Correlation and difference analysis in parameters between video head impulse test and caloric test in vestibular disease
-
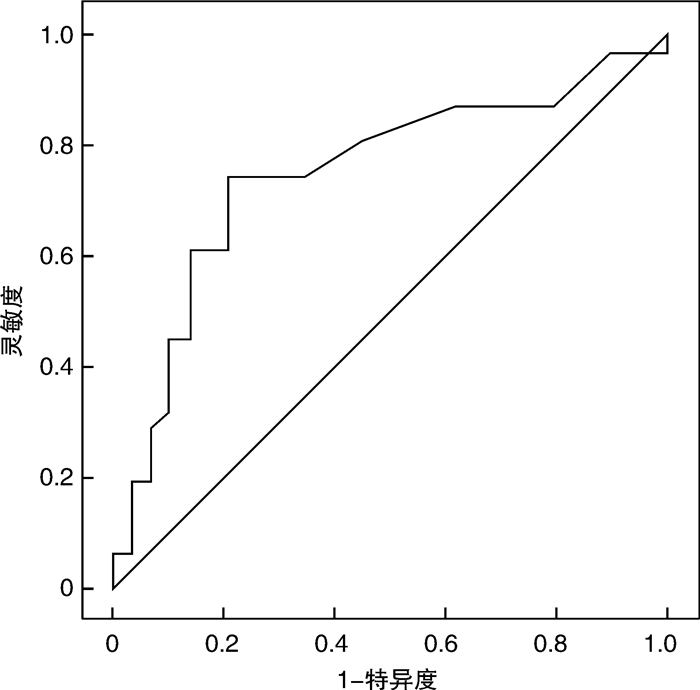
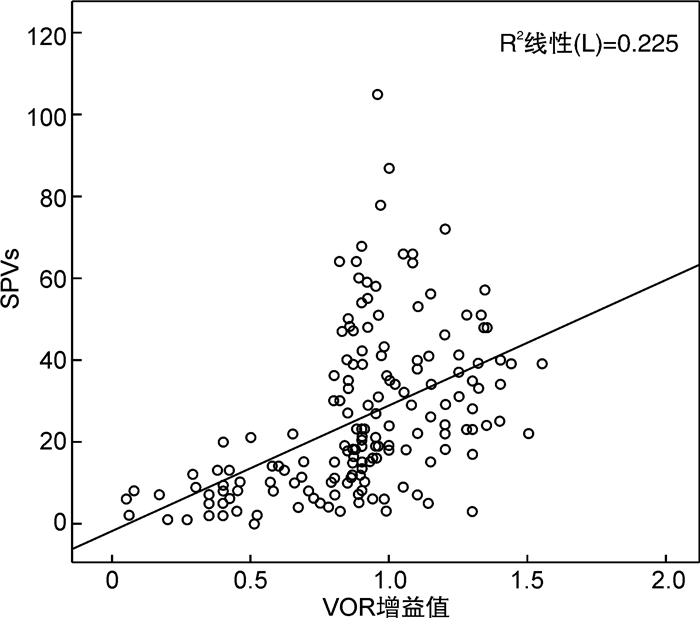
摘要: 目的 探讨视频头脉冲试验(vHIT)与冷热试验各参数在常见周围性眩晕疾病及健康人群中的相互关系及差异性,评估其在周围性眩晕中的临床诊断价值。方法 对85例受试者(17例健康受试者、68例眩晕患者)进行分析。询问病史,并进行耳镜检查、听力学检查后,再行冷热试验和vHIT检查。将vHIT参数中前庭眼反射(VOR)增益、增益不对称比(GA)与冷热试验中同侧慢相速度之和(SPVs)、半规管轻瘫值(UW)分别进行比较。并用受试者操作特征曲线(ROC曲线)计算vHIT的VOR增益值,评估两种检查方法在周围性眩晕中的临床诊断价值。结果 所有耳(n=170)中,同侧SPVs与VOR增益值呈显著正相关(r=0.568,P < 0.0001);健康受试者所有耳(n=34)中,同侧SPVs与VOR增益不相关(r=-0.05,P=0.778);患侧耳(n=76)中,同侧SPVs及VOR增益呈正相关(r=0.571,P < 0.0001);健侧耳(n=94)中,同侧SPVs与VOR增益呈正相关(r=0.286,P=0.005)。单侧前庭病患者患侧耳(n=60)中,VOR增益与UW呈显著负相关(r=-0.513,P < 0.0001);GA与UW呈显著正相关(r=0.713,P < 0.0001)。在波动性眩晕组中(n=34),患侧耳VOR增益和UW呈显著负相关(r=-0.516,P=0.002);GA和UW呈显著正相关(r=0.529,P=0.001);非波动性眩晕组中(n=26),患侧耳VOR增益与UW存在负相关(r=-0.428,P=0.029);GA与UW呈显著正相关(r=0.743,P < 0.0001)。在前庭神经疾病组,患侧耳VOR增益和UW呈负相关(r=-0.462,P=0.030);GA和UW呈显著正相关(r=0.757,P < 0.0001);在前庭末梢疾病组,患侧耳VOR增益与UW呈负相关(r=-0.516,P=0.002);GA与UW呈显著正相关(r=0.529,P=0.001)。孤立性显性扫视的患者组UW均值高于正常组,差异有统计学意义(P=0.006)。按UW损伤程度分级,vHIT的异常检出率差异有统计学意义(χ2=17.76,P < 0.05)。以冷热试验为“金标准”,vHIT的VOR增益界值为0.865,上述两种检查中的参数结果有28.3%的分离。结论 vHIT和冷热试验的参数密切相关,发生孤立性显性扫视的患者UW值高,说明前庭功能损伤可能更严重。vHIT和冷热试验可能是综合评估前庭疾病的互补性检查工具。Abstract: Objective To investigate interrelationships in parameters between caloric test and video head impulse test(vHIT) in the common peripheral vertigo diseases and healthy people, and to conduct correlation and difference analysis between the results in two tests, so as to evaluate the clinical diagnosis value of peripheral vertigo.Methods The caloric test and vHIT were fulfilled in 68 patients with vertigo and 17 healthy volunteers. The diagnosis was done according to history inquiring, otology and audiology examination and vestibular tests. The vestibulo-ocular reflex(VOR) gain and gain asymmetry(GA) of a vHIT as well as unilateral weakness(UW) and the sum of the slow-phase velocities(SPVs) of warm and cold irrigation of the same side were compared. A cutoff value of VOR gain of a vHIT was also calculated using a receiver-operating characteristic curve.Results In all ears(n=170), there was significant correlation in ipsilateral SPVs and VOR gain(r=0.568, P < 0.0001); In all ears(n=34) of 17 healthy volunteers, there was no correlation in ipsilateral SPVs and VOR gain(r=-0.05, P=0.778); In all affected ears(n=76), there was statistically positive correlation in ipsilateral SPVs and VOR gain(r=0.571, P < 0.0001); In all the unaffected ears(n=94), there was positive correlation in ipsilateral SPVs and VOR gain(r=0.286, P=0.005). In 60 patients with unilateral vestibular disease(n=60), there was statistically significant negative correlation between the VOR gain of affected ears and UW(r=-0.513, P < 0.0001); there was statistically significant positive correlation between GA of a vHIT and UW(r=0.713, P < 0.0001). There was a statistically significant negative correlation between the VOR gain of affected ears and UW in the fluctuating vertigo group(r=-0.516, P=0.002) as well as a positive correlation between GA and UW(r=0.529, P=0.001); In the non-fluctuating vertigo group, there was a statistically significant negative correlation between the VOR gain of affected ears and UW(r=-0.428, P=0.029); there was a positive correlation between GA of a vHIT and UW(r=0.743, P < 0.0001). In the vestibular neuropathy group, there was a negative correlation between the VOR gain of affected ears and UW(r=-0.462, P=0.030); there was a statistically significant positive correlation between GA of a vHIT and UW(r=0.757, P < 0.0001). There was a negative correlation between the VOR gain of affected ears and UW in the vestibular peripheral disease group(r=-0.516, P=0.002) as well as a statistically significant positive correlation between GA and UW(r=0.529, P=0.001). The mean value of UW(65.5%) was higher in the overt saccade group than that in the normal VOR group, there was statistically significant difference(P=0.006). According to the UW damage degree grading, there was statistically significant difference in abnormal educe rates(χ2=17.76, P < 0.05). Based on the gold standard of caloric response, a cutoff value of 0.865 was determined; the parameters of the two tests were dissociated in 28.3%.Conclusion There was a statistically significant correlation in parameters between vHIT and caloric test. The patients of overt saccade always accompany with the high UW, which could indicate that the vestibular function severely damaged. vHIT and caloric test can be complementary tools for the comprehensive evaluation of patients' vestibule function, on account of dissociation between the results of vHIT and caloric test and general result of consistent check.
-
Key words:
- vestibular diseases /
- video head impulse test /
- caloric test /
- vestibulo-ocular reflex /
- vertigo
-

-
表 1 扫视类型与UW均值的比较
组别 扫视类型 例数 UW均值/% A组 正常(无病理性扫视) 49 19.55 B组 孤立性隐性扫视 13 31.46 C组 混合性扫视(隐性+显性) 12 44.75 D组 孤立性显性扫视 11 56.45 表 2 对不同组均数行组间事后方差分析
对比组 A-B A-C A-D B-C B-D C-D Std.Error 7.381 9.010 8.612 11.042 10.720 11.900 Sig 0.468 0.087 0.006 0.858 0.199 0.915 表 3 半规管轻瘫指数分级与vHIT异常检出率
损伤程度 UW分级 例数 vHIT异常/例(%) 正常 UW≤25% 28 5(17.9) 轻度 25% < UW≤50% 18 8(44.4) 中重度 UW>50% 14 12(85.7) 表 4 vHIT的诊断率与冷热试验比较
vHIT 冷热试验 UW>25% UW≤25% VOR增益 < 0.8 20 5 VOR增益≥0.8 12 23 -
[1] 杨圆圆, 罗敏, 麻丹丹. 前庭功能减退的病因探讨及预防措施[J]. 医学理论与实践, 2021, 34(1): 160-162. https://www.cnki.com.cn/Article/CJFDTOTAL-YXLL202101082.htm
[2] 杨军, 郑贵亮. 外周前庭疾病的诊断和治疗[J]. 山东大学耳鼻喉眼学报, 2020, 34(5): 1-6. https://www.cnki.com.cn/Article/CJFDTOTAL-SDYU202005001.htm
[3] Halmagyi GM, Curthoys IS. A clinical sign of canal paresis[J]. Arch Neurol, 1988, 45(7): 737-739. doi: 10.1001/archneur.1988.00520310043015
[4] Ulmer E, Chays A. [Curthoys and Halmagyi Head Impulse test: an analytical device][J]. Ann Otolaryngol Chir Cervicofac, 2005, 122(2): 84-90. doi: 10.1016/S0003-438X(05)82329-1
[5] Beynon GJ, Jani P, Baguley DM. A clinical evaluation of head impulse testing[J]. Clin Otolaryngol Allied Sci, 1998, 23(2): 117-122. doi: 10.1046/j.1365-2273.1998.00112.x
[6] 林颖, 高林溪, 韩丽萍, 等. 正常成人水平半规管视频头脉冲检查参数及年龄分布特征[J]. 临床耳鼻咽喉头颈外科杂志, 2016, 30(13): 1063-1065. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201613015.htm
[7] Hullar TE, Della Santina CC, Hirvonen T, et al. Responses of irregularly discharging chinchilla semicircular canal vestibular-nerve afferents during high-frequency head rotations[J]. J Neurophysiol, 2005, 93(5): 2777-2786. doi: 10.1152/jn.01002.2004
[8] Lee IS, Park HJ, Shin JE, et al. Results of air caloric and other vestibular tests in patients with chronic otitis media[J]. Clin Exp Otorhinolaryngol, 2009, 2(3): 145-150. doi: 10.3342/ceo.2009.2.3.145
[9] Mahringer A, Rambold HA. Caloric test and video-head-impulse: astudy of vertigo/dizziness patients in a community hospital[J]. Eur Arch Otorhinolaryngol, 2014, 271: 463-472. doi: 10.1007/s00405-013-2376-5
[10] Zellhuber S, Mahringer A, Rambold HA. Relation of video-headimpulse test andcaloric irrigation: a study on the recovery in unilateralvestibular neuritis[J]. Eur Arch Otorhinolaryngol, 2014, 271: 2375-2383. doi: 10.1007/s00405-013-2723-6
[11] Maire R, van Melle G. Vestibulo-ocular reflex characteristics in patients with unilateral Ménière's disease[J]. Otol Neurotol, 2008, 29(5): 693-698. doi: 10.1097/MAO.0b013e3181776703
[12] 陈建勇, 杨军, 张勤, 等. 良性阵发性眩晕患儿视频头脉冲试验结果分析[J]. 临床耳鼻咽喉头颈外科杂志, 2019, 33(3): 232-236. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201903012.htm
[13] Bartolomeo M, Biboulet R, Pierre G, et al. Value of the video head impulse test in assessing vestibular deficits following vestibular neuritis[J]. Eur Arch Otorhinolaryngol, 2014, 271(4): 681-688. doi: 10.1007/s00405-013-2451-y
[14] Perez N, Rama-Lopez J. Head-impulse and caloric tests in patients with dizziness[J]. Otol Neurotol, 2003, 24(6): 913-917. doi: 10.1097/00129492-200311000-00016
-




 下载:
下载: