-
摘要: 目的 总结儿童先天性鳃裂畸形CT特征性表现,以减少误诊和指导制定手术方案。方法 回顾性分析上海市儿童医院2014年8月-2021年1月收入院并经手术和病理确诊的先天性第1鳃裂畸形(CFBCA)、先天性第2鳃裂畸形(CSBCAs)、先天性梨状窝瘘(CPSF)的患儿CT影像学资料。结果 共收集儿童先天性鳃裂畸形323例,其中CFBCA 119例(119/323,36.8%),96例(96/119,80.67%)与外耳道壁相关,89例(89/119,74.78%)与腮腺相关,CT检查阳性率87.4%(104/119);CSBCAs 57例(57/323,17.6%),其中46例(46/57,80.7%)与下颌下腺相关,CT检查阳性率84.2%(48/57);CPSF147例(147/323,45.5%),其中129例(129/147,87.8%)与甲状腺相关,CT检查阳性率89.1%(131/147)。结论 CFBCA的CT特征性表现为病灶位于同侧外耳道(底、后)壁及腮腺,CSBCAs的CT特征性表现为病灶位于同侧下颌下腺(后、内)侧,CPSF的CT特征性表现为病灶位于甲状腺侧叶上极背侧。
-
关键词:
- 儿童 /
- 先天性鳃裂畸形 /
- 体层摄影术,X线计算机
Abstract: Objective To summarize the CT features of congenital branchial cleft anomaly in children, to reduce misdiagnosis and improve surgical strategy.Methods This study enrolled 323 pediatric patients with congenital first branchial cleft anomaly, congenital second branchial cleft anomaly and congenital piriform sinus fistula confirmed by surgery and post-operative histopathology, who was admitted to Shanghai Children's hospital from August 2014 to January 2021., CT imaging data were retrospectively analyzed.Results A total of 323 children with congenital branchial cleft deformity were included. There were 145 males and 178 females, aged from 22 days to 15 years. 119(119/323, 36.8%) cases were diagnosed as congenital first branchial cleft anomaly. Among them, 96 cases(96/119, 80.67%) were related to the wall of external auditory canal, and 89 cases(89/119, 74.78%) were related to parotid gland. The positive rate of CT examination was 87.4%(104/119). 57 cases(57 / 323, 17.6%) had congenital second branchial cleft anomaly. Among them, 46 cases(46/57, 80.7%) were related to submandibular gland. The positive rate of CT examination was 84.2%(48/57). 147 cases(147/323, 45.5%) had congenital piriform sinus fistula, in which 129 cases(129/147, 87.8%) were related to thyroid. The positive rate of CT was 89.1%(131/147).Conclusion The CT findings of congenital first branchial cleft anomaly are characterized by lesions in the inferior and/or posterior wall of ipsilateral external auditory canal and parotid gland. The CT features of congenital second branchial cleft anomaly are that the lesion is located on the ipsilateral submandibular gland (posterior and medial). The CT features of congenital piriform sinus fistula are that the focus is located on the dorsal side of the upper pole of the lateral lobe of the thyroid gland.-
Key words:
- child /
- congenital branchial cleft anomaly /
- tomography, X-ray computed
-

-
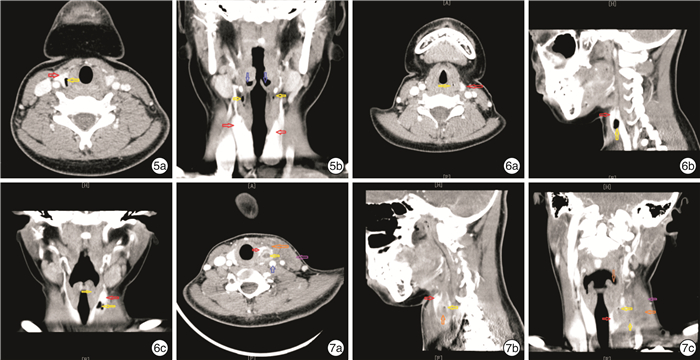
图 1 例1患儿CT检查 1a:横断面可见左侧外耳道(红色箭头)壁圆形低密度影(黄色箭头); 1b:矢状面可见外耳道底、后壁椭圆形低密度影,腮腺(橙色箭头)下缘条索状稍低密度影(黄色箭头); 1c:冠状面可见左侧外耳道下壁及腮腺内椭圆形稍低密度影; 图 2 例2患儿CT检查 2a:横断面可见左侧耳垂至外耳道(红色箭头)下壁内管状气体密度影(黄色箭头); 2b:矢状面可见条索状低密度影,病灶上达外耳道底,穿出腮腺(橙色箭头),下达下颌角颈部皮肤; 2c:冠状面可见左侧外耳道底壁圆形气体密度影,左侧腮腺外下条索状低密度影,病灶上达外耳道底,下达下颌角; 图 3 例3患儿CT检查 3a:横断面可见左侧颈动脉(橙色箭头)三角内、舌骨(蓝色箭头)外、下颌下腺(红色箭头)内侧、颈总动脉和颈内静脉前方圆形低密度影(黄色箭头); 3b:矢状面可见下颌下腺和颈动脉间椭圆形低密度影; 3c:冠状面可见左侧下颌下腺内下及舌骨外下之间椭圆形低密度影; 图 4 例4患儿CT检查 4a:横断面可见右侧下颌下腺(红色箭头)后、颈动脉(橙色箭头)前椭圆形低密度影(黄色箭头); 4b:矢状面可见下颌下腺和颈动脉间管道状低密度影,病灶上达下颌下腺后,下达锁骨平面; 4c:冠状面可见颈右侧下颌下腺和颈动脉间、胸锁乳突肌(紫色箭头)管道状低密度影,病灶上达下颌下腺内侧,下达胸锁乳突肌锁骨头。
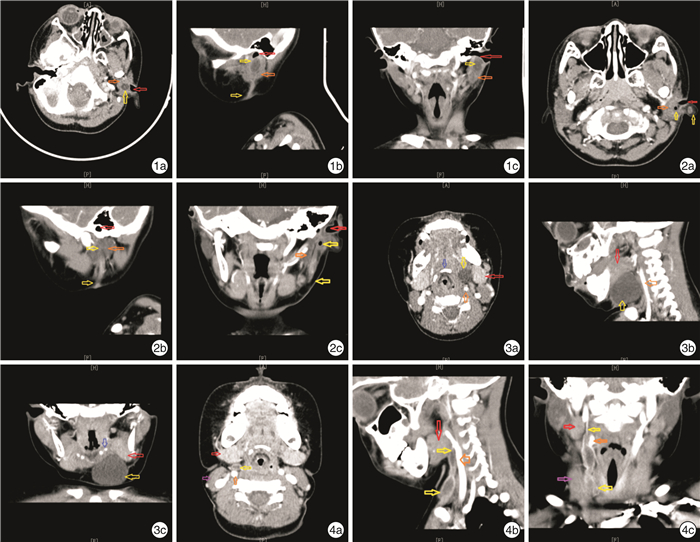
图 5 例5患儿CT检查 5a:横断面可见甲状腺右叶(红色箭头)上极不规则气体低密度影(黄色箭头); 5b:冠状面可见双侧梨状窝(蓝色箭头)下方点状气体低密度影; 图 6 例6患儿静止期CT检查 6a:横断面可见左侧梨状窝圆形低密度气体影(黄色箭头); 6b:矢状面可见甲状腺侧叶(红色箭头)椭圆形低密度气体影; 6c:冠状面可见左侧梨状窝点状低密度影(黄色箭头),甲状腺左叶斑片状低密度气体影,病灶上达梨状窝,穿出甲状腺左叶,下达胸锁乳突肌前缘; 图 7 例6患儿感染期CT检查 7a:横断面可见甲状腺左叶(红色箭头)上极不规则低密度团块影,内部椭圆形低密度影(黄色箭头),炎症(橙色箭头)反应向外膨隆,导致胸锁乳突肌(紫色箭头)和颈动脉鞘(蓝色箭头)结构变化; 7b:矢状面可见甲状腺侧叶内不规则低密度影; 7c:冠状面可见左侧梨状窝(褐色箭头)变浅,周围组织肿胀,甲状腺左叶低密度影,内部散在低密度气体影。
表 1 儿童先天性鳃裂畸形的CT特征性解剖结构
项目 CFBCA CSBCAs CPSF 上端(内瘘口) 开口外耳道(底或后壁)或鼓室 开口扁桃体窝或扁桃体内 开口梨状窝 行走路径 Pochet's三角内,沿外耳道纵轴向外、向下行走,穿过腮腺内成囊状、分叶状、管状,继续沿下颌骨升支向下到达下颌角 颈动脉三角内,茎突舌骨肌和二腹肌后腹外,穿过或越过颈总动脉分叉处,沿胸锁乳突肌深面向下在其中下1/3前缘穿出 环甲关节水平、穿过甲状腺上极(内或被膜边缘)到达胸锁乳突肌中下1/3前缘 特定关系的解剖结构 外耳道壁、腮腺 下颌下腺 甲状腺 下端(外瘘口) 下颌角后缘周围 胸锁乳突肌中下1/3前缘 无(继发感染破溃或医源性切开引流形成) -
[1] 黄选兆, 汪吉宝, 孔维佳, 等. 实用耳鼻咽喉头颈外科学[M]. 2版. 北京: 人民卫生出版社, 2008: 608-616.
[2] Adams A, Mankad K, Offiah C, et al. Branchial cleft anomalies: a pictorial review of embryological development and spectrum of imaging findings[J]. Insights Imaging, 2016, 7(1): 69-76. doi: 10.1007/s13244-015-0454-5
[3] Shekdar KV, Mirsky DM, Kazahaya K, et al. Magnetic resonance imaging of the pediatric neck: an overview[J]. Magn Reson Imaging Clin N Am, 2012, 20(3): 573-603. doi: 10.1016/j.mric.2012.05.008
[4] Black CJ, O'Hara JT, Berry J, et al. Magnetic resonance imaging of branchial cleft abnormalities: illustrated cases and literature review[J]. J Laryngol Otol, 2010, 124(2): 213-215. doi: 10.1017/S0022215109990995
[5] 刘菁华, 杨秀军. 多层螺旋CT在儿童腮裂畸形诊断中的应用[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(2): 146-149. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202002011.htm
[6] Olivas AD, Sherman JM. Firstbran chial clef tanoma-lies[J]. Oper Tech Otolayngol Head Neck Surg, 2017, 28(3): 151-155. doi: 10.1016/j.otot.2017.05.012
[7] Maithani T, Pandey A, Dey D, et al. First branchial cleft anomaly: clinical insight into its relevance in otolaryngology with pediatric considerations[J]. Indian J Otolaryngol Head Neck Surg, 2014, 66(Suppl 1): 271-276.
[8] 陈伟, 陈佳瑞, 陈淑梅, 等. 儿童先天性第一鳃裂畸形的临床分析[J]. 中国眼耳鼻喉科杂志, 2021, 21(6): 425-430, 434. https://www.cnki.com.cn/Article/CJFDTOTAL-YRBH202106006.htm
[9] 张贝, 陈良嗣, 黄舒玲, 等. 先天性第一鳃裂畸形临床特点分析: 附56例报告[J]. 临床耳鼻咽喉头颈外科杂志, 2016, 30(17): 1359-1362. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201617005.htm
[10] 陈良嗣, 张贝, 许咪咪, 等. 基于毗邻解剖的WorkⅠ型先天性第一鳃裂畸形分型及外科策略[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(8): 695-700. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202008005.htm
[11] LaRiviere CA, Waldhausen JH. Congenital cervical cysts, sinuses, and fistulae in pediatric surgery[J]. Surg Clin North Am, 2012, 92(3): 583-597. doi: 10.1016/j.suc.2012.03.015
[12] Adams A, Mankad K, Offiah C, et al. Branchial cleft anomalies: a pictorial review of embryological development and spectrum of imaging findings[J]. Insights Imaging, 2016, 7(1): 69-76. doi: 10.1007/s13244-015-0454-5
[13] Kajosaari L, Mäkitie A, Salminen P, et al. Second branchial cleft fistulae: patient characteristics and surgical outcome[J]. Int J Pediatr Otorhinolaryngol, 2014, 78(9): 1503-1507. doi: 10.1016/j.ijporl.2014.06.020
[14] 曹西迪. 第二鳃裂畸形临床特点及疗效影响因素分析[D]. 郑州大学, 2019.
[15] Pool C, Ehret C, Engle L, et al. Feasibility of same day surgery for pediatric second branchial cleft anomalies[J]. Int J Pediatr Otorhinolaryngol, 2020, 139: 110402. doi: 10.1016/j.ijporl.2020.110402
[16] 中国妇幼保健学会微创分会儿童耳鼻咽喉学组. 儿童先天性梨状窝瘘诊断与治疗临床实践指南[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(12): 1060-1064. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202012002.htm
[17] Wong PY, Moore A, Daya H. Management of third branchial pouch anomalies-an evolution of a minimally invasive technique[J]. Int J Pediatr Otorhinolaryngol, 2014, 78(3): 493-498. doi: 10.1016/j.ijporl.2013.12.027
[18] 陈伟, 倪坤, 顾美珍, 等. 显微支撑喉镜下低温等离子微创治疗儿童先天性梨状窝瘘[J]. 中国耳鼻咽喉颅底外科杂志, 2020, 26(5): 554-558. https://www.cnki.com.cn/Article/CJFDTOTAL-ZEBY202005018.htm
[19] 马静, 明澄, 娄凡, 等. 儿童先天性梨状窝瘘的误诊原因分析及治疗方法探讨[J]. 中华耳鼻咽喉头颈外科杂志, 2018, 53(5): 381-384. doi: 10.3760/cma.j.issn.1673-0860.2018.05.010
[20] 宫喜翔, 陈良嗣, 许咪咪, 等. 先天性梨状窝瘘瘘管走行分段及毗邻解剖临床研究[J]. 中华耳鼻咽喉头颈外科杂志, 2018, 53(8): 604-609. doi: 10.3760/cma.j.issn.1673-0860.2018.08.009
[21] 付营慧, 闵翔, 龙平, 等. 先天性梨状窝瘘的手术治疗和临床解剖学探讨[J]. 临床耳鼻咽喉头颈外科杂志, 2018, 32(13): 984-987. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201813006.htm
[22] 梁璐, 陈良嗣, 周正根, 等. 先天性梨状窝瘘的影像特征[J]. 中华放射学杂志, 2016, 50(3): 196-200. doi: 10.3760/cma.j.issn.1005-1201.2016.03.008
[23] 盛晓丽, 陈良嗣, 许咪咪, 等. 儿童双侧先天性梨状窝瘘1例[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(9): 848-850. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202009018.htm
-

| 引用本文: | 周宜龙, 陈伟, 徐蓉, 等. 儿童先天性鳃裂畸形的CT特征性表现[J]. 临床耳鼻咽喉头颈外科杂志, 2022, 36(6): 441-447. doi: 10.13201/j.issn.2096-7993.2022.06.007 |
| Citation: | ZHOU Yilong, CHEN Wei, XU Rong, et al. Study on CT features of congenital branchial cleft anomaly in children[J]. J Clin Otorhinolaryngol Head Neck Surg, 2022, 36(6): 441-447. doi: 10.13201/j.issn.2096-7993.2022.06.007 |
- Figure 1.
- Figure 5.



 下载:
下载: