Study on changes of nasal resistance based on 3D printing transparent nasal cavity models
-
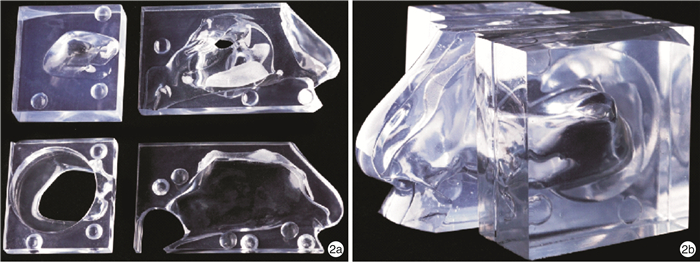
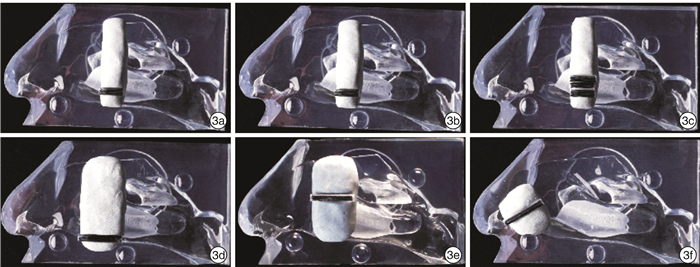
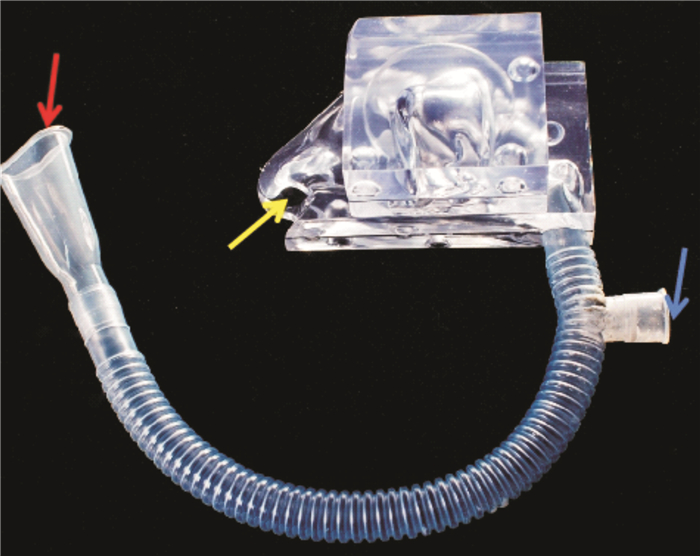
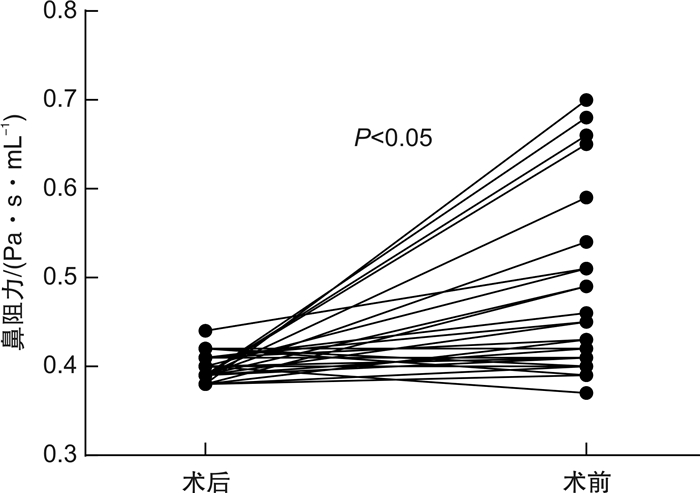
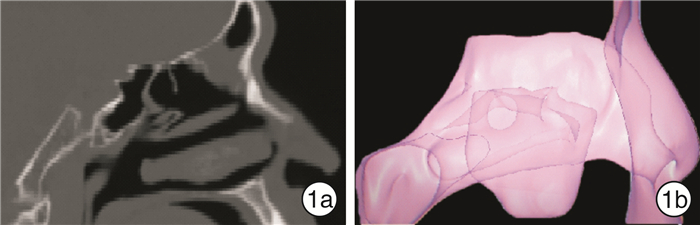
摘要: 目的 探讨鼻腔内最小截面积与鼻阻力互为因果的变化规律。方法 3D打印全透明可拆卸功能性鼻窦内镜手术(FESS)术后鼻腔模型30侧,在不同解剖部位用密封材料彻底堵塞气道,然后用不同截面积的可通气鼻腔引流管再通鼻腔,测量鼻阻力,再进行统计学分析。结果 ① 术后患者实测、3D打印模型鼻阻力分别为(0.38±0.15) Pa·s/mL、(0.39±0.02) Pa·s/mL,两组之间差异无统计学意义(P>0.05),术前患者鼻阻力为(0.56±0.09) Pa·s/mL,术后模型较术前显著下降约31%,差异有统计学意义(P < 0.05);②当截面积为3.14 mm2的可通气鼻腔引流管位于总鼻道上部、鼻阈区时鼻腔均中度阻塞,鼻阻力分别为阻塞前的(1.80±0.30)倍、(2.02±0.36)倍,位于总鼻道下部时鼻腔轻度阻塞,鼻阻力为阻塞前的(1.68±0.28)倍;③当截面积为6.28 mm2的可通气鼻腔引流管位于总鼻道下部、总鼻道上部、鼻阈区时,鼻阻力值分别为阻塞前的(1.44±0.23)倍、(1.50±0.25)倍、(1.60±0.27)倍;④当截面积为9.42 mm2的可通气鼻腔引流管位于以上部位时,鼻腔通气均接近正常,无明显鼻塞,鼻阻力值分别为阻塞前的(1.17±0.18)倍、(1.26±0.21)倍、(1.33±0.24)倍;⑤鼻阻力与通气管截面积、部位相关,相关系数分别为-0.895和0.339,差异均有统计学意义(P < 0.05)。结论 ① 3D打印可快速精准地复制鼻腔解剖结构,可作为定量测量鼻阻力的研究方法;②鼻腔最小截面积为鼻阻力主要决定因素;③部位为鼻阻力的次要决定因素,当阻塞程度相同时,鼻阈区鼻阻力略高于总鼻道。Abstract: Objective To investigate the causal relationship between the minimum cross-sectional area of nasal cavity and nasal resistance.Methods Thirty transparent detachable 3D printing nasal cavity models were made. The airway was completely blocked with sealing material at different anatomical sections. Then ventilatable nasal drainage tubes with different cross-sectional areas were used to pass through the nasal cavity. Nasal resistance was measured. SPSS was used for statistical analysis.Results ① The postoperative nasal resistances of patients and 3D printing nasal cavity models were (0.38±0.15)Pa· s/mL and (0.39±0.02)Pa· s/mL respectively. There was no statistical difference between the two groups.The preoperative nasal resistance of patients was (0.56±0.09)Pa· s/mL, and the postoperative nasal resistance of the models was significantly descreased by 31% compared with preoperative nasal resistance of the patients, with statistically significant difference(P < 0.05). ②When the ventilatable nasal drainage tubes with a cross-sectional area of 3.14 square millimeters was located in the the upper part of common meatus and the nasal valve area, the nasal cavity is moderately blocked, and the nasal resistances were (1.80±0.30) times and (2.02±0.36) times of that before the obstruction respectively. When the ventilatable nasal drainage tube was located in the lower part of common meatus, the nasal resistance was (1.68±0.28) times of that before the obstruction. ③When the ventilatable nasal drainage tubes with a cross-sectional area of 6.28 square millimeters and were located in the lower part of common meatus, the upper part of common meatus and nasal valve area, the nasal resistances were (1.44±0.23) times, (1.50±0.25) times and (1.60±0.27) times of those before obstruction, respectively. ④When the ventilatable nasal drainage tubes with a cross-sectional area of 9.42 square millimeters were located in the above areas, nasal ventilation was nearly normal without obvious nasal obstruction. The nasal resistances were (1.17±0.18) times, (1.26±0.21) times and (1.33±0.24) times of those before obstruction, respectively. ⑤The nasal resistance was statistically significant correlated with the cross-sectional area of the ventilation tubes and the obstruction sites. The correlation coefficients were -0.895 and 0.339, respectively (P < 0.05).Conclusion ① 3D printing can quickly and accurately replicate anatomical structure of the nasal cavity, and can be used as a research method for quantifitative measurement of nasal resistance. ②The minimum cross-sectional area of nasal cavitiy is the main determinant of nasal resistance. ③The obstruction site is the secondary determinant of nasal resistance. When the degree of nasal obstruction is the same, the nasal resistance in the nasal valve area is sightly higher than that in the common meatus.
-
Key words:
- sinusitis /
- nasal resistance /
- 3D printing /
- functional endoscopic sinus surgery
-

-
表 1 鼻腔不同类型再通状态在气道压差为150 Pa时鼻阻力结果
Pa·s/mL,x±s 部位 截面积/mm2 3.14 6.28 9.42 总鼻道下部 0.78±0.02 0.67±0.01 0.55±0.02 总鼻道上部 0.84±0.06 0.70±0.03 0.59±0.02 鼻阈区 0.94±0.04 0.74±0.04 0.63±0.03 表 2 鼻阻力影响因素相关性分析
Pa·s/mL,x±s 变量 鼻阻力 r P 截面积/mm2 -0.895 0.000 3.14 0.86±0.08 6.28 0.71±0.04 9.42 0.59±0.04 部位 0.339 0.000 总鼻道下部 0.67±0.10 总鼻道上部 0.71±0.11 鼻阈区 0.77±0.13 -
[1] Fokkens WJ, Lund VJ, Hopkins C, et al. European Position Paper on Rhinosinusitis and Nasal Polyps 2020[J]. Rhinology, 2020, 58(Suppl S29): 1-464.
[2] 陈平, 张欣, 张红茹, 等. 鼻阻力测定及鼻声反射评估鼻内镜手术通气功能的研究进展[J]. 国际耳鼻咽喉头颈外科杂志, 2019, 43(6): 369-372. doi: 10.3760/cma.j.issn.1673-4106.2019.06.013
[3] Valero A, Navarro AM, Del Cuvillo A, et al. Position paper on nasal obstruction: evaluation and treatment[J]. J Investig Allergol Clin Immunol, 2018, 28(2): 67-90. doi: 10.18176/jiaci.0232
[4] Jessen M, Malm L. The spontaneous course of nasal obstruction in patients with normal nasal airway resistance[J]. Clin Otolaryngol Allied Sci, 1991, 16(3): 302-304. doi: 10.1111/j.1365-2273.1991.tb00936.x
[5] Vogt K, Wernecke KD, Behrbohm H, et al. Four-phase rhinomanometry: a multicentric retrospective analysis of 36, 563 clinical measurements[J]. Eur Arch Otorhinolaryngol, 2016, 273(5): 1185-1198. doi: 10.1007/s00405-015-3723-5
[6] Valtonen O, Ormiskangas J, Kivekäs I, et al. Three-Dimensional Printing of the Nasal Cavities for Clinical Experiments[J]. Sci Rep, 2020, 10(1): 502. doi: 10.1038/s41598-020-57537-2
[7] 许庚, 李源, 谢民强, 等. 功能性内窥镜鼻窦手术后术腔黏膜转归阶段的划分及处理原则[J]. 中华耳鼻咽喉科杂志, 1999, 29(5): 45-48. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHEB199905021.htm
[8] 张健, 王丽华, 沙志荣, 等. 通窍冲洗方对慢性鼻-鼻窦炎Fess术后恢复的疗效观察[J]. 中国中西医结合耳鼻咽喉科杂志, 2018, 26(5): 372-375. https://www.cnki.com.cn/Article/CJFDTOTAL-XYJH201805014.htm
[9] 周书芳, 汪旭. 桉柠蒎肠溶胶囊对慢性鼻窦炎术后鼻黏膜恢复的影响[J]. 检验医学与临床, 2018, 15(13): 1927-1929. doi: 10.3969/j.issn.1672-9455.2018.13.018
[10] 董栋, 吕磊, 陈卓, 等. 3D打印鼻腔鼻窦模型的制作与检验[J]. 中华耳鼻咽喉头颈外科杂志, 2018, 53(8): 615-620. doi: 10.3760/cma.j.issn.1673-0860.2018.08.011
[11] Yu S, Liu Y, Sun X, et al. Influence of nasal structure on the distribution of airflow in nasal cavity[J]. Rhinology, 2008, 46(2): 137-143.
[12] Merkle J, Kohlhas L, Zadoyan G, et al. Rhinomanometric reference intervals for normal total nasal airflow resistance[J]. Rhinology, 2014, 52(4): 292-299. doi: 10.4193/Rhino13.220
[13] 李晓明, 卜国铉. 421名正常成人鼻气道阻力分析[J]. 中华耳鼻咽喉科杂志, 1990, 20(6): 357-359, 384.
[14] Morris S, Jawad MS, Eccles R. Relationships between vital capacity, height and nasal airway resistance in asymptomatic volunteers[J]. Rhinology, 1992, 30(4): 259-264.
[15] 刘彬, 彭正加, 江殿立, 等. 鼻内镜手术治疗鼻阻塞及治疗前后鼻阻力比较[J]. 中国医学工程, 2014, 22(9): 104-105. https://www.cnki.com.cn/Article/CJFDTOTAL-YCGC201409093.htm
[16] Uz U, Günhan K, Ylmaz H, et al. The evaluation of pattern and quality of sleep in patients with chronic rhinosinusitis with nasal polyps[J]. Auris Nasus Larynx, 2017, 44(6): 708-712. doi: 10.1016/j.anl.2017.01.015
[17] 张永杰, 王彤, 臧洪瑞, 等. 鼻内镜术后术腔硅胶扩张引流管应用[J]. 中国耳鼻咽喉头颈外科, 2008, 15(4): 243-244. doi: 10.3969/j.issn.1672-7002.2008.04.026
[18] 戚意冰, 郑开敏. 鼻内镜鼻窦术后硅胶管填塞对鼻腔粘连的影响[J]. 中国基层医药, 2008, 15(3): 508-509. doi: 10.3760/cma.j.issn.1008-6706.2008.03.114
[19] 卫来, 彭凤兰, 王立志, 等. FESS或鼻中隔成形术失败原因及修正性鼻功能重建手术的疗效[J]. 西部医学, 2020, 32(5): 730-735. doi: 10.3969/j.issn.1672-3511.2020.05.025
[20] 李界文, 徐孔昌, 张清惠. 鼻内镜鼻腔扩容术治疗慢性肥厚性鼻炎的临床效果[J]. 中国当代医药, 2019, 26(29): 151-153, 156. doi: 10.3969/j.issn.1674-4721.2019.29.044
[21] 吴俊涛, 饶裕民, 游全贵, 等. 鼻内镜下鼻中隔矫正术治疗鼻中隔偏曲伴变应性鼻炎的疗效[J]. 实用临床医学, 2015, 16(1): 79-80. https://www.cnki.com.cn/Article/CJFDTOTAL-LCSY201501035.htm
[22] 谢晶晶, 吴慧莉, 韦新法. 鼻腔扩容术改善上气道阻力治疗OSAHS的相关研究进展[J]. 世界睡眠医学杂志, 2019, 6(11): 1637-1640. doi: 10.3969/j.issn.2095-7130.2019.11.059
[23] 陈赛明, 周小柳, 李智群, 等. 立体"Z"成形术治疗后天性鼻瓣区膜性狭窄[J]. 中国耳鼻咽喉头颈外科, 2020, 27(1): 34-36. https://www.cnki.com.cn/Article/CJFDTOTAL-EBYT202001010.htm
-




 下载:
下载: