Clinical features and prognostic factors for early-stage external auditory canal carcinoma
-
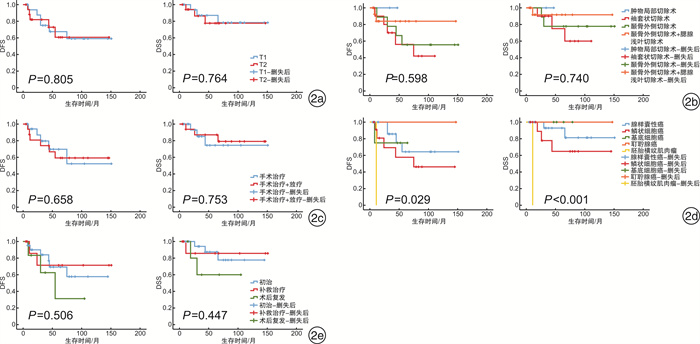
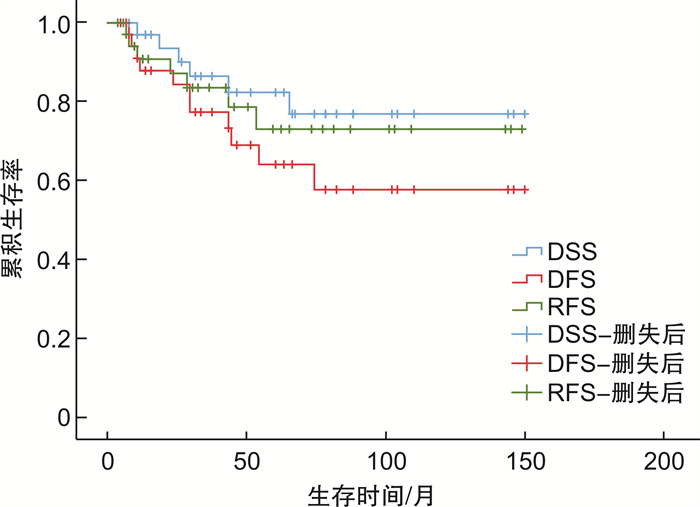
摘要: 目的 探讨早期外耳道癌患者的临床特征及术后复发及预后的相关因素。方法 回顾性分析2008年1月—2020年6月经空军军医大学西京医院耳鼻咽喉科手术治疗的36例早期(T1、T2期)外耳道癌患者资料, 包括临床症状、手术和治疗方式、病理类型、就诊时疾病状态。采用Kaplan-Meier法比较上述因素对患者生存率的影响, 并应用Cox比例风险模型分析影响早期外耳道癌患者预后的独立危险因素。结果 36例早期外耳道癌患者首发症状最常见为耳痛(66.7%), 其次为耳溢液/流脓(41.7%)和听力下降(30.6%)。病理类型以腺样囊性癌(50.0%)和外耳道鳞状细胞癌(33.3%)居多。就诊患者中, 初治者21例(58.3%), 外院手术确诊肿瘤行补救治疗者9例(25.0%), 外耳道癌术后复发再次手术者6例(16.7%)。至随访截至时间, 患者术后5年疾病特异性生存率(DSS)为82.3%, 无病生存率(DFS)为64.0%, 无复发生存率(RFS)为73.0%, 7例(19.4%)患者术后复发。颞骨外侧切除联合腮腺浅叶切除术患者5年生存率(DSS 91.7%, DFS 83.9%)高于颞骨外侧切除术(DSS 77.8%, DFS 55.6%)和袖套状切除术(DSS 75.0%, DFS 56.0%), 但差异无统计学意义(P>0.05)。术后放疗与否、患者就诊时疾病状态对生存率无明显影响。本组患者术后复发与年龄、性别、分期、病理类型、手术方式和术后放疗因素无显著相关性(P>0.05), 但不同病理类型与患者DSS、DFS存在显著性差异(P < 0.05), 且多因素回归分析提示病理类型是影响患者DFS的独立预后因素。结论 早期外耳道癌症状无特异性, 以耳痛、耳溢液多见。病理类型对早期外耳道癌患者的预后有直接影响, 根据早期肿瘤患者病理恶性程度的不同, 制定个体化治疗方案, 可提高患者的生存时间。Abstract: Objective To analyze the clinical features and the prognostic factors of early-stage external auditory canal carcinoma.Methods Data from 36 patients with early-stage external auditory canal carcinoma(T1, T2) treated in Department of Otolaryngology, Xijing Hospital, Air Force Military Medical University from January 2008 to June 2020 were reviewed retrospectively, including clinical manifestations, surgical and treatment methods, pathological types and disease status. The relationship between survival rate and the prognostic factors was compared using Kaplan-Meier method, and the independent risk factors were analyzed by Cox proportional hazards model.Results There were 36 patents with early-stage external auditory canal carcinoma. The common initial symptoms were otalgia(66.7%), otorrhea(41.7%) and hearing loss(30.6%). The most common histopathologic types were adenoid cystic carcinoma(50.0%) and squamous cell carcinoma(33.3%). Among the patients, 21 patients(58.3%) were initially treated, 9 patients(25.0%) were treated with salvage therapy, and 6 patients(16.7%) were re-surgery after recurrence. The 5-year disease-specific survival(DSS), disease-free survival(DFS) and relapse-free survival(RFS) were 82.3%, 64.0% and 73.0% respectively. Seven cases (19.4%) relapsed after surgery. For 5-year survival rate, the lateral temporal bone resection with superficial parotidectomy(DSS 91.7%, DFS 83.9%) is higher than the lateral temporal bone resection only(DSS 77.8%, DFS 55.6%) and sleeve resection(DSS 75.0%, DFS 56.0%), but there was no significant difference(P>0.05). In these patients, the postoperative radiotherapy and disease status had no significant impact on the survival rate. Additionally, there was no obvious correlation between recurrence and age, gender, stage, histopathologic types, operation methods and postoperative radiotherapy(P>0.05). But there were significant differences between histopathologic types and DSS or DFS(P < 0.05). Multivariate regression analysis showed that histopathologic type was an independent prognostic factor for DFS.Conclusion There are no specific clinical manifestations for early-stage external auditory canal carcinoma, such as otalgia and otorrhea. Histopathologic types have a direct impact on the patients'prognosis. Thus, individualized treatment should be applied based on pathologic findings to improve the survival rate.
-
Key words:
- ear neoplasms /
- external auditory canal /
- prognosis
-

-
表 1 36例早期外耳道癌患者的基本资料
基本资料 例(%) 性别 男 17(47.2) 女 19(52.8) 年龄/岁 ≤60 25(69.4) >60 11(30.6) 首发症状 耳痛 24(66.7) 耳溢液/流脓 15(41.7) 听力下降 11(30.6) 外耳道新生物 11(30.6) 耳鸣 9(25.0) 耳出血 8(22.2) 耳闷 5(13.9) 头痛 2(5.6) 病理类型 腺样囊性癌 18(50.0) 鳞状细胞癌 12(33.3) 基底细胞癌 4(11.1) 耵聍腺癌 1(2.8) 胚胎横纹肌肉瘤 1(2.8) 就诊时疾病状态 初治 21(58.3) 补救治疗 9(25.0) 术后复发 6(16.7) 表 2 术后复发的影响因素分析
影响因素 无复发(n=29) 复发(n=7) χ2/F P 年龄/岁 0.442 0.511 平均年龄 48.6±16.8 55.1±19.0 中位年龄 47 48 性别 0.343 0.684 男 13(44.8) 4(57.1) 女 16(55.2) 3(42.9) 分期 0.177 1.000 T1 14(48.3) 4(57.1) T2 15(51.7) 3(42.9) 病理类型 0.887 0.903 腺样囊性癌 15(51.7) 3(42.9) 鳞状细胞癌 9(31.0) 3(42.9) 基底细胞癌 3(10.3) 1(14.3) 耵聍腺癌 1(3.4) 0(0) 胚胎横纹肌肉瘤 1(3.4) 0(0) 手术方式 3.374 0.354 颞骨外侧切除联合腮腺浅叶切除术 13(44.8) 1(14.3) 颞骨外侧切除术 6(20.7) 3(42.9) 袖套状切除术 8(27.6) 3(42.9) 肿物局部切除术 2(6.9) 0(0) 术后放疗 2.043 0.219 是 17(58.6) 2(28.6) 否 12(41.4) 5(71.4) 表 3 预后的多因素分析
病理类型 B Wald Sig. HR 95%CI 腺样囊性癌 参照 5.913 0.206 1.000 — 鳞状细胞癌 0.709 1.092 0.296 2.031 0.538~7.673 基底细胞癌 0.083 0.006 0.941 1.087 0.120~9.849 耵聍腺癌 -12.378 0.000 0.988 0.000 0.000~0.000 胚胎横纹肌肉瘤 3.049 5.599 0.018 21.100 1.688~263.741 -
[1] Moody SA, Hirsch BE, Myers EN. Squamous cell carcinoma of the external auditory canal: an evaluation of a staging system[J]. Am J Otol, 2000, 21(4): 582-588.
[2] Sancho E, Escorial O, Cortés JM, et al. [Laryngeal chondro-radionecrosis][J]. Acta Otorrinolaringol Esp, 2003, 54(2): 123-126. doi: 10.1016/S0001-6519(03)78394-0
[3] Prasad SC, D'Orazio F, Medina M, et al. State of the art in temporal bone malignancies[J]. Curr Opin Otolaryngol Head Neck Surg, 2014, 22(2): 154-165. doi: 10.1097/MOO.0000000000000035
[4] 高燕, 杨慧, 陈飞, 等. 外耳道腺样囊性癌的临床诊治分析[J]. 临床耳鼻咽喉头颈外科杂志, 2018, 32(21): 1660-1664. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201821013.htm
[5] Liu SC, Kang BH, Nieh S, et al. Adenoid cystic carcinoma of the external auditory canal[J]. J Chin Med Assoc, 2012, 75(6): 296-300. doi: 10.1016/j.jcma.2012.04.007
[6] Moffat DA, Grey P, Ballagh RH, et al. Extended Temporal Bone Resection for Squamous Cell Carcinoma[J]. Otolaryngol Head Neck Surg, 1997, 116(6): 617-623. doi: 10.1016/S0194-5998(97)70237-7
[7] Kunst H, Lavieille JP, Marres H. Squamous cell carcinoma of the temporal bone: results and management[J]. Otol Neurotol, 2008, 29(4): 549-552. doi: 10.1097/MAO.0b013e31816c7c71
[8] Ghavami Y, Haidar YM, Maducdoc M, et al. Tympanic Membrane and Ossicular-Sparing Modified Lateral Temporal Bone Resection[J]. Otolaryngol Head Neck Surg, 2017, 157(3): 530-532. doi: 10.1177/0194599817712686
[9] Piras G, Grinblat G, Albertini R, et al. Management of squamous cell carcinoma of the temporal bone: long-term results and factors influencing outcomes[J]. Eur Arch Otorhinolaryngol, 2020.
[10] Zhang T, Li W, Dai C, et al. Evidence-based surgical management of T1 or T2 temporal bone malignancies[J]. Laryngoscope, 2013, 123(1): 244-248. doi: 10.1002/lary.23637
[11] Nam GS, Moon IS, Kim JH, et al. Prognostic Factors Affecting Surgical Outcomes in Squamous Cell Carcinoma of External Auditory Canal[J]. Clin Exp Otorhinolaryngol, 2018, 11(4): 259-266. doi: 10.21053/ceo.2017.01340
[12] Mazzoni A, Danesi G, Zanoletti E. Primary squamous cell carcinoma of the external auditory canal: surgical treatment and long-term outcomes[J]. Acta Otorhinolaryngol Ital, 2014, 34(2): 129-137.
[13] Takenaka Y, Cho H, Nakahara S, et al. Chemoradiation therapy for squamous cell carcinoma of the external auditory canal: A meta-analysis[J]. Head Neck, 2015, 37(7): 1073-1080. doi: 10.1002/hed.23698
[14] Gillespie MB, Francis HW, Chee N, et al. Squamous cell carcinoma of the temporal bone: a radiographic-pathologic correlation[J]. Arch Otolaryngol Head Neck Surg, 2001, 127(7): 803-807.
[15] Choi J, Kim SH, Koh YW, et al. Tumor Stage-Related Role of Radiotherapy in Patients with an External Auditory Canal and Middle Ear Carcinoma[J]. Cancer Res Treat, 2017, 49(1): 178-184. doi: 10.4143/crt.2016.165
[16] Zhang X, Bai S, Li H, et al. CT and MRI findings of radiation-induced external auditory canal carcinoma in patients with nasopharyngeal carcinoma after radiotherapy[J]. Br J Radiol, 2015, 88(1050): 20140791. doi: 10.1259/bjr.20140791
[17] Zanoletti E, Marioni G, Franchella S, et al. Recurrent squamous cell carcinoma of the temporal bone: critical analysis of cases with a poor prognosis[J]. Am J Otolaryngol, 2015, 36(3): 352-355. doi: 10.1016/j.amjoto.2014.12.008
[18] 戴春富, 李轩毅. 外耳道腺样囊性癌临床诊断和治疗的现状和探讨[J]. 临床耳鼻咽喉头颈外科杂志, 2018, 32(20): 1527-1530. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201820002.htm
-




 下载:
下载: