Construction and verification of lymph node metastasis model of cN0 stage thyroid micropapillary carcinoma and discussion of surgical methods
-
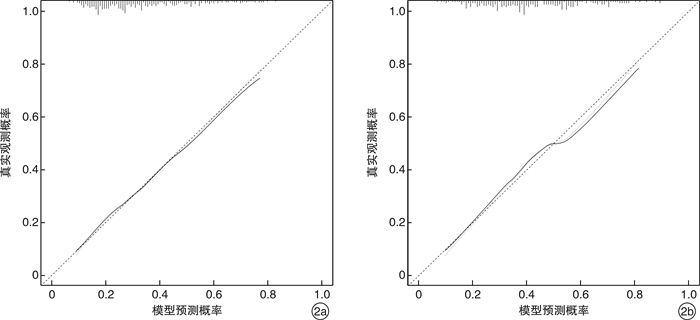
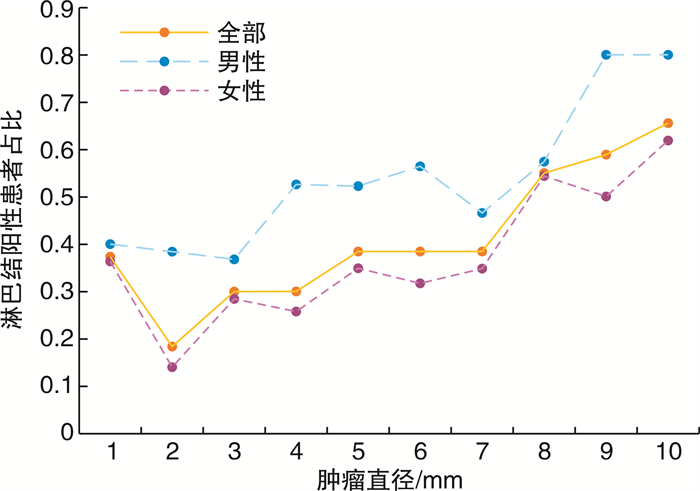
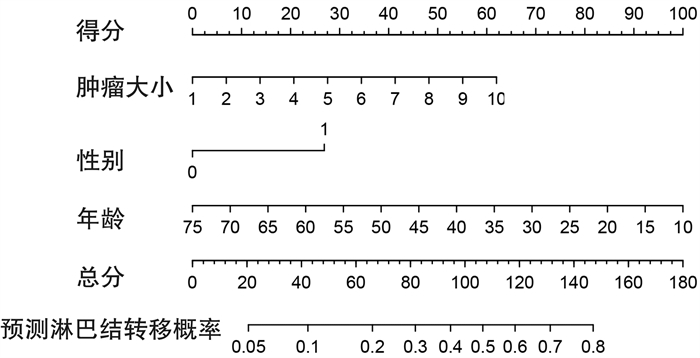
摘要: 目的 构建和验证cN0期甲状腺微小乳头状癌Ⅵ区淋巴结转移模型, 探讨甲状腺腺叶切除联合预防性Ⅵ区淋巴结清扫在cN0期甲状腺微小乳头状癌手术中的意义。方法 收集cN0期甲状腺微小乳头状癌并行Ⅵ区淋巴结清扫的患者670例。所有患者均行患侧甲状腺腺叶±峡部切除+同侧Ⅵ区淋巴结清扫。将性别、年龄、甲状腺乳头状癌的大小、是否多灶、是否被膜侵犯与中央区淋巴结是否转移构建Logistic回归模型, 并用列线图展示最终的回归模型。鉴别力和预测准确性用C指数, 校正曲线和ROC曲线评价。采用内部验证组对拟合模型进行测试。根据肿瘤最大直径分层分析淋巴结转移趋势。随访分析再次手术情况, 评估初次手术治疗效果。结果 Ⅵ区淋巴结转移率为36.7%。多元回归分析纳入3个变量, 肿瘤最大直径(P < 0.001)、男性(P < 0.001)及年轻(P < 0.001)是淋巴结转移的主要独立风险因素。结论 甲状腺腺叶切除联合预防性Ⅵ区淋巴结清扫再次手术率低, 该手术方案治疗cN0期甲状腺微小乳头状癌安全、可靠, 值得推广。Abstract: Objective To construct and verify a model of lymph node metastasis in cN0 stage thyroid micropapillary carcinoma. To explore the significance of thyroid gland lobectomy combined with prophylactic zone Ⅵ lymph node dissection in cN0 stage thyroid micropapillary carcinoma surgery.Methods The clinical data of 670 patients with cN0 stage thyroid micropapillary carcinoma and area Ⅵ lymph node dissection were collected. All patients underwent the affected thyroid gland lobe±isthmus resection+ area Ⅵ lymphadenectomy on the same side. Logistic regression model was constructed by gender, age, size of thyroid papillary carcinoma, whether it was multifocal, whether it was encroaching on the membrane, and whether the lymph nodes in the central area were metastasized, and displayed by nomogram. Discrimination and prediction accuracy were evaluated by C-index, calibration curve and ROC curve. An internal validation group was used to test the fitted model. Analyze the lymph node metastasis trend according to the largest tumor diameter. Follow-up analysis of the reoperation was conducted to evaluate the effect of initial surgery.Results The rate of lymph node metastasis in area Ⅵ was 36.7%. Multiple regression analysis included three variables. The largest tumor diameter(P < 0.001), male(P < 0.001) and young(P < 0.001) were the main independent risk factors for lymph node metastasis.Conclusion The reoperation rate of thyroid gland lobectomy combined with prophylactic zone Ⅵ lymph node dissection was low, and this surgical method might be safe and reliable for the treatment of cN0 stage thyroid micropapillary carcinoma, and it is worthy of promotion.
-
Key words:
- thyroid neoplasms /
- lymph node metastasis /
- surgical procedures /
- prediction /
- nomograms
-

-
表 1 回归模型中的变量及对应参数
参数 系数 标准误差 Wald Z P 常数 0.0665 0.5598 0.12 0.9055 肿瘤最大直径 0.2357 0.0536 4.40 < 0.0001 性别 0.9196 0.2776 3.31 0.0009 年龄 -0.0527 0.0118 -4.47 < 0.0001 -
[1] Haugen BR, Alexander EK, Bibie KC, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer[J]. Thyroid, 2016, 26(1): 1-133. doi: 10.1089/thy.2015.0020
[2] 高明. 甲状腺结节和分化型甲状腺癌诊治指南[J]. 中国肿瘤临床, 2012, 39(17): 1249-1272. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGWK201010018.htm
[3] 中国抗癌协会甲状腺癌专业委员会(CATO). 甲状腺微小乳头状癌诊断与治疗中国专家共识(2016版)[J]. 中国肿瘤临床, 2016, 43(10): 405-411. doi: 10.3969/j.issn.1000-8179.2016.10.001
[4] 赵志宏. 探讨超声诊断甲状腺癌颈部淋巴结转移的临床效果[J]. 影像研究与医学应用, 2020, 4(5): 150-151. https://www.cnki.com.cn/Article/CJFDTOTAL-YXYY202005101.htm
[5] 朱乔丹, 欧笛, 杨菁, 等. 甲状腺乳头状癌颈部淋巴结转移风险评估的研究现状[J]. 中华医学超声杂志(电子版), 2019, 16(11): 880-884. doi: 10.3877/cma.j.issn.1672-6448.2019.11.018
[6] Ito Y, Tomoda C, Uruno T, et al. Clinical significance of metastasis to the central compartment from papillary microcarcinoma of the thyroid[J]. World J Surg, 2006, 30(1): 91-99. doi: 10.1007/s00268-005-0113-y
[7] 项昆, 王建, 张杰, 等. CT、MRI对甲状腺癌转移淋巴结的诊断价值[J]. 现代中西医结合杂志, 2019, 28(6): 663-666. doi: 10.3969/j.issn.1008-8849.2019.06.027
[8] Lu W, Zhong L, Dong D, et al. Radiomic analysis for preoperative prediction of cervical lymph node metastasis in patients with papillary thyroid carcinoma[J]. Eur J Radiol, 2019, 118: 231-238. doi: 10.1016/j.ejrad.2019.07.018
[9] Ito Y, Tomoda C, Uruno T, et al. Papillary microcarcinoma of the thyroid: how should it be treated?[J]. World J Surg, 2004, 28(11): 1115-1121. doi: 10.1007/s00268-004-7644-5
[10] Wang Y, Guan Q, Xiang J. Nomogram for predicting level Ⅴ lymph node metastases in papillary thyroid carcinoma with clinically lateral lymph node metastases: A large retrospective cohort study of 1037 patients from FDUSCC[J]. J Cancer, 2019, 10(3): 772-778. doi: 10.7150/jca.28527
[11] Sywak M, Cornford L, Roach P, et al. Routine ipsilateral level Ⅵ lymphadenectomy reduces postoperative thyroglobulin levels in papillary thyroid cancer[J]. Surgery, 2006, 140(6): 1000-1007. doi: 10.1016/j.surg.2006.08.001
[12] 刘春萍, 李治, 黄韬. 抗甲状腺球蛋白抗体对分化型甲状腺癌患者术后血甲状腺球蛋白监测的影响[J]. 实用癌症杂志, 2006, 21(4): 369-370. doi: 10.3969/j.issn.1001-5930.2006.04.011
[13] 邱帅, 司延芳, 房学东, 等. 乳头状甲状腺癌颈部淋巴结转移相关因素的logistic分析[J]. 中国实验诊断学, 2017, 21(11): 1961-1962. doi: 10.3969/j.issn.1007-4287.2017.11.028
[14] 郑克思, 曾勇, 陈聪, 等. 基于监测、流行病学和最终结果数据库甲状腺乳头状微癌颈部淋巴结转移的危险因素[J]. 中国医学科学院学报, 2018, 40(6): 736-743. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYKX201806003.htm
[15] 石臣磊, 石铁锋, 吴佳奇, 等. 桥本甲状腺炎对乳头状甲状腺癌颈淋巴结转移的影响[J]. 中国普通外科杂志, 2013, 22(5): 580-584. https://www.cnki.com.cn/Article/CJFDTOTAL-ZPWZ201305013.htm
[16] Chen L, Zhang J, Meng L, et al. A new ultrasound nomogram for differentiating benign and malignant thyroid nodules[J]. Clin Endocrinol(Oxf), 2019, 90(2): 351-359. doi: 10.1111/cen.13898
[17] Ding Y, Mao Z, Ruan J, et al. Nomogram-Based New Recurrence Predicting System in Early-Stage Papillary Thyroid Cancer[J]. Int J Endocrinol, 2019, 2019: 1029092.
[18] Guo BL, Ouyang FS, Ouyang LZ, et al. Development and validation of an ultrasound-based nomogram to improve the diagnostic accuracy for malignant thyroid nodules[J]. Eur Radiol, 2019, 29(3): 1518-1526. doi: 10.1007/s00330-018-5715-5
[19] Hei H, Song Y, Qin J. Individual prediction of lateral neck metastasis risk in patients with unifocal papillary thyroid carcinoma[J]. Eur J Surg Oncol, 2019, 45(6): 1039-1045. doi: 10.1016/j.ejso.2019.02.016
[20] Liang L, Xie J, Li S, et al. Nomogram for the diagnosis of suspected papillary thyroid carcinomas based on sonographic patterns: a retrospective study[J]. Gland Surg, 2019, 8(4): 362-369. doi: 10.21037/gs.2019.07.09
[21] Wen Q, Yu Y, Yang J, et al. Development and Validation of a Nomogram for Predicting Survival in Patients with Thyroid Cancer[J]. Med Sci Monit, 2019, 25: 5561-5571. doi: 10.12659/MSM.915620
-




 下载:
下载: