-
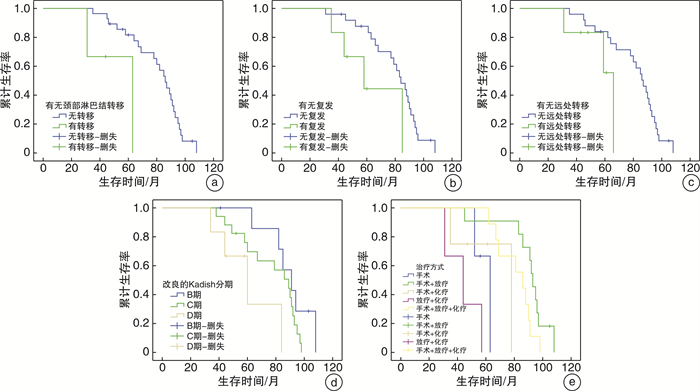
摘要: 目的 探讨嗅神经母细胞瘤的临床特点及影响预后的因素。方法 回顾性分析31例嗅神经母细胞瘤患者的临床资料。结果 31例患者从首次发病到确诊的平均时间为7.84个月, 其中3例(9.68%)首次就诊时已有颈部淋巴结转移。至随访截止时间, 共存活25例, 死亡6例。其中6例复发, 平均复发时间为10.6个月。6例发生远处转移, 其中4例发生颈部淋巴结转移, 发生肝转移和骨转移各1例。改良的Kadish分期、不同治疗方式、有无复发、首诊有无颈部淋巴结转移及有无远处转移均为影响患者预后的因素。结论 嗅神经母细胞瘤的发病率低, 手术联合放疗的综合治疗是最佳的治疗方案。低Kadish分期、手术联合放疗的治疗方式、无复发、首诊无颈部淋巴结转移和无远处转移患者的预后较好。Abstract: Objective To investigate the clinical characteristics and prognostic factors of esthesioneuroblastoma.Methods The clinical data of 31 patients with esthesioneuroblastoma were retrospectively studied.Results The average time from first onset to diagnosis in 31 patients was 7.84 months, among which 3 patients(9.68%) had cervical lymph node metastasis at the first visit. By the end of follow-up, there were 25 coexisting cases and 6 deaths. The mean recurrence time of 6 patients was 10.6 months. There were 6 patients with distant metastasis, including 4 patients with cervical lymph node metastasis, 1 patient with liver metastasis and 1 patient with bone metastasis. Modified Kadish stage, different treatment methods, recurrence, first diagnosis of cervical lymph node metastasis, and distant metastasis were all factors affecting the prognosis of the patients.Conclusion The incidence of esthesioneuroblastoma is low and the comprehensive treatment of surgery combined with radiotherapy is the optimal treatment plan. Patients with low Kadish staging, surgical combined with radiotherapy, no recurrence, no initial cervical lymph node metastasis, and no distant metastasis have a better prognosis.
-
Key words:
- esthesioneuroblastoma /
- surgical procedures, operative /
- radiotherapy /
- prognosis
-

-
[1] Su SY, Bell D, Hanna EY. Esthesioneuroblastoma, neuroendocrine carcinoma, and sinonasal undifferentiated carcinoma: differentiation in diagnosis and treatment[J]. Int Arch Otorhinolaryngol, 2014, 18(Suppl 2): S149-156.
[2] Mahooti S, Wakely PE Jr. Cytopathologic features of olfactory neuroblastoma[J]. Cancer, 2006, 108(2): 86-92. doi: 10.1002/cncr.21718
[3] Platek ME, Merzianu M, Mashtare TL, et al. Improved survival following surgery and radiation therapy for olfactory neuroblastoma: analysis of the SEER database[J]. Radiat Oncol, 2011, 6: 41. doi: 10.1186/1748-717X-6-41
[4] 佘春华, 李文良, 翟琼莉, 等. 成人嗅神经母细胞瘤的临床策略探讨[J]. 中国肿瘤临床, 2015, 42(17): 871-875. doi: 10.3969/j.issn.1000-8179.2015.17.718
[5] Morita A, Ebersold MJ, Olsen KD, et al. Esthesioneuroblastoma: prognosis and management[J]. Neurosurgery, 1993, 32(5): 706-714. doi: 10.1227/00006123-199305000-00002
[6] Bak M, Wein RO. Esthesioneuroblastoma: a contemporary review of diagnosis and management[J]. Hematol Oncol Clin North Am, 2012, 26(6): 1185-1207. doi: 10.1016/j.hoc.2012.08.005
[7] Faragalla H, Weinreb I. Olfactory neuroblastoma: a review and update[J]. Adv Anat Pathol, 2009, 16(5): 322-331. doi: 10.1097/PAP.0b013e3181b544cf
[8] Fiani B, Quadri SA, Cathel A, et al. Esthesioneuroblastoma: A Comprehensive Review of Diagnosis, Management, and Current Treatment Options[J]. World Neurosurg, 2019, 126: 194-211. doi: 10.1016/j.wneu.2019.03.014
[9] Kim HJ, Cho HJ, Kim KS, et al. Results of salvage therapy after failure of initial treatment for advanced olfactory neuroblastoma[J]. J Craniomaxillofac Surg, 2008, 36(1): 47-52. doi: 10.1016/j.jcms.2007.08.004
[10] Abdelmeguid AS. Olfactory Neuroblastoma[J]. Curr Oncol Rep, 2018, 20(1): 7. doi: 10.1007/s11912-018-0661-6
[11] Schwartz JS, Palmer JN, Adappa ND. Contemporary management of esthesioneuroblastoma[J]. Curr Opin Otolaryngol Head Neck Surg, 2016, 24(1): 63-69. doi: 10.1097/MOO.0000000000000220
[12] 高炜, 汪银凤, 王亚林, 等. 嗅神经母细胞瘤内镜手术与传统手术联合放疗疗效分析[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(2): 128-130. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202002007.htm
[13] Xiong L, Zeng XL, Guo CK, et al. Optimal treatment and prognostic factors for esthesioneuroblastoma: retrospective analysis of 187 Chinese patients[J]. BMC Cancer, 2017, 17(1): 254. doi: 10.1186/s12885-017-3247-z
-

| 引用本文: | 贺新娣, 王英. 31例嗅神经母细胞瘤临床分析[J]. 临床耳鼻咽喉头颈外科杂志, 2021, 35(4): 338-340. doi: 10.13201/j.issn.2096-7993.2021.04.012 |
| Citation: | HE Xindi, WANG Ying. Clinical analysis of 31 cases of esthesioneuroblastoma[J]. J Clin Otorhinolaryngol Head Neck Surg, 2021, 35(4): 338-340. doi: 10.13201/j.issn.2096-7993.2021.04.012 |
- Figure 1.



 下载:
下载: