Comparative analysis of clinical features of primary and secondary laryngeal tuberculosis
-
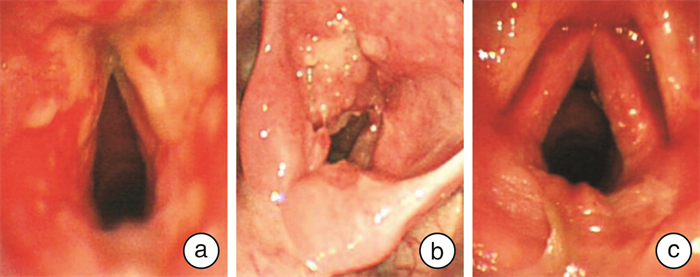
摘要: 目的 探讨原发性和继发性喉结核的临床模式、诊断和治疗。方法 回顾性分析103例确诊为喉结核的患者, 从病例记录中获得人口学特征、生活方式、临床特征、诊断和治疗。结果 103例患者中, 64例被诊断为原发性喉结核, 39例被诊断为继发性喉结核。最常见的症状是声音嘶哑和吞咽困难。声带是最常见的侵犯部位。大多数原发性喉结核病患者表现为单发、增生病变。继发性喉结核表现为溃疡、水肿、多部位病变。所有喉结核患者均给予系统的抗结核治疗。如果患者出现喉梗阻, 则考虑手术治疗。结论 原发性、继发性喉结核的临床表现、体征存在差异。喉结核容易误诊为喉炎、喉肿瘤, 应进行病理学检查, 以明确诊断。Abstract: Objective The aim of this study was to analyze and compare the clinical pattern, diagnosis and treatment in primary and secondary laryngeal and pharyngeal TB.Methods A retrospective analysis was carried out on 103 patients diagnosed laryngeal tuberculosis in our department. Characteristics of demography, life-style, clinical features, diagnosis and treatment were obtained from medical case records. Clinical analysis of 103 patients with pathologically confirmed laryngeal TB was carried out retrospectively in the second affiliated hospital of Nanchang university in Jiangxi province.Results Among 103 patients, 64 cases were diagnosed as primary laryngeal TB and 39 cases were diagnosed as secondary laryngeal TB. The most common complaints were hoarseness and odynophagia. The true and the false vocal cords were most commonly involved. Most patients with primary tuberculosis of the larynx present a single, hyperplastic lesion.Secondary laryngeal TB of larynx was characterized by ulcers, edema effusive, multiple sites lesions. The anti-TB treatment was given systemically to all patients. The surgery should be considered if the patient has a laryngeal obstruction.Conclusion The clinical manifestations and signs of primary and secondary tuberculosis of the larynx are different. Laryngeal tuberculosis is easy to be misdiagnosed as laryngitis and laryngeal tumors. Pathological examination should be performed to confirm the diagnosis.
-
Key words:
- tuberculosis, larynx /
- clinical features /
- misdiagnosis
-

-
表 1 原发性和继发性喉结核的人口学及烟酒不良嗜好的比较
例(%) 项目 例数(%) 原发性喉结核 继发性喉结核 P 性别 0 男 75(72.81) 53(51.46) 22(21.36) 女 28(27.18) 11(10.68) 17(16.50) 年龄/岁 0~20 4(3.88) 0(0) 4(3.88) >20~30 4(3.88) 2(1.94) 2(1.94) >30~40 12(11.65) 7(6.80) 5(4.85) >40~50 31(30.10) 20(19.42) 11(10.68) >50~60 25(24.27) 17(16.50) 8(7.78) >60~70 20(19.42) 12(11.65) 8(7.78) >70 7(6.80) 4(3.88) 3(2.91) 出生地 0 城市 32(31.07) 24(23.30) 8(7.77) 农村 71(68.93) 42(40.78) 31(30.10) 吸烟 0.06 否 38(36.89) 20(19.42) 18(17.48) 是 65(63.11) 44(42.72) 21(20.39) 饮酒 0.05 否 66(64.08) 32(31.08) 34(33.01) 是 47(45.63) 32(31.08) 15(14.56) 表 2 原发性和继发性喉结核内镜特征比较
喉镜特征 原发性喉结核 继发性喉结核 χ2 P 浸润和水肿型 12(18.75) 19(48.72) 12.776 0.002 增生型 37(57.81) 10(25.64) 喉炎型 15(23.44) 10(25.64) 多部位 18(28.13) 32(82.05) 28.212 0.00 单部位 46(71.87) 7(17.95) -
[1] Shin JE, Nam SY, Yoo SJ, et al. Changing trends in clinical manifestations of laryngeal tuberculosis[J]. Laryngoscope, 2000, 110(11): 1950-1953. doi: 10.1097/00005537-200011000-00034
[2] Wang CC, Lin CC, Wang CP, et al. Laryngeal tuberculosis: a review of 26 cases[J]. Otolaryngol Head Neck Surg, 2007, 137(4): 582-588. doi: 10.1016/j.otohns.2007.04.002
[3] Rizzo PB, Da Mosto MC, Clari M, et al. Laryngeal tuberculosis: an often forgotten diagnosis[J]. Int J Infect Dis, 2003, 7(2): 129-131. doi: 10.1016/S1201-9712(03)90008-7
[4] Harding E. WHO global progress report on tuberculosis elimination[J]. Lancet Respir Med, 2020, 8(1): 19-19. doi: 10.1016/S2213-2600(19)30418-7
[5] Zheng Y L, Zhang L P, Zhang X L, et al. Forecast Model Analysis for the Morbidity of Tuberculosis in Xinjiang, China[J]. PLoS One, 2015, 10(3): e0116832. doi: 10.1371/journal.pone.0116832
[6] Peto HM, Pratt RH, Harrington TA, et al. Epidemiology of extrapulmonary tuberculosis in the United States, 1993-2006[J]. Clin Infect Dis, 2009, 49(9): 1350-1357. doi: 10.1086/605559
[7] te Beek LA, van der Werf MJ, Richter C, et al. Extrapulmonary tuberculosis by nationality, The Netherlands, 1993-2001[J]. Emerg Infect Dis, 2006, 12(9): 1375-1382.
[8] Forssbohm M, Zwahlen M, Loddenkemper R, et al. Demographic characteristics of patients with extrapulmonary tuberculosis in Germany[J]. Eur Respir J, 2008, 31(1): 99-105. doi: 10.1183/09031936.00020607
[9] Zhang X, Andersen AB, Lillebaek T, et al. Effect of sex, age, and race on the clinical presentation of tuberculosis: a 15-year population-based study[J]. Am J Trop Med Hyg, 2011, 85(2): 285-290. doi: 10.4269/ajtmh.2011.10-0630
[10] Wang X, Yang Z, Fu Y, et al. Insight to the Epidemiology and Risk Factors of Extrapulmonary Tuberculosis in Tianjin, China during 2006-2011[J]. PLoS One, 2014, 9(12): e112213. doi: 10.1371/journal.pone.0112213
[11] Kulkarni NS, Gopal GS, Ghaisas SG, et al. Epidemiological considerations and clinical features of ENT tuberculosis[J]. J Laryngol Otol, 2001, 115(7): 555-558.
[12] Flynn JL, Chan J, Lin PL. Macrophages and control of granulomatous inflammation in tuberculosis[J]. Mucosal Immunol, 2011, 4(3): 271-278. doi: 10.1038/mi.2011.14
[13] El Ayoubi F, Chariba I, El Ayoubi A, et al. Primary tuberculosis of the larynx[J]. Eur Ann Otorhinolaryngol Head Neck Dis, 2014, 131(6): 361-364. doi: 10.1016/j.anorl.2013.10.005
[14] Benwill JL, Sarria JC. Laryngeal tuberculosis in the United States of America: a forgotten disease[J]. Scand J Infect Dis, 2014, 46(4): 241-249. doi: 10.3109/00365548.2013.877157
[15] Cranford J, Kadakia S, Berzofsky C. Palatopharyngoplasty for treatment of nasopharyngeal stenosis secondary to extra-laryngeal tuberculosis[J]. Am J Otolaryngol, 2016, 37(6): 559-562. doi: 10.1016/j.amjoto.2016.06.002
[16] Lee JY. Diagnosis and treatment of extrapulmonary tuberculosis[J]. Tuberc Respir Dis(Seoul), 2015, 78(2): 47-55. doi: 10.4046/trd.2015.78.2.47
[17] Stickney DR, Noveljic Z, Garsd A, et al. Safety and activity of the immune modulator HE2000 on the incidence of tuberculosis and other opportunistic infections in AIDS patients[J]. Antimicrob Agents Chemother, 2007, 51(7): 2639-2641. doi: 10.1128/AAC.01446-06
-




 下载:
下载: