis after thyroidectomy
-
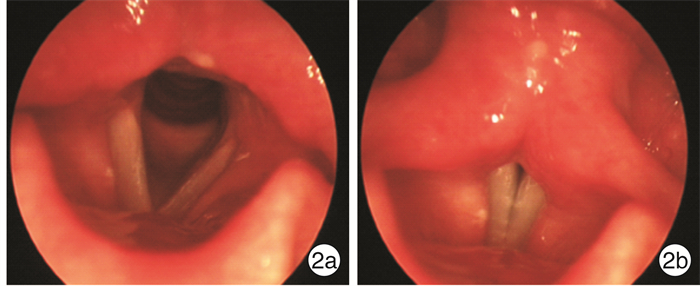
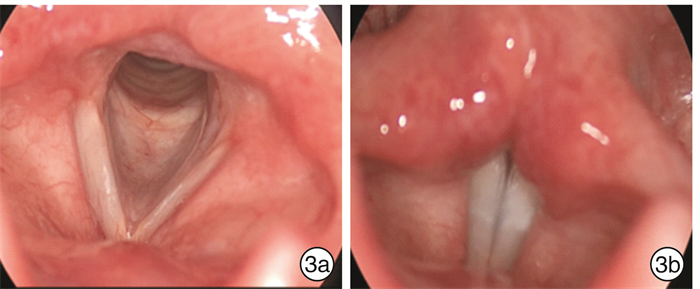
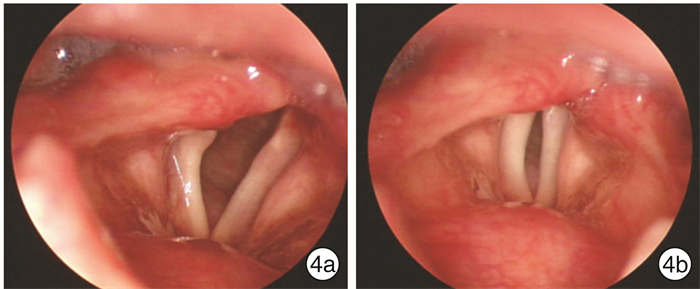
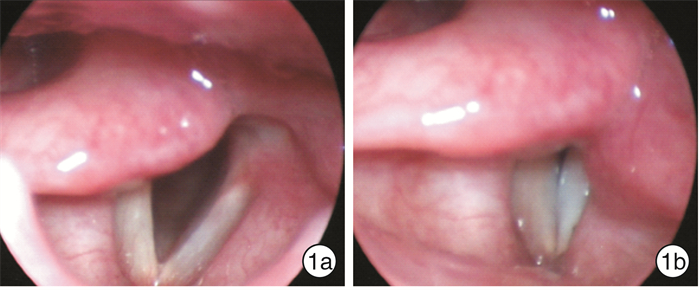
摘要: 目的 探讨甲状腺术后暂时性单侧声带麻痹的频闪喉镜及气流动力学特征。方法 回顾性分析2013年1月-2021年3月就诊于中山大学孙逸仙纪念医院耳鼻咽喉头颈外科的11例甲状腺切除术后暂时性单侧声带麻痹患者;纳入同期8例甲状腺术后永久性单侧声带麻痹患者作为对照组。比较两组基线频闪喉镜声带麻痹评分、声学、气流动力学指标的差异。结果 甲状腺术后暂时性单侧声带麻痹患者音调均正常,出现异形声带(弓形声带、声带萎缩及缩短)、室带内收及中重度声门闭合不全的比例均显著低于永久性声带麻痹患者;杓状软骨稳定性和无声带高度差呈优于永久性声带麻痹的趋势。暂时性声带麻痹患者最长声时(MPT)为(8.5±4.1)s,显著长于永久性声带麻痹患者的(3.9±2.1) s;基频微扰、平均气流量(MeAF)和声门下压(SGP)优于永久性声带麻痹患者,但差异无统计学意义。结论 声门闭合良好或轻度闭合不全,音调正常,无室带内收,无声带萎缩、缩短及弓形声带等异形声带改变,是甲状腺术后暂时性声带麻痹早期的喉镜表现,提示可早期恢复声带运动。MPT小于4 s,MeAF和SGP明显升高是预后不良的气流动力学表现。Abstract: Objective To investigate the strobovideolaryngoscopy, acoustic and aerodynamic characteristics of transient unilateral vocal ford paralysis(UVFP) after thyroidectomy.Methods A retrospective analysis was made of 11 patients with temporary UVFP after thyroidectomy who were treated in Department of Otolaryngology and Head and Neck Surgery, Sun Yat-sen Memorial Hospital, Sun Yat-sen University from January 2013 to March 2021; 8 patients with permanent UVFP after thyroidectomy during the same period were included as a control group. The differences in baseline strobovideolaryngoscopy, acoustic and aerodynamic measures were compared between the two groups.Results The tones of patients with temporary UVFP after thyroidectomy were all normal, and the proportions of abnormal vocal fords(vocal ford bowing, atrophy, and shortening), ventricular adduction and glottic insufficiency were significantly lower than those of permanent UVFP patients; arytenoid cartilage stability and height mismatch of vocal ford tended to be better than permanent UVFP. The maximal phonation time(MPT) in patients with temporary UVFP was (8.5±4.1) s, which was significantly longer than (3.9±2.1) s in patients with permanent UVFP; fundamental frequency, mean airflow(MeAF) and mean subglottic pressure(SGP) were better in temporary UVFP than those in patients with permanent UVFP, but the difference did not reach statistical significance.Conclusion None and mild glottic insufficiency, normal tone, ventricular adduction, and vocal ford appearances without vocal fold bowing, atrophy, and shortening, can be served as the predictors for the early recovery of vocal ford movement in temporary UVFP after thyroidectomy. The MPT less than 4 s, and MeAF, and SGP remarkably increased is the predictor of poor prognosis for vocal ford recovery.
-

-
表 1 甲状腺术后暂时性麻痹组和对照组患者声带麻痹评分的比较
指标 暂时性麻痹组
(n=11)对照组
(n=8)P值 自主内收活动(有∶部分/无) 0∶11 0∶8 - 黏膜波(正常∶部分/无) 2∶9 0∶8 0.202 杓状软骨稳定性(正常∶部分受损/消失) 10;1 5∶3 0.134 杓状软骨位置(正常∶移位) 7∶4 4∶4 0.552 音调(正常∶下降) 11∶0 5∶3 0.027 声带萎缩(无∶有) 11∶0 6∶2 0.080 弓形声带(无∶有) 10∶1 4∶4 0.046 声带缩短(无∶有) 10∶1 4∶4 0.046 唾液积聚(无∶有) 10∶1 7∶1 0.811 声带高度差(无∶有) 9∶2 4∶4 0.141 室带内收(无∶有) 10∶1 4∶4 0.046 声门闭合不全(无/轻度∶中度/重度) 10∶1 0∶8 <0.001 表 2 甲状腺术后暂时性声带麻痹组和对照组患者声学和空气动力学参数的比较
组别 F0/Hz jitter/% shimmer/% MPT/s MeAF/(L·s-1) SGP/cm H2O 暂时麻痹组 213.1±43.5 3.1±2.7 7.1±3.2 8.5±4.1 0.45±0.38 7.8±3.4 对照组 200.6±72.2 6.2±5.9 9.4±5.0 3.9±2.1 0.72±0.36 11.4±5.5 P值 0.642 0.132 0.243 0.010 0.158 0.138 -
[1] Bergenfelz A, Salem AF, Jacobsson H, et al. Risk of recurrent laryngeal nerve palsy in patients undergoing thyroidectomy with and without intraoperative nerve monitoring[J]. Br J Surg, 2016, 103(13): 1828-1838. doi: 10.1002/bjs.10276
[2] Sancho JJ, Pascual-Damieta M, Pereira JA, et al. Risk factors for transient vocal cord palsy after thyroidectomy[J]. Br J Surg, 2008, 95(8): 961-967. doi: 10.1002/bjs.6173
[3] Chiang FY, Lu IC, Kuo WR, et al. The mechanism of recurrent laryngeal nerve injury during thyroid surgery——the application of intraoperative neuromonitoring[J]. Surgery, 2008, 143(6): 743-749. doi: 10.1016/j.surg.2008.02.006
[4] Tsuzuki N, Wasano K, Kawasaki T, et al. Thyroid lobe size predicts risk of postoperative temporary recurrent laryngeal nerve paralysis[J]. Laryngoscope Investig Otolaryngol, 2019, 4(6): 708-713. doi: 10.1002/lio2.321
[5] Sitges-Serra A, Gallego-Otaegui L, Fontané J, et al. Contralateral surgery in patients scheduled for total thyroidectomy with initial loss or absence of signal during neural monitoring[J]. Br J Surg, 2019, 106(4): 404-411. doi: 10.1002/bjs.11067
[6] Dhillon VK, Rettig E, Noureldine SI, et al. The incidence of vocal fold motion impairment after primary thyroid and parathyroid surgery for a single high-volume academic surgeon determined by pre-and immediate post-operative fiberoptic laryngoscopy[J]. Int J Surg, 2018, 56: 73-78. doi: 10.1016/j.ijsu.2018.06.014
[7] 中华耳鼻咽喉头颈外科杂志编辑委员会咽喉组, 中华医学会耳鼻咽喉头颈外科学分会嗓音学组, 中华医学会耳鼻咽喉头颈外科学分会咽喉学组, 等. 喉白斑诊断与治疗专家共识[J]. 中华耳鼻咽喉头颈外科杂志, 2018, 53(8): 564-569. doi: 10.3760/cma.j.issn.1673-0860.2018.08.002
[8] Rosow DE, Sulica L. Laryngoscopy of vocal fold paralysis: evaluation of consistency of clinical findings[J]. Laryngoscope, 2010, 120(7): 1376-1382. doi: 10.1002/lary.20945
[9] Bakhsh Z, Crevier-Buchman L. Stroboscopic assessment of unilateral vocal fold paralysis: a systematic review[J]. Eur Arch Otorhinolaryngol, 2019, 276(9): 2377-2387. doi: 10.1007/s00405-019-05562-x
[10] Benninger MS, Crumley RL, Ford CN, et al. Evaluation and treatment of the unilateral paralyzed vocal fold[J]. Otolaryngol Head Neck Surg, 1994, 111(4): 497-508. doi: 10.1177/019459989411100419
[11] Desuter G, Dedry M, Schaar B, et al. Voice outcome indicators for unilateral vocal fold paralysis surgery: a review of the literature[J]. Eur Arch Otorhinolaryngol, 2018, 275(2): 459-468. doi: 10.1007/s00405-017-4844-9
-



 下载:
下载: