-
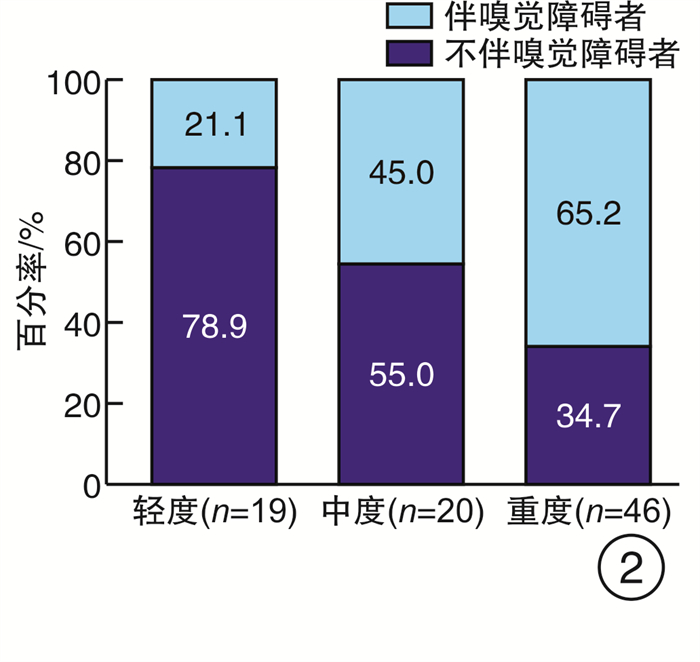
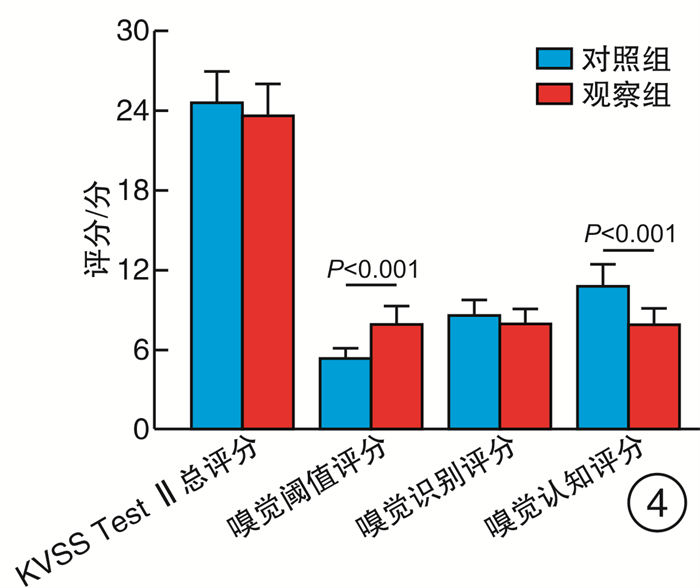
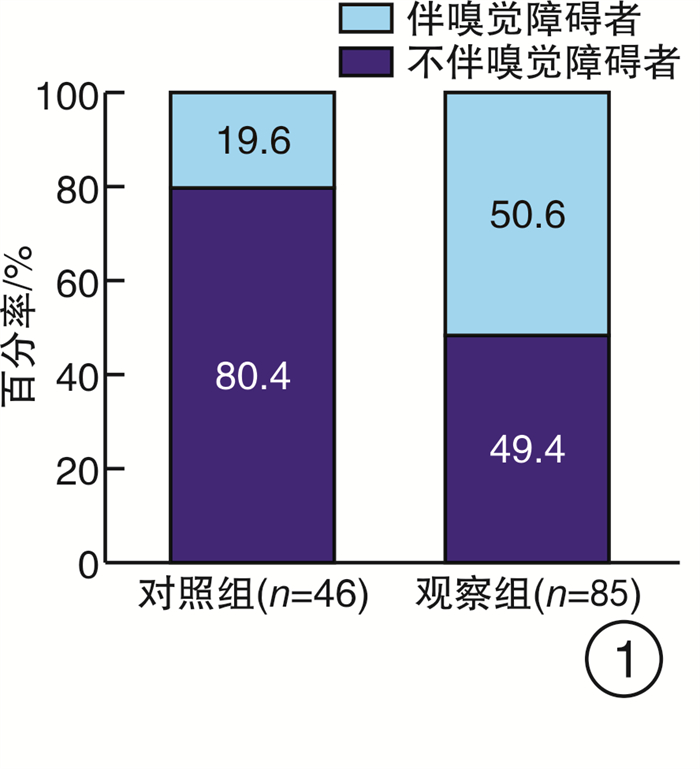
摘要: 目的 探讨未经任何治疗的阻塞性睡眠呼吸暂停(OSA)患者的嗅觉功能, 为临床嗅觉的研究提供参考依据。方法 131例参与者分别行PSG监测, 根据结果分成OSA组(观察组)和健康志愿者(对照组), 对两组分别行韩国版的嗅棒测试Ⅱ检查, 并采用SPSS 26.0软件对数据进行分析。结果 观察组与对照组嗅觉障碍的发生率存在显著差异(χ2=12.000, P=0.001);重度OSA患者发生嗅觉障碍的比率显著高于轻度患者(P < 0.05), 且随着OSA病情严重程度的增高嗅觉障碍患者所占比率呈增加的趋势(χ2=10.672, P=0.001);观察组与对照组发生嗅觉障碍严重程度(即嗅觉减退和嗅觉缺失)的构成之间差异无统计学意义(P=1.000), 均以嗅觉减退为主; 两组间KVSS Test Ⅱ总分差异无统计学意义(t=1.166, P=0.249), 嗅觉识别评分差异亦无统计学意义(t=1.598, P=0.116), 但嗅觉阈值评分和嗅觉认知评分差异有统计学意义(t=5.346, t=6.405, 均P < 0.001)。结论 OSA对嗅觉有负面影响, 并且病情严重程度与嗅觉障碍的发病率呈正相关, OSA发生的嗅觉障碍以嗅觉减退为主, 且主要表现为嗅觉认知分数的下降。
-
关键词:
- 睡眠呼吸暂停, 阻塞性 /
- 嗅觉功能
Abstract: Objective To investigate the olfactory function of patients with obstructive sleep apnea(OSA) without any treatment, and to providereference for clinical olfactory research.Methods One hundred and thirty-one participants underwent polysomnography(PSG) overnight, and were divided into OSA group (observation group) and non-OSA group (control group) according to the results. The two groups were examined by the Korean version of the olfactory stick test Ⅱ(Korean Bersion) of Sniffin Sticks Test (KVSS Test Ⅱ). SPSS 26.0 statistical software were used to analyze the data.Results There was a significant difference in the incidence of olfactory disorders between the observation group and the control group(χ2=12.000, P=0.001). The rate of olfactory disorders in patients with severe OSA was significantly higher than that in patients with mild OSA(P < 0.05), and the proportion of patients with olfactory disorders increased with the increase of OSA severity(χ2=10.672, P=0.001). There was no statistically significant difference between the observation group and the control group in the severity of olfactory disorders(hyposmia and anosmia)(P=1.000). KVSS between two groups of Test Ⅱ total score has no statistical difference(t=1.166, P=0.249), the sense of smell recognition scores also has no statistical difference(t=1.598, P=0.116), but the olfactory threshold score and olfactory cognition scores were statistically significant(t=5.346, t=6.405, P < 0.001).Conclusion OSA has a negative effect on the sense of smell, and the severity of OSA is positively correlated with the incidence of olfactory disorder. OSA olfactory disorder is mainly anosmia, and the main manifestation is the decrease of olfactory cognitive scores.-
Key words:
- sleep apnea, obstructive /
- olfactory function
-

-
表 1 观察组与对照组基本信息
组别 例数 性别 年龄/岁 吸烟史/年 受教育程度/年 男 女 观察组 85 70 15 42.0(34.0,50.0) 10.0(0.0,21.0) 12.0(8.0,15.0) 对照组 46 37 9 42.0(35.3,50.8) 12.5(5.0,21.0) 12.0(9.0,15.0) Z/χ2 0.073 -0.256 -0.903 -0.700 P 0.786 0.798 0.366 0.484 表 2 观察组伴嗅觉障碍与不伴嗅觉障碍者基本信息
指标 伴嗅觉障碍者(n=43) 不伴嗅觉障碍者(n=42) Z/t值 P 病程/年 5.0(4.0,9.0) 6.0(4.0,8.0) 0.287 0.775 BMI 30.45±5.11 29.39±3.71 1.097 0.276 -
[1] Günbey E, Güzel A, Karlı R, Ünal R. The relationships between the clinical and polysomnographic findings and the olfactory function in patients with obstructive sleep apnea syndrome[J]. Sleep Breath, 2015, 19(4): 1301-1307. doi: 10.1007/s11325-015-1165-3
[2] Lai CC, Lin PW, Lin HC, et al. Effects of Upper Airway Surgery on Daytime Sleepiness in Nonobese Patients with Obstructive Sleep Apnea/Hypopnea Syndrome[J]. Ann Otol Rhinol Laryngol, 2018, 127(12): 912-918. doi: 10.1177/0003489418800089
[3] Doǧan A, Bayar Muluk N, Şahin H. Olfactory Bulb Volume and Olfactory Sulcus Depth in Patients With OSA: An MRI Evaluation[J]. Ear Nose Throat J, 2020, 99(7): 442-447. doi: 10.1177/0145561319881571
[4] Salihoǧlu M, Kendirli MT, Altundaǧ A, et al. The effect of obstructive sleep apnea on olfactory functions[J]. Laryngoscope, 2014, 124(9): 2190-4. doi: 10.1002/lary.24565
[5] 中华耳鼻咽喉头颈外科杂志编辑委员会, 中华医学会耳鼻咽喉头颈外科学分会咽喉学组. 阻塞性睡眠呼吸暂停低通气综合征诊断和外科治疗指南[J]. 中华耳鼻咽喉头颈外科杂志, 2009, 44(2): 95-96. doi: 10.3760/cma.j.issn.1673-0860.2009.02.003
[6] Huang Y, Liu Y, Zhao D, et al. Small-world properties of the whole-brain functional networks in patients with obstructive sleep apnea-hypopnea syndrome[J]. Sleep Med, 2019, 62: 53-58. doi: 10.1016/j.sleep.2018.08.037
[7] Fu D, Pinto JM, Wang L, et al. The effect of nasal structure on olfactory function in patients with OSA[J]. Eur Arch Otorhinolaryngol, 2015, 272(2): 357-362. doi: 10.1007/s00405-014-3096-1
[8] Shin DH, Ahn SH, Yang Y, et al. The Effect of Sleep Disordered Breathing on Olfactory Functions: Analysis by Apnea-Hypopnea Index[J]. Clin Exp Otorhinolaryngol, 2017, 10(1): 71-76. doi: 10.21053/ceo.2015.01438
[9] Kaya KS, Akpınar M, Turk B, et al. Olfactory Function in Patients With Obstructive Sleep Apnea Using Positive Airway Pressure[J]. Ear Nose Throat J, 2020, 99(4): 239-244. doi: 10.1177/0145561319878949
[10] Passali D, Corallo G, Petti A, et al. A comparative study on oxidative stress role in nasal breathing impairment and obstructive sleep apnoea syndrome[J]. Acta Otorhinolaryngol Ital, 2016, 36(6): 490-495. doi: 10.14639/0392-100X-1361
[11] Carpagnano GE, Spanevello A, Sabato R, et al. Systemic and airway inflammation in sleep apnea and obesity: the role of ICAM-1 and IL-8[J]. Transl Res, 2010, 155(1): 35-43. doi: 10.1016/j.trsl.2009.09.004
[12] Magliulo G, De Vincentiis M, Iannella G, et al. Olfactory evaluation in obstructive sleep apnoea patients[J]. Acta Otorhinolaryngol Ital, 2018, 38(4): 338-345. doi: 10.14639/0392-100X-1981
[13] Huppertz T, Freiherr J, Olzowy B, et al. Reduction of olfactory sensitivity during normobaric hypoxia[J]. Auris Nasus Larynx, 2018, 45(4): 747-752. doi: 10.1016/j.anl.2017.11.001
[14] Ruffini R, Di Giulio C, Verratti V, et al. Adaptation of olfactory threshold at high altitude[J]. Adv Exp Med Biol, 2015, 837: 19-22.
[15] Walliczek-Dworschak U, Cassel W, Mittendorf L, et al. Continuous positive air pressure improves orthonasal olfactory function of patients with obstructive sleep apnea[J]. Sleep Med, 2017, 34: 24-29. doi: 10.1016/j.sleep.2017.02.018
[16] Magliulo G, De Vincentiis M, Iannella G, et al. Olfactory evaluation in obstructive sleep apnoea patients[J]. Acta Otorhinolaryngol Ital, 2018, 38(4): 338-345. doi: 10.14639/0392-100X-1981
-

| 引用本文: | 贾怡松, 吕思莹, 白尚杰. 阻塞性睡眠呼吸暂停与嗅觉功能的相关性研究[J]. 临床耳鼻咽喉头颈外科杂志, 2021, 35(1): 34-37. doi: 10.13201/j.issn.2096-7993.2021.01.008 |
| Citation: | JIA Yisong, LV Siying, BAI Shangjie. The correlation between obstructive sleep apnea and olfaction function[J]. J Clin Otorhinolaryngol Head Neck Surg, 2021, 35(1): 34-37. doi: 10.13201/j.issn.2096-7993.2021.01.008 |
- Figure 1.
- Figure 2.
- Figure 3.
- Figure 4.



 下载:
下载: