Short-term postoperative outcome of laser-assisted stapedotomy in patients with otosclerosis
-
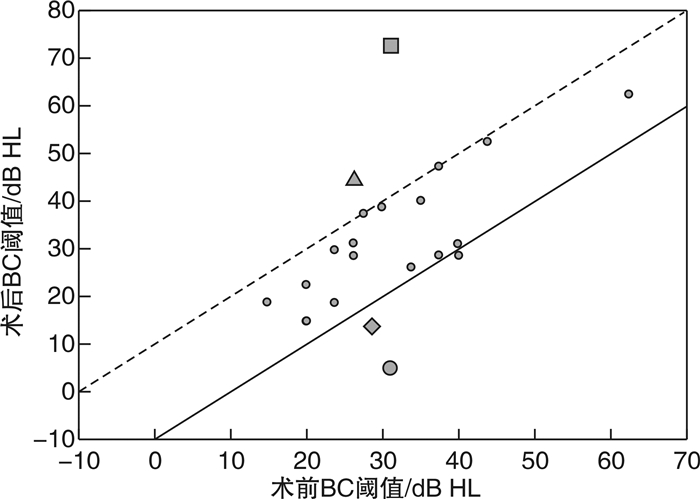
摘要: 目的 评估耳硬化症患者行激光镫骨底板开窗术后的短期疗效。方法 回顾性分析21例(21耳)行激光镫骨底板开窗术的耳硬化症患者的临床资料。比较术前和术后3个月纯音测听0.5、1、2、4 kHz频率的气导(AC)、骨导(BC)阈值和气骨导差(ABG)平均值,并统计手术并发症的发生情况。结果 21耳术前和术后AC阈值分别为(58.2±12.7) dB HL和(43.0±23.1) dB HL,术后AC阈值降低15.2 dB HL(P < 0.01);0.5、1、2、4 kHz各频率术后AC阈值较术前均显著降低。术前术后BC阈值分别为(31.4±10.3) dB HL和(33.3±16.6) dB HL,差异无统计学意义;各频率的手术前后BC阈值差异亦无统计学意义。3耳(14.3%)术后BC阈值减低>10 dB HL,出现过度闭合。手术前后ABG平均值分别为(27.0±9.1) dB HL和(9.6±9.9) dB HL,术后ABG缩小17.4 dB HL(P < 0.01);各频率ABG平均值均显著缩小。14耳(66.7%)术后ABG≤10 dB HL,18耳(85.7%)术后ABG≤20 dB HL。术后2耳(9.5%)出现感音神经性听力损失;15耳(71.4%)耳鸣和3耳(14.3%)眩晕均于术后第3天缓解。结论 激光辅助下镫骨底板开窗术治疗耳硬化症安全有效,虽然术后骨导阈值稍有提高,但不影响总体听觉康复效果。Abstract: Objective To assess the short-term efficacy of laser-assisted stapedotomy in patients with otosclerosis.Method The clinical data of twenty-one patients with otosclerosis who underwent laser-assisted stapedotomy were retrospectively analyzed. Preoperative and 3-month postoperative standardized audiometric evaluations were carried out in all patients. The occurrence of surgical complications was observed.Result The mean preoperative and postoperative air conduction (AC) thresholds were (58.2±12.7) dB HL and (43.0±23.1)dB HL respectively; the postoperative AC threshold decreased by 15.2 dB HL which was statistically significant at 0.5, 1, 2, and 4 kHz (P < 0.01). The mean preoperative and postoperative bone conduction (BC) thresholds were (31.4±10.3)dB HL and (33.3±16.6)dB HL, and there was not significant difference between them as well as BC thresholds at each frequency. Overclosure >10 dB HL was occured in 3 ears (14.3%) while sensorineural hearing loss>10 dB HL was found in 2 ears (9.5%). The mean ABG decreased by 17.4 dB HL (P < 0.01) from preoperative (27.0±9.1) dB HL to postoperative (9.6±9.9) dB HL, and the ABG at each frequency had significant decrease. Fourteen ears (66.7%) had postoperative ABG of ≤10 dB HL while 18 ears (85.7%) had postoperative ABG of ≤20 dB HL. Sensorineural hearing loss occurred in 2 ears (9.5%) after surgery, tinnitus in 15 ears (71.4%) and vertigo in 3 ears (14.3%). But all were relieved on the third day after operation.Conclusion Laser-assisted stapedotomy is a safe and effective treatment of otosclerosis. Although BC thresholds was slightly increased after surgery, it did not affect the overall hearing outcomes.
-
Key words:
- otosclerosis /
- laser /
- stapedotomy /
- treatment effectiveness
-

-
表 1 手术前后听力学检查结果
dB HL 听力学检查 术前 术后 差值 P AC平均阈值 58.2±12.7 43.0±23.1 15.2 0.006 BC平均阈值 31.4±10.3 33.3±16.6 -1.9 0.537 ABG平均值 27.0±9.1 9.6±9.9 17.4 < 0.001 表 2 手术前后不同频率AC阈值比较
dB HL 频率/kHz 术前 术后 差值 P 0.5 61.9 41.2 20.7 0.002 1 58.3 40.0 18.3 0.004 2 53.6 39.8 13.3 0.010 4 59.0 51.0 8.1 0.040 表 3 手术前后不同频率AC/BC平均阈值
dB HL 频率/ kHz 术前 术后 AC BC AC BC 0.5 61.9±10.9 23.1±10.9 41.2±25.1 28.1±16.1 1 58.3±12.3 28.6±7.1 40.0±24.2 28.8±16.5 2 53.6±15.0 39.3±14.5 39.8±22.8 36.2±19.3 4 59.0±23.3 34.8±19.2 51.0±28.7 40.2±22.8 表 4 手术前后不同频率ABG值及缩小值
dB HL 频率/kHz 术前 术后 缩小值 P 0.5 39.3 13.1 26.2 <0.0001 1 30.2 11.2 19.0 0.0002 2 14.3 3.6 10.7 0.0003 4 24.3 10.7 13.6 0.0006 -
[1] Altamami NM, Huyghues des Etages G, Fieux M, et al. Is one of these two techniques: CO2 laser versus microdrill assisted stapedotomy results in better post-operative hearing outcome?[J]. Eur Arch Otorhinolaryngol, 2019, 276(7): 1907-1913. doi: 10.1007/s00405-019-05415-7
[2] Committee on Hearing and Equilibrium guidelines for the evaluation of results of treatment of conductive hearing loss. American Academy of Otolaryngology-Head and Neck Surgery Ffoundation, Inc[J]. Otolaryngol Head Neck Surg, 1995, 113(3): 186-187. doi: 10.1016/S0194-5998(95)70103-6
[3] Khorsandi AMT, Jalali MM, Shoshi DV. Predictive factors in 995 stapes surgeries for primary otosclerosis[J]. Laryngoscope, 2018, 128(10): 2403-2407. doi: 10.1002/lary.27160
[4] Babighian GG, Albu S. Failures in stapedotomy for otosclerosis[J]. Otolaryngol Head Neck Surg, 2009, 141(3): 395-400. doi: 10.1016/j.otohns.2009.03.028
[5] Faranesh N, Magamseh E, Zaaroura S, et al. Hearing and Otoacoustic Emissions Outcome of Stapedotomy: Does the Prosthesis Diameter Matter?[J]. J Int Adv Otol, 2017, 13(2): 162-170. doi: 10.5152/iao.2017.3378
[6] de Bruijn AJ, Tange RA, Dreschler WA. Efficacy of evaluation of audiometric results after stapes surgery in otosclerosis. Ⅱ. A method for reporting results from individual cases[J]. Otolaryngol Head Neck Surg, 2001, 124(1): 84-89. doi: 10.1067/mhn.2001.111600
[7] 郝欣平, 陈树斌, 于子龙, 等. 200例耳硬化症手术患者临床特征分析[J]. 临床耳鼻咽喉头颈外科杂志, 2017, 31(20): 1545-1553. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201720001.htm
[8] Vincent R, Rovers M, Zingade N, et al. Revision stapedotomy: operative findings and hearing results. A prospective study of 652 cases from the Otology-Neurotology Database[J]. Otol Neurotol, 2010, 31(6): 875-882. doi: 10.1097/MAO.0b013e3181e8f1da
[9] Hanna KK, Abdulkhaliq E, Lana ARD. The outcome of stapedotomy in adult patients with clinical otosclerosis in Erbil[J]. Zanco J Med Sci, 2019, 23(1): 1-10. doi: 10.15218/zjms.2019.001
[10] Silverstein H, Hoffmann KK, Thompson JH Jr, et al. Hearing outcome of laser stapedotomy minus prosthesis(STAMP)versus conventional laser stapedotomy[J]. Otol Neurotol, 2004, 25(2): 106-111. doi: 10.1097/00129492-200403000-00005
[11] Redfors YD, Möller C. Otosclerosis: thirty-year follow-up after surgery[J]. Ann Otol Rhinol Laryngol, 2011, 120(9): 608-614. doi: 10.1177/000348941112000909
[12] Perez R, de Almeida J, Nedzelski JM, et al. Variations in the "Carhart notch" and overclosure after laser-assisted stapedotomy in otosclerosis[J]. Otol Neurotol, 2009, 30(8): 1033-1036. doi: 10.1097/MAO.0b013e31818edf00
[13] Wiatr A, Składzień J, Strek P, et al. Carhart Notch-A Prognostic Factor in Surgery for Otosclerosis[J]. Ear Nose Throat J, 2019. 〔Online ahead of print〕
[14] Persson P, Harder H, Magnuson B. Hearing results in otosclerosis surgery after partial stapedectomy, total stapedectomy and stapedotomy[J]. Acta Otolaryngol, 1997, 117(1): 94-99. doi: 10.3109/00016489709117998
[15] Quaranta N, Besozzi G, Fallacara RA, et al. Air and bone conduction change after stapedotomy and partial stapedectomy for otosclerosis[J]. Otolaryngol Head Neck Surg, 2005, 133(1): 116-120. doi: 10.1016/j.otohns.2005.03.011
[16] Kishimoto M, Ueda H, Uchida Y, et al. Factors affecting postoperative outcome in otosclerosis patients: Predictive role of audiological and clinical features[J]. Auris Nasus Larynx, 2015, 42(5): 369-373. doi: 10.1016/j.anl.2015.03.001
[17] Kamalski DM, Verdaasdonk RM, de Boorder T, et al. Comparing mechanical effects and sound production of KTP, thulium, and CO2 laser in stapedotomy[J]. Otol Neurotol, 2014, 35(7): 1156-1162. doi: 10.1097/MAO.0000000000000465
[18] Shiao AS, Kuo CL, Wang MC, et al. Minimally traumatic stapes surgery for otosclerosis: Risk reduction of post-operative vertigo[J]. J Chin Med Assoc, 2018, 81(6): 559-564. doi: 10.1016/j.jcma.2017.08.022
-




 下载:
下载: