-
摘要: 目的 分析锤骨前庭桥接术(MT)应用于听骨链重建的远期效果。方法 回顾性分析应用MT技术重建中耳传声功能并获得远期随访的11例(12耳)患者资料, 统计术前、术后1周和术后≥1年的听力结果, 根据术中发现、手术并发症及术后听力效果, 探讨此术式的适应证, 评估其远期安全性和有效性。结果 11例(12耳)中, 鼓室硬化1例(1耳), 先天性听骨链畸形3例(4耳), 耳硬化症5例(5耳), 局灶性中耳胆脂瘤2例(2耳)。所有患者术后2周内均无骨导听力下降(骨导损失超过10 dB); 4例术后短暂眩晕, 平均3 d缓解; 2例局灶性中耳胆脂瘤患者无复发。随访1~6年, 全部患者气导改善显著, 无骨导下降, 气骨导差术前与术后的差异有统计学意义(P < 0.05)。结论 在严格掌握手术适应证的前提下, MT远期效果安全有效, 适用于多种原因导致的伴有锤砧传声功能障碍的镫骨或底板固定的听骨链重建。Abstract: Objective To analysis the long-term outcomes of ossicular chain reconstruction using the malleostapedotomy(MT).Method A total of 11 patients(12 ears) underwent MT and their hearing levels were measured prior to surgery, 1 week and more than 1 year after surgery. The indications of MT were discussed and its safety and efficacy were evaluated in terms of the intra-operative findings, post-operative hearing and complications.Result Among 11 patients(12 ears), there were 1 patient(1 ear) with tympanosclerosis, 3 patients(4 ears) with ossicular chain deformity, 5 patients(5 ears) with otosclerosis and 2 patients(2 ears) with localized cholesteatoma of the middle ear. No cases of bone conduction hearing loss(more than 10 dB) were observed within 2 weeks after surgery while four patients suffered from short-term vertigo with an average remission duration of 3 days. And no recurrence was found in the two patients with cholesteatoma. After a follow-up of 1-6 years, we found a remarkable improvement of air conduction without bone conduction loss in all patients and there was a significant difference between preoperative and post-operative air-bone gap(P < 0.05).Conclusion With a strict selection according to the indications, MT showes safe and effective long-term outcomes and is proved to be applicable in ossicular chain reconstruction in the cases of fixation of the stapes footplate accompanied with malleus/incus mobility disorder by various causes.
-
Key words:
- malleostapedotomy /
- stapes surgery /
- otosclerosis /
- ossicular chain reconstruction /
- long-term outcome
-

-
表 1 11例(12耳)患者MT术中所见
例序 诊断 手术侧别 术中所见 术中处理 1 鼓室硬化 左 初次探查全听骨固定,鼓岬黏膜受累,底板固定;1年后二期手术发现鼓膜完整与锤骨柄连接良好,底板再固定,中耳含气 一期清除病灶,修补鼓膜,保留锤骨柄及镫骨底板;二期底板全切MT 2 听骨链畸形(马凡综合征) 左 全听骨粗大,锤砧关节活动差,镫骨底板固定 小孔窗MT 3 听骨链畸形(马凡综合征) 右 全听骨粗大,锤砧关节活动差,镫骨底板固定 小孔窗MT 4 听骨链畸形 右 镫骨底板固定,镫骨体细小,砧骨长脚短小,砧镫失连接 小孔窗MT 5 耳硬化症 左 合并锤砧关节活动差 小孔窗MT 6 耳硬化症 左 合并锤砧关节活动差 小孔窗MT 7 耳硬化症 右 合并锤砧关节活动差 小孔窗MT 8 耳硬化症 左 操作失误导致锤砧关节脱位 小孔窗MT 9 听骨链畸形 右 锤砧关节融合,板上结构及砧骨长脚缺失,面神经脱垂并遮盖前庭窗2/3,镫骨底板固定 小孔窗MT 10 耳硬化症 右 合并锤砧关节活动差 小孔窗MT 11 局灶性中耳胆脂瘤 右 鼓膜完整,中耳局限胆脂瘤上皮,破坏砧骨长脚及镫骨,清除胆脂瘤后见底板部分破坏,前庭池裸露 底板全切MT 12 局灶性中耳胆脂瘤 左 鼓膜完整,中耳局限胆脂瘤上皮,破坏砧骨长脚及镫骨,清除胆脂瘤后见底板部分破坏,前庭池裸露 底板全切MT 表 2 11例(12耳)患者术后近期、远期纯音骨导比较
例序 术前
骨导术后近期骨导
(2周内)近期骨导差
(2周内)术后远期骨导
(1年以上)远期骨导差
(1年以上)1 11 19 8 16 5 2 18 10 -8 13 -5 3 6 8 2 11 5 4 6 3 -3 15 9 5 40 41 1 39 -1 6 50 50 0 54 4 7 22 29 7 24 2 8 35 31 -4 33 -2 9 36 20 -16 20 -16 10 27 9 -18 23 -4 11 17 14 -3 22 5 12 41 40 -1 36 -5 表 3 术后远期ABG与术前ABG比较
例序 术前 远期 术前与远期ABG之差 骨导 气导 ABG 骨导 气导 ABG 1 11 55 44 16 46 35 9 2 18 67 49 13 13 -5 54 3 6 60 54 11 11 5 49 4 6 59 53 15 20 14 39 5 40 73 33 39 47 7 26 6 50 91 41 54 63 13 28 7 22 77 55 24 41 19 36 8 35 55 20 33 40 5 15 9 36 67 31 20 36 0 31 10 27 73 46 23 23 -4 50 11 17 62 45 22 41 24 21 12 41 88 47 36 51 10 37 -
[1] Fisch U, Acar GO, Huber AM. Malleostapedotomy in revision surgery for otosclerosis[J]. Otol Neurotol, 2001, 22(6): 776-785. doi: 10.1097/00129492-200111000-00011
[2] Rambousek A, Schlegel CH, Linder TE. From incus bypass to malleostapedotomy: technical improvements and results[J]. J Laryngol Otol, 2012, 126(10): 995-1002. doi: 10.1017/S0022215112002034
[3] Burggraaf J, Mylanus EAM, Pennings RJE, et al. Malleostapedotomy with the self-fixing and articulated titanium piston[J]. Eur Arch Otorhinolaryngol, 2018, 275(7): 1715-1722. doi: 10.1007/s00405-018-4999-z
[4] 吴佩娜, 葛润梅, 王正敏, 等. 锤骨-前庭桥接术在镫骨外科中的应用(附6例报告)[J]. 临床耳鼻咽喉头颈外科杂志, 2007, 21(17): 791-793. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH200717010.htm
[5] An YS, Lee KS. The surgical results of stapes fifixation in children[J]. Int J Pediatr Otorhinolaryngol, 2014, 78(1): 55-59. doi: 10.1016/j.ijporl.2013.10.043
[6] Gluth MB, Motakef S, Friedland PL, et al. Incus replacement malleostapedotomy in quiescent chronic otitis media with a mobile stapes footplate: an alternative to TORP in select cases[J]. Otol Neurotol, 2011, 32(2): 242-245. doi: 10.1097/MAO.0b013e3182015f44
[7] Kwok P, Fisch U, Nussbaumer M, et al. Morphology of the malleus handle and the comparison of different prostheses for malleostapedotomy[J]. Otol Neurotol, 2009, 30(8): 1175-1185. doi: 10.1097/MAO.0b013e31819e6361
[8] Chang MY, Jang JH, Song JJ, et al. Malleus neck-anchoring malleostapedotomy: preliminary results[J]. Otol Neurotol, 2012, 33(9): 1477-1481. doi: 10.1097/MAO.0b013e31827139b9
[9] Magliulo G, Celebrini A, Cuiuli G, et al. Malleostapedotomy in tympanosclerosis patients[J]. J Laryngol Otol, 2007, 121(12): 1148-1150. doi: 10.1017/S0022215107008766
[10] Kaftan H, Blaurock M, Kaftan S. Design-Dependent Calculation of the Prosthesis Length in Malleostapedotomy[J]. Ann Otol Rhinol Laryngol, 2015, 124(9): 728-733. doi: 10.1177/0003489415581367
[11] Iannella G, Angeletti D, Manno A, et al. Malleostapedotomy in stapes revision surgery: Is an endoscopic approach possible?[J]. Laryngoscope, 2018, 128(11): 2611-2614. doi: 10.1002/lary.27206
-

| 引用本文: | 王晓茜, 黄宏明, 葛润梅, 等. 锤骨前庭桥接术应用于听骨链重建的远期效果分析[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(10): 884-888. doi: 10.13201/j.issn.2096-7993.2020.10.005 |
| Citation: | WANG Xiaoqian, HUANG Hongming, GE Runmei, et al. The long term effect of malleostapedotomy in ossicular chain reconstruction[J]. J Clin Otorhinolaryngol Head Neck Surg, 2020, 34(10): 884-888. doi: 10.13201/j.issn.2096-7993.2020.10.005 |
- Figure 1.
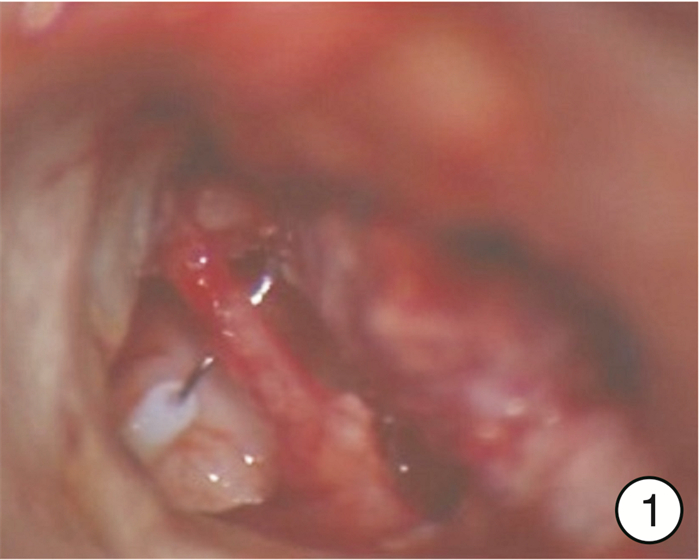
- Figure 2.



 下载:
下载: