Analysis of propensity score matching between inflammatory factor levels and gene polymorphisms and susceptibility to obstructive sleep apnea
-
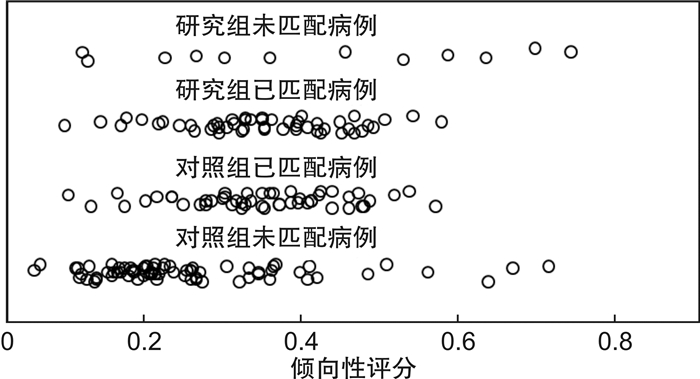
摘要: 目的 :探讨炎症因子水平及其基因多态性与阻塞性睡眠呼吸暂停(OSA)发生之间的相关性。方法 选择2018年10月—2020年12月于新疆维吾尔自治区人民医院确诊的OSA患者79例作为研究组,并选择同期体检的健康成年人104例作为对照组。对两组患者的临床资料进行倾向性评分匹配(PSM),而后对纳入匹配的患者进行血清IL-6、IL-8及TNF-α水平和外周血IL-6、IL-8及TNF-α基因多态性分析比较。结果 匹配前研究组患者年龄、男性占比、BMI、颈围、吸烟史、收缩压和舒张压占比均高于对照组,差异有统计学意义(P < 0.05)。两组患者经PSM后有67例配对成功,在两组间的协变量经匹配后均达到平衡,经PSM各协变量的均衡性得到明显提高(P>0.05)。匹配后研究组患者空腹血糖、C反应蛋白、IL-6、IL-8、TNF-α、AHI及Ts90%显著高于对照组,差异有统计学意义(P < 0.05)。Hardy-Weinberg平衡验证各组基因频率均符合遗传平衡法则(均P>0.05);匹配后两组患者IL-6(rs1800795)及TNF-α(rs1800629)基因亚型分布情况比较,差异有统计学意义;研究组患者IL-6(rs1800795)等位基因C频率及TNF-α(rs1800629)等位基因A频率显著高于对照组,差异有统计学意义(P < 0.05)。结论 炎症因子TNF-α和IL-6水平及其基因多态性与OSA易感性存在显著相关性。
-
关键词:
- 睡眠呼吸暂停,阻塞性 /
- 白细胞介素 /
- 肿瘤坏死因子 /
- 基因多态性 /
- 倾向性评分匹配
Abstract: Objective To explore the correlation between the levels of inflammatory factors and their gene polymorphisms and the susceptibility to obstructive sleep apnea(OSA).Methods Seventy-nine patients who were diagnosed with OSA in People's Hospital of Xinjiang Uygur Autonomous Region from October 2018 to December 2020 were selected as the study group, and 104 healthy adults who received physical examination during the same period were selected as the control group. After collecting the clinical data of the two groups of patients, the two groups of patients were matched by propensity scores. Then, the serum IL-6, IL-8 and TNF-α levels and the peripheral blood IL-6, IL-8 and TNF-α gene polymorphism analysis and comparison were performed on the included matched patients.Results Before matching, the age, proportion of males, BMI, neck circumference, smoking history, SBP and DBP of the study group were higher than those of the control group, and the difference was statistically significant(P < 0.05). After the two groups of patients were matched by propensity scores, a total of 67 patients were successfully matched. The covariates between the two groups were all balanced after matching, and the balance of the PSM covariates was significantly improved(P>0.05). After matching, the fasting blood glucose, C-reactive protein, IL-6, IL-8, TNF-α, AHI and Ts90% of the study group were significantly higher than those of the control group, and the difference was statistically significant(P < 0.05). Hardy-Weinberg balance verifies that the gene frequencies of each group are in accordance with the genetic balance rule(P>0.05); after matching, the distribution of IL-6(rs1800795) and TNF-α(rs1800629) genotypes between the two groups is compared, and the difference is statistically significant scientific significance; the frequency of IL-6(rs1800795) allele C and the frequency of TNF-α(rs1800629) allele A in the study group were significantly higher than those in the control group, and the difference was statistically significant(P < 0.05).Conclusion The levels of inflammatory factors TNF-α and IL-6 and their gene polymorphisms are significantly related to the susceptibility to OSA. -

-
表 1 IL-6、IL-8及TNF-α基因各位点PCR引物序列
项目 序列(5′-3′) IL-6 上游 TGACTTCAGCTTTACTCTTTGT (rs1800795) 下游 CTGATTGGAAACCTTATTAAG IL-8 上游 CACTGGAATTAATGTCTTAG (rs4073) 下游 AAGCTTGTGTGCTCTGCTGTCTCT IL-8 上游 GTCGTATCACAGAGGATTATGC (rs2227306) 下游 CAGTCATAACTGACAACATTGATC TNF-α 上游 AGGCAATAGGTTTTGAGGGCCAT (rs1800629) 下游 GAGCGTCTGCTGGCTGGGTG TNF-α 上游 GGCTCTGAGGAATGGGTTAC (rs1799724) 下游 CCTCTACATGGCCCTGTCTAC 表 2 两组匹配前基线资料比较
组别 例数 年龄/岁 性别 BMI 颈围/cm 吸烟史
/例(%)饮酒史
/例(%)血压/mmHg 男 女 收缩压 舒张压 研究组 79 49.17±10.231) 53 261) 25.47±3.791) 40.07±4.931) 32(40.51)1) 14(17.72) 131.24±14.03 71.21±8.731) 对照组 104 44.52±9.78 53 51 23.07±2.54 37.54±4.02 24(23.08) 11(10.58) 126.34±15.32 77.04±9.51 注:1 mmHg=0.133 kPa。与对照组比较,1)P < 0.05。 表 3 两组匹配后基线资料比较
组别 例数 年龄/岁 性别 BMI 颈围/cm 吸烟史
/例(%)饮酒史
/例(%)血压/mmHg 男 女 收缩压 舒张压 研究组 67 47.51±9.64 39 28 24.13±2.97 39.42±5.01 19(25.36) 7(10.45) 119.53±11.62 78.43±9.21 对照组 67 45.93±10.01 34 33 23.94±2.85 38.64±4.73 14(20.90) 5(7.46) 117.54±10.72 77.65±8.47 表 4 两组实验室检查指标比较
项目 研究组(n=67) 对照组(n=67) TC/(mmol·L-1) 1.82±0.53 1.67±0.42 TG/(mmol·L-1) 4.57±0.73 4.35±0.89 HDL-C/(mmol·L-1) 1.32±0.35 1.41±0.41 LDL-C/(mmol·L-1) 3.22±0.78 2.97±0.82 空腹血糖/(mmol·L-1) 5.56±1.431) 4.97±1.39 C反应蛋白/(mg·L-1) 3.07±0.791) 2.43±0.62 IL-6/(pg·mL-1) 30.21±12.941) 9.37±2.04 IL-8/(pg·mL-1) 31.52±14.241) 11.74±3.97 TNF-α/(pg·mL-1) 29.43±13.641) 11.47±3.86 AHI/(次·h-1) 27.34±4.871) 4.31±1.05 Ts90% 18.47±4.921) 0.71±0.25 与对照组比较,1)P < 0.05。 表 5 匹配后两组IL-6、IL-8及TNF-α基因各位点情况比较
位点 研究组
(n=67)对照组
(n=67)统计值 P值 IL-6(rs1800795) CC 19 11 6.064 0.014 CG 39 36 GG 9 20 C 77 58 5.328 0.020 G 57 76 IL-8(rs4073) AA 17 19 0.013 0.909 AT 32 29 TT 18 19 A 66 67 0.015 0.903 T 68 67 IL-8(rs2227306) CC 20 24 0.986 0.321 CT 26 27 TT 21 16 C 66 75 1.212 0.271 T 68 59 TNF-α(rs1800629) GG 42 60 13.271 < 0.001 GA 20 6 AA 5 1 G 104 128 18.483 < 0.001 A 30 6 TNF-α(rs1799724) CC 54 59 1.421 0.233 CT 11 7 TT 2 1 C 119 125 1.648 0.199 T 15 9 -
[1] Rundo JV. Obstructive sleep apnea basics[J]. Cleve Clin J Med, 2019, 86(9 Suppl 1): 2-9. doi: 10.3949/ccjm.86.s1.02
[2] 贾怡松, 吕思莹, 白尚杰. 阻塞性睡眠呼吸暂停与嗅觉功能的相关性研究[J]. 临床耳鼻咽喉头颈外科杂志, 2021, 35(1): 34-37. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202101008.htm
[3] Veasey SC, Rosen IM. Obstructive Sleep Apnea in Adults[J]. N Engl J Med, 2019, 380(15): 1442-1449. doi: 10.1056/NEJMcp1816152
[4] 孙楷, 聂洪玉, 徐东兰, 等. 鼾症患者中阻塞性睡眠呼吸暂停低通气综合征的筛查及危险因素分析[J]. 中国呼吸与危重监护杂志, 2019, 18(1): 26-30. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGHW201901008.htm
[5] Kheirandish-Gozal L, Gozal D. Obstructive Sleep Apnea and Inflammation: Proof of Concept Based on Two Illustrative Cytokines[J]. Int J Mol Sci, 2019, 20(3): 459. doi: 10.3390/ijms20030459
[6] 中华医学会, 中华医学会杂志社, 中华医学会全科医学分会, 中华医学会呼吸病学分会睡眠呼吸障碍学组, 中华医学会《中华全科医师杂志》编辑委员会, 呼吸系统疾病基层诊疗指南编写专家组. 成人阻塞性睡眠呼吸暂停基层诊疗指南(2018年)[J]. 中华全科医师杂志, 2019, 18(1): 21-29. doi: 10.3760/cma.j.issn.1671-7368.2019.01.007
[7] Salman LA, Shulman R, Cohen JB. Obstructive Sleep Apnea, Hypertension, and Cardiovascular Risk: Epidemiology, Pathophysiology, and Management[J]. Curr Cardiol Rep, 2020, 22(2): 6. doi: 10.1007/s11886-020-1257-y
[8] Lu D, Abulimiti A, Wu T, et al. Pulmonary surfactant-associated proteins and inflammatory factors in obstructive sleep apnea[J]. Sleep Breath, 2018, 22(1): 99-107. doi: 10.1007/s11325-017-1536-z
[9] 李杰茹, 高秀华, 韩聚强, 等. 阻塞性睡眠呼吸暂停患者血浆脂联素、炎性因子与心功能早期损伤相关[J]. 实用医学杂志, 2019, 35(9): 1445-1449. doi: 10.3969/j.issn.1006-5725.2019.09.020
[10] Kheirandish-Gozal L, Gozal D. Obstructive Sleep Apnea and Inflammation: Proof of Concept Based on Two Illustrative Cytokines[J]. Int J Mol Sci, 2019, 20(3): 459. doi: 10.3390/ijms20030459
[11] 许萍, 刘晓静, 徐春燕, 等. 重叠综合征患者血清白介素-6水平与肺功能的关系[J]. 实用医学杂志, 2019, 35(21): 3308-3311. doi: 10.3969/j.issn.1006-5725.2019.21.009
[12] Wu BG, Sulaiman I, Wang J, et al. Severe Obstructive Sleep Apnea Is Associated with Alterations in the Nasal Microbiome and an Increase in Inflammation[J]. Am J Respir Crit Care Med, 2019, 199(1): 99-109. doi: 10.1164/rccm.201801-0119OC
[13] 周斌, 蒋晓真, 陈蕊华, 等. 男性代谢综合征伴睡眠呼吸暂停患者血清代谢指标及脂肪因子变化[J]. 实用医学杂志, 2020, 36(1): 79-83. doi: 10.3969/j.issn.1006-5725.2020.01.015
[14] Caballero-Eraso C, Muñoz-Hernández R, Asensio Cruz MI, et al. Relationship between the endothelial dysfunction and the expression of the β1-subunit of BK channels in a non-hypertensive sleep apnea group[J]. PLoS One, 2019, 14(6): e0217138. doi: 10.1371/journal.pone.0217138
[15] Belaidi E, Morand J, Gras E, et al. Targeting the ROS-HIF-1-endothelin axis as a therapeutic approach for the treatment of obstructive sleep apnea-related cardiovascular complications[J]. Pharmacol Ther, 2016, 168: 1-11. doi: 10.1016/j.pharmthera.2016.07.010
[16] Liu W, Zhang W, Wang T, et al. Obstructive sleep apnea syndrome promotes the progression of aortic dissection via a ROS-HIF-1α-MMPs associated pathway[J]. Int J Biol Sci, 2019, 15(13): 2774-2782. doi: 10.7150/ijbs.34888
[17] Prabhakar NR, Peng YJ, Nanduri J. Hypoxia-inducible factors and obstructive sleep apnea[J]. J Clin Invest, 2020, 130(10): 5042-5051. doi: 10.1172/JCI137560
[18] Yu LM, Zhang WH, Han XX, et al. Hypoxia-Induced ROS Contribute to Myoblast Pyroptosis during Obstructive Sleep Apnea via the NF-κB/HIF-1α Signaling Pathway[J]. Oxid Med Cell Longev, 2019, 2019: 4596368.
[19] Goya TT, Silva RF, Guerra RS, et al. Increased Muscle Sympathetic Nerve Activity and Impaired Executive Performance Capacity in Obstructive Sleep Apnea[J]. Sleep, 2016, 39(1): 25-33. doi: 10.5665/sleep.5310
[20] 谢小晨, 张希龙, 黄茂, 等. 重度阻塞性睡眠呼吸暂停综合征患者脉氧下降率与日间嗜睡的相关性[J]. 中华医学杂志, 2020, 100(28): 2181-2185. doi: 10.3760/cma.j.cn112137-20200309-00670
[21] Bielicki P, MacLeod AK, Douglas NJ, et al. Cytokine gene polymorphisms in obstructive sleep apnoea/hypopnoea syndrome[J]. Sleep Med, 2015, 16(6): 792-795. doi: 10.1016/j.sleep.2015.01.006
[22] Mohan S, Gupta D. Crosstalk of toll-like receptors signaling and Nrf2 pathway for regulation of inflammation[J]. Biomed Pharmacother, 2018, 108: 1866-1878. doi: 10.1016/j.biopha.2018.10.019
[23] Murdaca G, Negrini S, Pellecchio M, et al. Update upon the infection risk in patients receiving TNF alpha inhibitors[J]. Expert Opin Drug Saf, 2019, 18(3): 219-229. doi: 10.1080/14740338.2019.1577817
[24] Wu JC, Zhang X, Wang JH, et al. Gene polymorphisms and circulating levels of the TNF-alpha are associated with ischemic stroke: A meta-analysis based on 19, 873 individuals[J]. Int Immunopharmacol, 2019, 75: 105827. doi: 10.1016/j.intimp.2019.105827
[25] Wang XQ, Hu M, Chen JM, et al. Effects of gene polymorphism and serum levels of IL-2 and IL-6 on endometriosis[J]. Eur Rev Med Pharmacol Sci, 2020, 24(9): 4635-4641.
-




 下载:
下载: