Serum 25-hydroxyvitamin D expression and its correlation in patients with vestibular neuritis
-
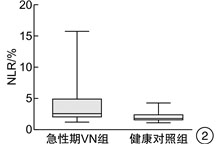
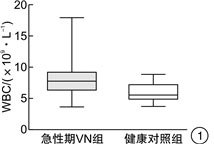
摘要: 目的 探讨前庭神经炎(VN)患者血清25-羟维生素D[25-(OH)D]的表达水平及其相关性。方法 选取2020年10月-2021年10月在山西医科大学第一医院耳鼻咽喉头颈外科就诊的符合纳入、排除标准的30例急性期VN患者和50例年龄、性别匹配的健康对照者。记录所有受试者的人口统计学数据和临床数据,测量和比较血清25-(OH)D水平和炎症指标水平,并追踪VN患者恢复期(3个月后)血清25-(OH)D水平的变化情况。结果 急性期VN组的血清25-(OH)D水平明显低于健康对照组[(10.14±2.92) ng/mL和(20.61±4.70) ng/mL,P < 0.01],缺乏率100.0%(30/30)明显高于对照组54.0%(27/50)。且VN患者恢复期(3个月后)血清25-(OH)D水平较急性期明显升高[(10.14±2.92) ng/mL和(15.94±4.88) ng/mL,P < 0.01],缺乏率76.7%(23/30)明显降低。但无论是急性期还是恢复期,VN组的血清25-(OH)D水平均明显低于对照组,缺乏率均明显高于对照组。多因素二元logistic回归模型分析显示低水平血清25-(OH)D与VN的发病相关,OR值为0.193(95%CI=0.043~0.861,P=0.031)。此外,本研究结果显示急性期VN组的外周血白细胞(WBC)和中性粒细胞/淋巴细胞比率(NLR)水平均明显高于对照组[(7.65±3.02)×109/L和(5.50±2.50)×109/L,P < 0.01;(2.46±2.95)×100%和(1.67±0.92)×100%,P < 0.01)],两组的血小板/淋巴细胞比率(PLR)和血小板平均体积(MPV)水平差异无统计学意义(P>0.05)。两组的年龄分布、性别比、体重指数、持续健康问题或生活方式方面差异均无统计学意义(P>0.05)。结论 本研究首次对急性期VN患者进行血清25-(OH)D水平和炎症指标水平的同步检测,并动态评估VN患者不同阶段的血清25-(OH)D水平,发现低水平血清25-(OH)D与VN的发病相关,生理浓度下的血清25-(OH)D是VN的保护性因素,维生素D补充治疗可能成为VN治疗的新靶点。Abstract: Objective To investigate the expression level of serum 25-(OH) D and its correlation in patients with vestibular neuritis(VN).Methods 30 acute VN patients and 50 age-and sex-matched healthy controls who attended the Otolaryngology, Head and Neck Surgery Department of the First Hospital of Shanxi Medical University from October 2020 to October 2021 were selected. The demographic and clinical data of all subjects were recorded, the levels of serum 25-(OH) D and inflammatory markers were measured and compared, and the changes of serum 25-(OH) D levels in convalescent patients with VN were followed up.Results The serum level of 25-(OH) D in the acute phase VN group was significantly lower than that in healthy controls[(10.14±2.92) ng/mL vs (20.61±4.70) ng/mL, P < 0.01], and the deficiency rate of 100.0%(30/30) was significantly higher than 54.0%(27/50). Moreover, the serum level of 25-(OH) D in the recovery period(3 months later) was significantly higher[(10.14±2.92) ng/mL vs (15.94±4.88) ng/mL, P < 0.01], and the deficiency rate was significantly decreased by 76.7%(23/30). However, the serum 25-(OH) D level was significantly lower in both the VN group than that in both the acute period and the recovery group, and the deficiency rate was significantly higher than that in the control group. Multivariate binary Logistic regression model analysis showed that low-level serum 25-(OH) D was associated with the onset of VN, with an OR value of 0.193(95%CI=0.043-0.861, P=0.031). In addition, the results of this study showed that peripheral blood leukocyte(WBC) and neutrophil / lymphocyte ratio(NLR) levels in the acute VN group were significantly higher than in healthy controls[(7.65±3.02) ×109/L vs (5.50±2.50) ×109/L, P < 0.01; (2.46±2.95) ×100% vs(1.67±0.92) ×100%, P < 0.01], and there was no significant difference in Platelet / lymphocyte ratio(PLR) and and average platelet volume(MPV) levels in the two groups(P>0.05). There were no significant differences in age distribution, sex ratio, body mass index, persistent health problems, or lifestyle groups(P>0.05).Conclusion This study is the first to detect serum 25-(OH) D level and inflammation index level, and dynamically assess the serum 25-(OH) D level in different stages, found that low serum 25-(OH) D is associated with the onset of VN, physiological concentration of serum 25-(OH) D is a protective factor of VN, vitamin D supplementation therapy may be a new target of VN treatment.
-
Key words:
- vestibular neuritis /
- 25-hydroxyvitamin D /
- immune inflammatory response
-

-
表 1 急性期VN组和对照组人口统计和生化特征
项目 急性期VN组(n=30) 对照组(n=50) P值 年龄/岁 45.00±19.23 51.48±12.47 0.106 性别(男/女)/例 14/16 17/33 0.260 BMI/(kg·m-2) 23.55±3.58 23.81±3.70 0.766 高血压/例(%) 8(26.7) 15(30.0) 0.750 糖尿病/例(%) 4(13.3) 10(20.0) 0.447 吸烟/例(%) 4(13.3) 5(10.0) 0.927 饮酒/例(%) 3(10.0) 2(4.0) 0.551 TC/mmol·L-1 4.32±0.89 4.42±0.85 0.637 TG/mmol·L-1 1.38±0.90 1.23±0.83 0.128* HDL-C/(mmol·L-1) 1.12±0.24 1.18±0.26 0.309 LDL-C/(mmol·L-1) 2.55±0.59 2.72±0.71 0.272 WBC/(×109·L-1) 7.65±3.02 5.50±2.50 <0.001* NLR/% 2.46±2.95 1.67±0.92 <0.001* PLR/% 133.49±82.52 139.72±59.70 0.531* MPV/fL 9.80±1.64 10.04±1.51 0.502 注:*计量资料数据不符合正态分布,采用中位数±四分位间距表示,P < 0.05为差异有统计学意义。 表 2 多因素二元logistic回归分析确定VN的独立危险因素
变量 B SE Wald OR 95% CI P值 年龄 -0.114 0.081 1.985 0.892 0.761-1.046 0.159 BMI -0.801 0.557 2.069 0.449 0.151-1.337 0.150 血清25-(OH)D -1.643 0.762 4.652 0.193 0.043-0.861 0.031 注:多因素二元logistic回归分析模型包括年龄、性别、BMI、糖尿病、高血压、血脂、血清25-(OH)D。Nagelkerke R方值为0.924,Hosmer-Lemeshow检验卡方值为5.506,P=0.702。 -
[1] 李斐, 鞠奕, 张甦琳, 等. 前庭神经炎诊治多学科专家共识[J]. 中华老年医学杂志, 2020, 39(9): 985-994. doi: 10.3760/cma.j.issn.0254-9026.2020.09.001
[2] Le TN, Westerberg BD, Lea J. Vestibular Neuritis: Recent Advances in Etiology, Diagnostic Evaluation, and Treatment[J]. Adv Otorhinolaryngol, 2019, 82: 87-92.
[3] Himmelein S, Lindemann A, Sinicina I, et al. Differential Involvement during Latent Herpes Simplex Virus 1 Infection of the Superior and Inferior Divisions of the Vestibular Ganglia: Implications for Vestibular Neuritis[J]. J Virol, 2017, 91(14).
[4] Arbusow V, Derfuss T, Held K, et al. Latency of herpes simplex virus type-1 in human geniculate and vestibular ganglia is associated with infiltration of CD8+ T cells[J]. J Med Virol, 2010, 82(11): 1917-1920. doi: 10.1002/jmv.21904
[5] Bartual-Pastor J. Vestibular neuritis: etiopathogenesis[J]. Rev Laryngol Otol Rhinol(Bord), 2005, 126(4): 279-281.
[6] Freedman JE, Loscalzo J. Platelet-monocyte aggregates: bridging thrombosis and inflammation[J]. Circulation, 2002, 105(18): 2130-2132. doi: 10.1161/01.CIR.0000017140.26466.F5
[7] Kassner SS, Schöttler S, Bonaterra GA, et al. Proinflammatory activation of peripheral blood mononuclear cells in patients with vestibular neuritis[J]. Audiol Neurootol, 2011, 16(4): 242-247. doi: 10.1159/000320839
[8] Bikle D. Nonclassic actions of vitamin D[J]. J Clin Endocrinol Metab, 2009, 94(1): 26-34. doi: 10.1210/jc.2008-1454
[9] Muñoz Garcia A, Kutmon M, Eijssen L, et al. Pathway analysis of transcriptomic data shows immunometabolic effects of vitamin D[J]. J Mol Endocrinol, 2018, 60(2): 95-108. doi: 10.1530/JME-17-0186
[10] Reins RY, McDermott AM. Vitamin D: Implications for ocular disease and therapeutic potential[J]. Exp Eye Res, 2015, 134: 101-110. doi: 10.1016/j.exer.2015.02.019
[11] Uberti F, Lattuada D, Morsanuto V, et al. Vitamin D protects human endothelial cells from oxidative stress through the autophagic and survival pathways[J]. J Clin Endocrinol Metab, 2014, 99(4): 1367-1374. doi: 10.1210/jc.2013-2103
[12] Bikle DD. Vitamin D and immune function: understanding common pathways[J]. Curr Osteoporos Rep, 2009, 7(2): 58-63. doi: 10.1007/s11914-009-0011-6
[13] Wei R, Christakos S. Mechanisms Underlying the Regulation of Innate and Adaptive Immunity by Vitamin D[J]. Nutrients, 2015, 7(10): 8251-8260. doi: 10.3390/nu7105392
[14] Baecher-Allan C, Kaskow BJ, Weiner HL. Multiple Sclerosis: Mechanisms and Immunotherapy[J]. Neuron, 2018, 97(4): 742-768. doi: 10.1016/j.neuron.2018.01.021
[15] Abdelmaksoud AA, Fahim D, Bazeed S, et al. Relation between vitamin D deficiency and benign paroxysmal positional vertigo[J]. Sci Rep, 2021, 11(1): 16855. doi: 10.1038/s41598-021-96445-x
[16] Jeong SH, Kim JS, Shin JW, et al. Decreased serum vitamin D in idiopathic benign paroxysmal positional vertigo[J]. J Neurol, 2013, 260(3): 832-838. doi: 10.1007/s00415-012-6712-2
[17] Büki B, Jünger H, Lundberg YW. Vitamin D supplementation may improve symptoms in Meniere's disease[J]. Med Hypotheses, 2018, 116: 44-46. doi: 10.1016/j.mehy.2018.04.019
[18] Jeong SH, Kim JS, Kim HJ, et al. Prevention of benign paroxysmal positional vertigo with vitamin D supplementation: A randomized trial[J]. Neurology, 2020, 95(9): e1117-e1125. doi: 10.1212/WNL.0000000000010343
[19] Jeong SH, Lee SU, Kim JS. Prevention of recurrent benign paroxysmal positional vertigo with vitamin D supplementation: a meta-analysis[J]. J Neurol, 2022, 269(2): 619-626. doi: 10.1007/s00415-020-09952-8
[20] Greco A, Macri GF, Gallo A, et al. Is vestibular neuritis an immune related vestibular neuropathy inducing vertigo?[J]. J Immunol Res, 2014, 2014: 459048.
[21] Byun H, Chung JH, Lee SH, et al. Clinical value of 4-hour delayed gadolinium-Enhanced 3D FLAIR MR Images in Acute Vestibular Neuritis[J]. Laryngoscope, 2018, 128(8): 1946-1951. doi: 10.1002/lary.27084
[22] Fattori B, Ursino F, Cristofani R, et al. Relevance of plasma D-dimer measurement in patients with acute peripheral vertigo[J]. J Laryngol Otol, 2003, 117(6): 467-472. doi: 10.1258/002221503321892316
[23] Milionis HJ, Mittari V, Exarchakos G, et al. Lipoprotein(a)and acute-phase response in patients with vestibular neuronitis[J]. Eur J Clin Invest, 2003, 33(12): 1045-1050. doi: 10.1111/j.1365-2362.2003.01275.x
[24] Chung JH, Lim J, Jeong JH, et al. The significance of neutrophil to lymphocyte ratio and platelet to lymphocyte ratio in vestibular neuritis[J]. Laryngoscope, 2015, 125(7): E257-E261. doi: 10.1002/lary.25204
[25] Büki B, Jünger H, Zhang Y, et al. The Price of Immune Responses and the Role of Vitamin D in the Inner Ear[J]. Otol Neurotol, 2019, 40(6): 701-709. doi: 10.1097/MAO.0000000000002258
[26] Oh EH, Rhee JK, Shin JH, et al. Neutrophil-mediated immune response as a possible mechanism of acute unilateral vestibulopathy[J]. J Vestib Res, 2020, 30(6): 363-374. doi: 10.3233/VES-200044
[27] Solis RN, Sun DQ, Tatro E, et al. Do steroids improve recovery in vestibular neuritis?[J]. Laryngoscope, 2019, 129(2): 288-290. doi: 10.1002/lary.27278
[28] 李秀花, 孟萌, 宋江曼, 等. 前庭神经炎患者25羟维生素D和C反应蛋白水平的研究[J]. 中风与神经疾病杂志, 2021, 38(9): 829-832. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFSJ202109016.htm
[29] Schwalfenberg GK. A review of the critical role of vitamin D in the functioning of the immune system and the clinical implications of vitamin D deficiency[J]. Mol Nutr Food Res, 2011, 55(1): 96-108. doi: 10.1002/mnfr.201000174
[30] Zhang Y, Leung DY, Richers BN, et al. Vitamin D inhibits monocyte/macrophage proinflammatory cytokine production by targeting MAPK phosphatase-1[J]. J Immunol, 2012, 188(5): 2127-2135. doi: 10.4049/jimmunol.1102412
[31] Townsend K, Evans KN, Campbell MJ, et al. Biological actions of extra-renal 25-hydroxyvitamin D-1alpha-hydroxylase and implications for chemoprevention and treatment[J]. J Steroid Biochem Mol Biol, 2005, 97(1-2): 103-109.
[32] Calton EK, Keane KN, Soares MJ. The potential regulatory role of vitamin D in the bioenergetics of inflammation[J]. Curr Opin Clin Nutr Metab Care, 2015, 18(4): 367-373. doi: 10.1097/MCO.0000000000000186
[33] Adorini L, Penna G, Giarratana N, et al. Tolerogenic dendritic cells induced by vitamin D receptor ligands enhance regulatory T cells inhibiting allograft rejection and autoimmune diseases[J]. J Cell Biochem, 2003, 88(2): 227-233. doi: 10.1002/jcb.10340
[34] Yamamoto E, Jørgensen TN. Immunological effects of vitamin D and their relations to autoimmunity[J]. J Autoimmun, 2019, 100: 7-16. doi: 10.1016/j.jaut.2019.03.002
[35] Minasyan A, Keisala T, Zou J, et al. Vestibular dysfunction in vitamin D receptor mutant mice[J]. J Steroid Biochem Mol Biol, 2009, 114(3-5): 161-166.
[36] Wu Y, Hu Z, Cai M, et al. Decreased 25-Hydroxyvitamin D Levels in Patients With Vestibular Neuritis. [J]. Front Neurol, 2019, 10: 863. doi: 10.3389/fneur.2019.00863
-




 下载:
下载: