Effectiveness of transoral endoscopic thyroid surgery for lymph node dissection in the central region of thyroid cancer
-
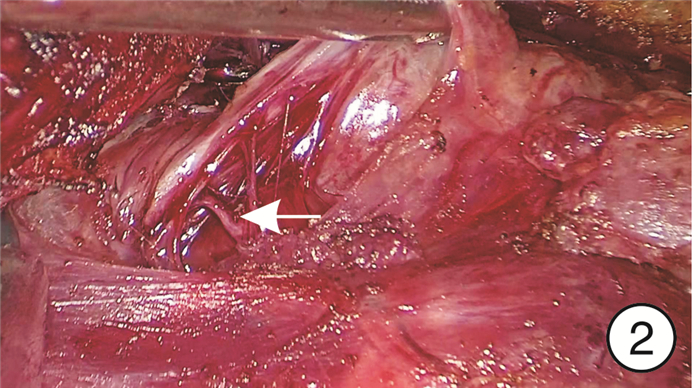
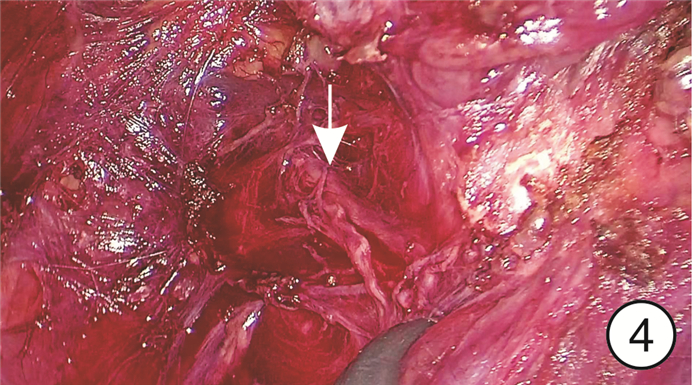
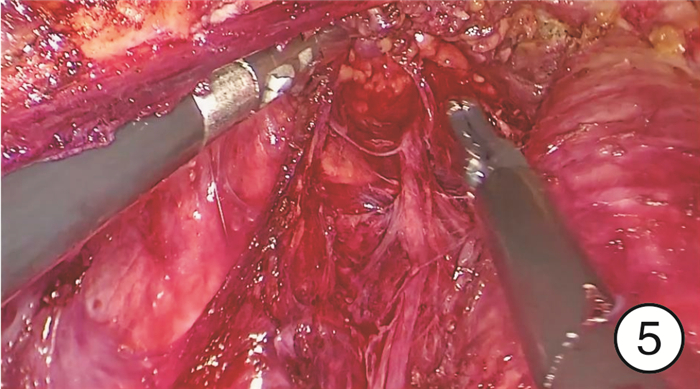
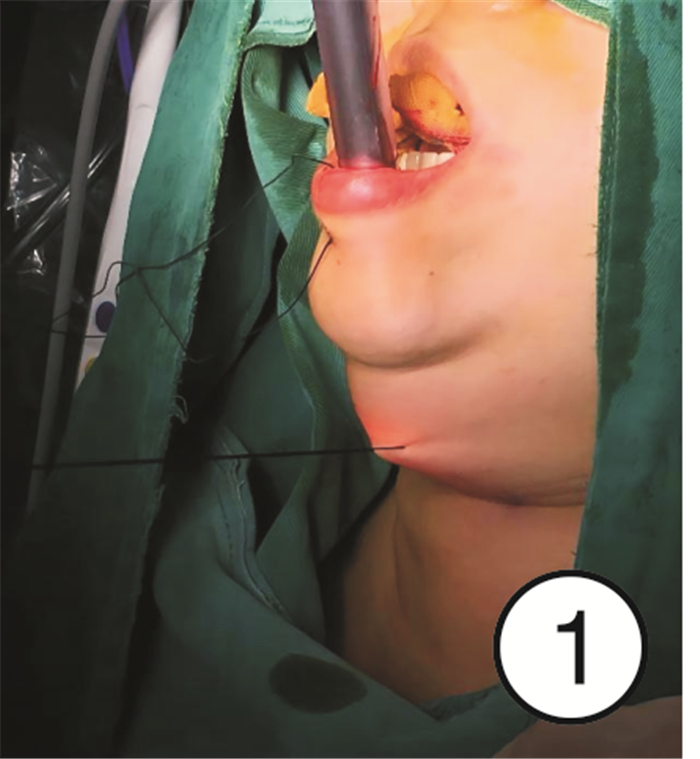
摘要: 目的 探讨经口腔前庭入路腔镜手术在甲状腺癌中央区淋巴结清扫中的效果。方法 根据纳入标准,确定行经口腔前庭入路腔镜甲状腺手术(TOETVA)患者20例(TOETVA组),在同样标准下,按照性别、年龄匹配行传统开放甲状腺手术患者20例(开放组),收集分析两组患者的临床资料、手术相关数据、淋巴结清扫数及术后并发症。采用SPSS 24.0统计软件进行数据分析。结果 TOETVA组和开放组患者的年龄、BMI、肿瘤大小及桥本甲状腺炎患者数的差异均无统计学意义(P>0.05);TOETVA组的手术时间[(117.30±10.54) min]及术后引流量[(146.05±30.66) mL]显著高于开放组[(59.05±6.40) min,(77.90±22.18) mL],均P < 0.001。开放组患者术后24 h疼痛较TOETVA组更强烈(P < 0.05)。两组清扫的总中央组淋巴结数目、喉前淋巴结数目及气管前淋巴结数目相似,最终阳性淋巴结数目无明显差异; 但TOETVA组清扫的气管旁淋巴结数目[(7.8±4.2)枚]较开放组[(6.4±3.9)枚]更多,P < 0.05。两组术后并发症的差异无统计学意义。TOETVA组患者术后6个月瘢痕美容评估与评级得分(0.77±0.58)明显低于开放组(4.30±1.54),P < 0.001。结论 在中央区淋巴结清扫中,TOETVA与传统开放甲状腺手术的清扫效率相似,对于特殊解剖区域,腔镜手术效率更高; 同时TOETVA不增加相关并发症发生率,且美容效果好。Abstract: Objective To investigate the effect of transoral endoscopic thyroid surgery in the central lymph node dissection of thyroid cancer.Methods Twenty patients underwent endoscopic thyroidectomy via oral vestibular approach (TOETVA group) and 20 gender and age matched patients underwent conventional open thyroidectomy were selected in this study. The clinical data, number of lymph node dissection and postoperative complications of the two groups were collected and analyzed. SPSS 24.0 statistical software was used for data analysis.Results There was no significant differences in age, BMI, tumor size or the number of Hashimoto's thyroiditis patients between the TOETVA group and the open group(P>0.05). The operation time([117.30±10.54]min) and postoperative drainage volume([146.05±30.66]mL) in the TOETVA group were significantly higher than those in the open group([59.05±6.40]min, [77.90±22.18]mL), P < 0.001. The pain in the open group 24 h after surgery was more severe than that in the TOETVA group(P < 0.05). The total number of central lymph nodes, the number of pre-laryngeal lymph nodes and the number of pre-tracheal lymph nodes cleared by the two groups were similar, and the number of final positive lymph nodes had no significant difference. However, the number of paratracheal lymph nodes removed in the TOETVA group was more(7.8±4.2) nodes than that in the open group(6.4±3.9) nodes, P < 0.05. There was no significant difference in postoperative complications between the two groups. The scores of cosmetic evaluation and rating of cicatrices in the TOETVA group six months after surgery were(0.77±0.58) significantly lower than those in the open group(4.30±1.54), P < 0.001.Conclusion In central lymph node dissection, the efficiency of TOETVA is similar to that of traditional open thyroid surgery. For special anatomical regions, endoscopic surgery is more efficient. At the same time, TOETVA does not increase the incidence of related complications, and has good cosmetic effect.
-

-
表 1 两组患者手术相关信息及并发症比较
TOETVA组(n=20) 开放组(n=20) P值 手术时间/min 117.30±10.54 59.05±6.40 < 0.001 术后引流量/mL 146.05±30.66 77.90±22.18 < 0.001 住院天数/d 5.0±0.79 5.2±1.10 0.515 并发症/例(%) 术口感染 1(5) 0(0) 0.311 暂时性声带麻痹 1(5) 2(10) 0.548 暂时性甲状旁腺功能低下 0(0) 3(15) 0.231 甲状旁腺误切 0(0) 1(5) 0.311 颏神经损伤 1(5) 0(0) 0.311 VAS评分(术后24 h) 7.10±1.21 7.95±1.15 0.028 表 2 两组淋巴结清扫比较
枚,X±S TOETVA组(n=20) 开放组(n=20) P值 总中央组淋巴结数目 12.2±8.5 10.3±7.2 0.121 转移淋巴结数目 4.1±1.2 4.0±0.9 0.627 气管前淋巴结数目 3.1±1.3 2.9±0.8 0.407 喉前淋巴结数目 2.3±1.0 2.0±0.6 0.201 气管旁淋巴结数目 7.8±4.2 6.4±3.9 0.037 表 3 术后Ca2+及PTH比较
X±S TOETVA组(n=20) 开放组(n=20) P值 Ca2+/(mmol·L-1) 2.33±1.45 2.34±1.44 0.853 PTH/(pg·mL-1) 术后1 d 17.64±1.79 17.45±3.12 0.815 术后3个月 27.79±4.22 29.01±3.23 0.314 -
[1] Wang TS, Sosa JA. Thyroid surgery for differentiated thyroid cancer-recent advances and future directions[J]. Nat Rev Endocrinol, 2018, 14(11): 670-683. doi: 10.1038/s41574-018-0080-7
[2] Davies L, Hoang JK. Thyroid cancer in the USA: current trends and outstanding questions[J]. Lancet Diabetes Endocrinol, 2021, 9(1): 11-12. doi: 10.1016/S2213-8587(20)30372-7
[3] Sosa JA, Hanna JW, Robinson KA, et al. Increases in thyroid nodule fine-needle aspirations, operations, and diagnoses of thyroid cancer in the United States[J]. Surgery, 2013, 154(6): 1420-1427. doi: 10.1016/j.surg.2013.07.006
[4] Qu N, Zhang L, Ji QH, et al. Risk Factors for Central Compartment Lymph Node Metastasis in Papillary Thyroid Microcarcinoma: A Meta-Analysis[J]. World J Surg, 2015, 39(10): 2459-2470. doi: 10.1007/s00268-015-3108-3
[5] Lundgren CI, Hall P, Dickman PW, et al. Clinically significant prognostic factors for differentiated thyroid carcinoma: a population-based, nested case-control study[J]. Cancer, 2006, 106(3): 524-531. doi: 10.1002/cncr.21653
[6] Choi Y, Lee JH, Kim YH, et al. Impact of postthyroidectomy scar on the quality of life of thyroid cancer patients[J]. Ann Dermatol, 2014, 26(6): 693-699. doi: 10.5021/ad.2014.26.6.693
[7] Razavi CR, Khadem M, Fondong A, et al. Early outcomes in transoral vestibular thyroidectomy: Robotic versus endoscopic techniques[J]. Head Neck, 2018, 40(10): 2246-2253. doi: 10.1002/hed.25323
[8] Camenzuli C, Schembri Wismayer P, Calleja Agius J. Transoral Endoscopic Thyroidectomy: A Systematic Review of the Practice So Far[J]. JSLS, 2018, 22(3): e2018.00026. doi: 10.4293/JSLS.2018.00026
[9] 王平, 吴国洋, 田文, 等. 经口腔前庭入路腔镜甲状腺手术专家共识(2018版)[J]. 中国实用外科杂志, 2018, 38(10): 1104-1107. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGWK201810002.htm
[10] Yi JW, Yoon SG, Kim HS, et al. Transoral endoscopic surgery for papillary thyroid carcinoma: initial experiences of a single surgeon in South Korea[J]. Ann Surg Treat Res, 2018, 95(2): 73-79. doi: 10.4174/astr.2018.95.2.73
[11] Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer[J]. Thyroid, 2016, 26(1): 1-133. doi: 10.1089/thy.2015.0020
[12] 王存川, 翟贺宁, 刘卫军, 等. 经口腔前庭腔镜甲状腺切除术6例经验[J]. 中国内镜杂志, 2013, 19(4): 363-366. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGNJ201304008.htm
[13] Russell JO, Razavi CR, Shaear M, et al. Transoral Vestibular Thyroidectomy: Current State of Affairs and Considerations for the Future[J]. J Clin Endocrinol Metab, 2019, 104(9): 3779-3784. doi: 10.1210/jc.2019-00116
[14] Razavi CR, Fondong A, Tufano RP, et al. Central neck dissection via the transoral approach[J]. Ann Thyroid, 2017, 2(5): 11.
[15] Hong YT, Ahn JH, Kim JH, et al. Bi-institutional experience of transoral endoscopic thyroidectomy: Challenges and outcomes[J]. Head Neck, 2020, 42(8): 2115-2122. doi: 10.1002/hed.26153
[16] Sun H, Zheng H, Wang X, et al. Comparison of transoral endoscopic thyroidectomy vestibular approach, total endoscopic thyroidectomy via areola approach, and conventional open thyroidectomy: a retrospective analysis of safety, trauma, and feasibility of central neck dissection in the treatment of papillary thyroid carcinoma[J]. Surg Endosc, 2020, 34(1): 268-274. doi: 10.1007/s00464-019-06762-6
[17] Russell JO, Clark J, Noureldine SI, et al. Transoral thyroidectomy and parathyroidectomy-A North American series of robotic and endoscopic transoral approaches to the central neck[J]. Oral Oncol, 2017, 71: 75-80. doi: 10.1016/j.oraloncology.2017.06.001
[18] Wang T, Wu Y, Xie Q, et al. Safety of central compartment neck dissection for transoral endoscopic thyroid surgery in papillary thyroid carcinoma[J]. Jpn J Clin Oncol, 2020, 50(4): 387-391. doi: 10.1093/jjco/hyz195
[19] Anuwong A, Ketwong K, Jitpratoom P, et al. Safety and Outcomes of the Transoral Endoscopic Thyroidectomy Vestibular Approach[J]. JAMA Surg, 2018, 153(1): 21-27. doi: 10.1001/jamasurg.2017.3366
[20] Roh MR. The SCAR(Scar Cosmesis Assessment and Rating)scale: new evaluation method for postoperative scars[J]. Br J Dermatol, 2016, 175(6): 1151-1152. doi: 10.1111/bjd.14989
[21] Kantor J. Reliability and Photographic Equivalency of the Scar Cosmesis Assessment and Rating(SCAR)Scale, an Outcome Measure for Postoperative Scars[J]. JAMA Dermatol, 2017, 153(1): 55-60. doi: 10.1001/jamadermatol.2016.3757
[22] Kuo TC, Duh QY, Wang YC, et al. Practice Patterns and Learning Curve in Transoral Endoscopic Thyroidectomy Vestibular Approach With Neuromonitoring[J]. Front Endocrinol(Lausanne), 2021, 12: 744359. doi: 10.3389/fendo.2021.744359
-




 下载:
下载: